Published online Jul 27, 2019. doi: 10.4240/wjgs.v11.i7.322
Peer-review started: April 19, 2019
First decision: June 3, 2019
Revised: June 11, 2019
Accepted: June 20, 2019
Article in press: June 21, 2019
Published online: July 27, 2019
Processing time: 102 Days and 20.5 Hours
Pancreatoduodenectomy (PD) is one of the most important operations in hepatobiliary and pancreatic surgery.
To evaluate the advantages and disadvantages of pancreaticojejunostomy (PJ) and pancreaticogastrostomy (PG).
This meta-analysis was performed using Review Manager 5.3. All clinical randomized controlled trials, in which patients underwent PD with pancreatico-digestive tract reconstruction via PJ or PG, were included.
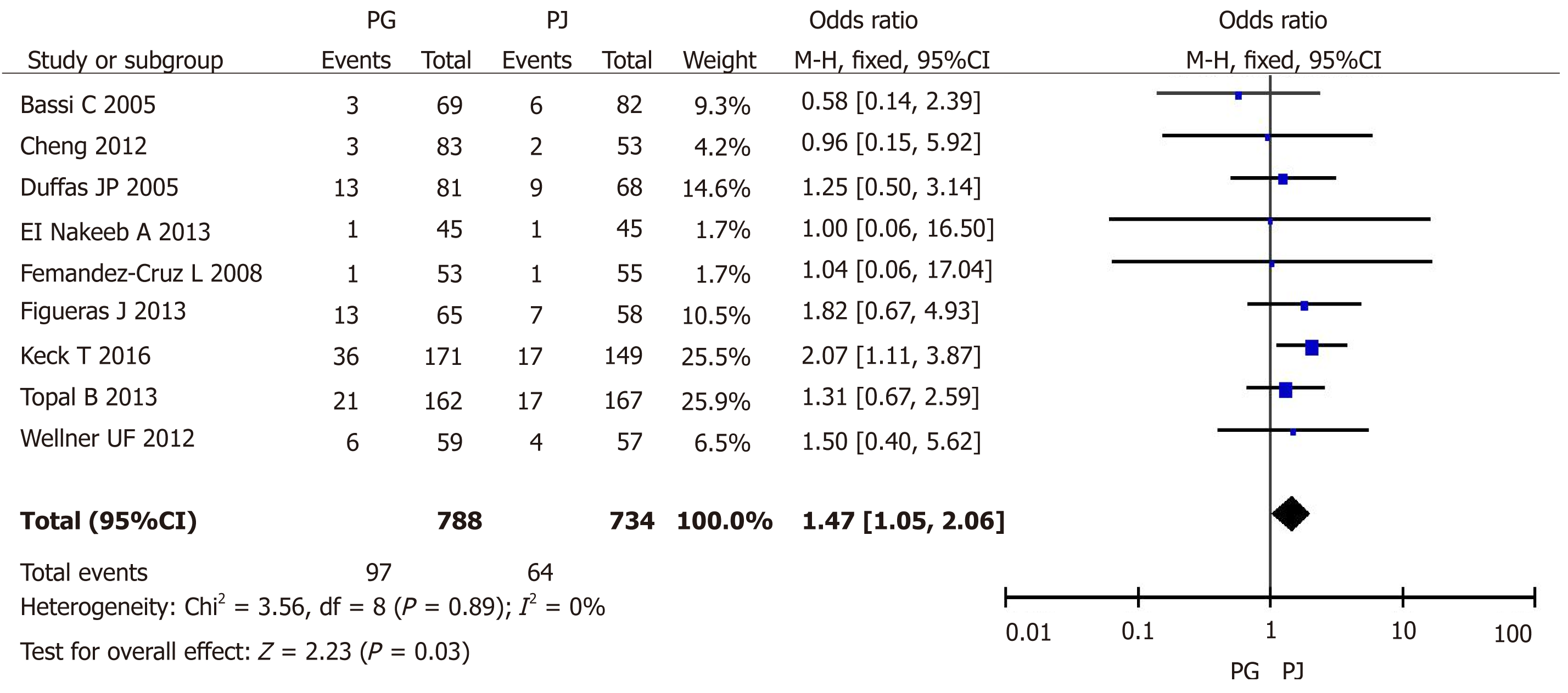
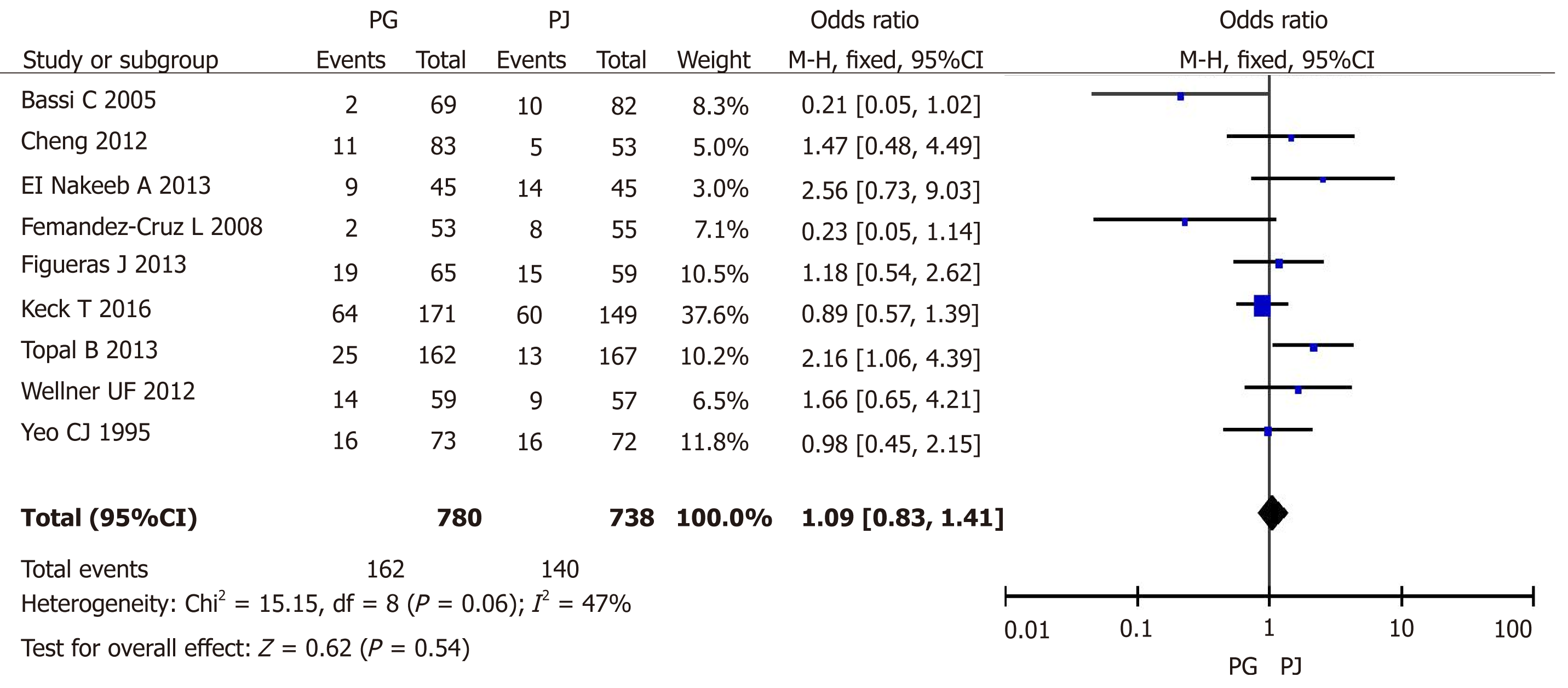
The search of PubMed, Wanfang Data, EMBASE, and the Cochrane Library provided 125 citations. After further analysis, 11 trials were included from nine counties. In all, 909 patients underwent PG and 856 underwent PJ. Meta-analysis showed that pancreatic fistula (PF) was a significantly lower morbidity in the PG group than in the PJ group (odds ratio [OR] = 0.67, 95% confidence interval [CI]: 0.53-0.86, P = 0.002); however, grades B and C PF was not significantly different between the two groups (OR = 0.61, 95%CI: 0.34-1.09, P = 0.09). Postoperative hemorrhage showed a significantly lower morbidity in the PJ group than in the PG group (OR = 1.47, 95%CI: 1.05-2.06, P = 0.03). Delayed gastric emptying was not significantly different between the two groups (OR = 1.09, 95%CI: 0.83-1.41, P = 0.54).
There is no difference in the incidence of grades B and C PF between the two groups. However, postoperative bleeding is significantly higher in PG than in PJ. Binding PJ or binding PG is a safe and secure technique according to our decades of experience.
Core tip: Pancreatico-digestive tract anastomosis after pancreaticoduodenectomy is still controversial. This systematic review and meta-analysis aimed to further evaluate the role and importance of pancreaticojejunostomy and pancreaticogastrostomy. We compared the complications of these two surgical procedures, including pancreatic fistula, delayed gastric emptying, and hemorrhage.
- Citation: Jin Y, Feng YY, Qi XG, Hao G, Yu YQ, Li JT, Peng SY. Pancreatogastrostomy vs pancreatojejunostomy after pancreaticoduodenectomy: An updated meta-analysis of RCTs and our experience. World J Gastrointest Surg 2019; 11(7): 322-332
- URL: https://www.wjgnet.com/1948-9366/full/v11/i7/322.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v11.i7.322
Pancreatoduodenectomy (PD) is the main treatment procedure for benign and malignant tumors of the pancreatic head, lower common bile duct, and ampulla[1]. The incidence of complications after PD is still high, with some large pancreatic centers reporting an incidence of approximately 10-45%[2-7]. The incidence of pancreatic fistula (PF), delayed gastric emptying (DGE), and gastrointestinal or abdominal hemorrhage has been reported to be 3-45%[8], 5%-61%[9,10], and 1%-8%[11], respectively. Other complications include abdominal empyema, incision infection, and pulmonary infection[12].
Since the establishment of PD, pancreatico-digestive tract reconstruction has been a highly valued research area, which is considered to be closely related to the success /failure of the surgery[13]. In general, pancreatico-digestive tract reconstruction includes pancreaticojejunostomy (PJ) and pancreaticogastrostomy (PG). Unlike gastrointestinal anastomosis, these two types of reconstruction after pancreatic surgery are diverse, with different results and evaluations. Therefore, there is still room for improvement in PJ and PG, and these procedures are still the focus of future research in PD.
This systematic review and meta-analysis aimed to further evaluate the role and importance of pancreatico-digestive tract anastomosis. Further, the advantages and disadvantages of PJ and PG were compared to provide a valuable reference for a more reasonable and safe choice of pancreatico-digestive tract reconstruction in the future.
All clinical randomized controlled trials, in which patients underwent PD with pancreatico-digestive tract reconstruction via PJ or PG, were included.
Studies were identified by searching electronic databases and scanning reference lists of articles. No limits were applied for languages and foreign papers were translated to English. The search was applied to Medline, Wanfang Data, EMBASE, Science Citation Index Expanded, and the Cochrane Library. The last search was run on March 15, 2019.
We used the following search terms to search all trial registers and databases: Pan-creatoduodenectomy or Pancreatoduodenectomies or Duodenopancreatectomy or Duodenopancreatectomies or Pancreaticoduodenectomy or Whipple or PD or Whipple procedure or Pancreatoduodenal resection or Pancreaticoduodenal resection, Pancreaticojejunostomy or Pancreaticojejunostomies or Pancreatojejunostomy or Pancreatojejunostomies or Pancreaticoenteric anastomosis or Pancreatoenteric anastomosis or Pancreaticojejunal anastomosis or Pancreatojejunal anastomosis or PJ, or Pancreaticogastrostomy or PG.
Eligibility assessment was performed independently in an unblinded standardized manner by two reviewers. Disagreements between reviewers were resolved by discu-ssion.
One review author extracted the following data from the included studies and the second author checked the extracted data. Disagreements were resolved by discussion between the two review authors; if no agreement could be reached, a third author would take the decision.
Data were extracted from each included trial on: (1) Characteristics of trial participants including age, disease, and number of patients; (2) Intervention with PG vs PJ; (3) Type of outcome measures including the definition and occurrence of PF, DGE, and other postoperative complications.
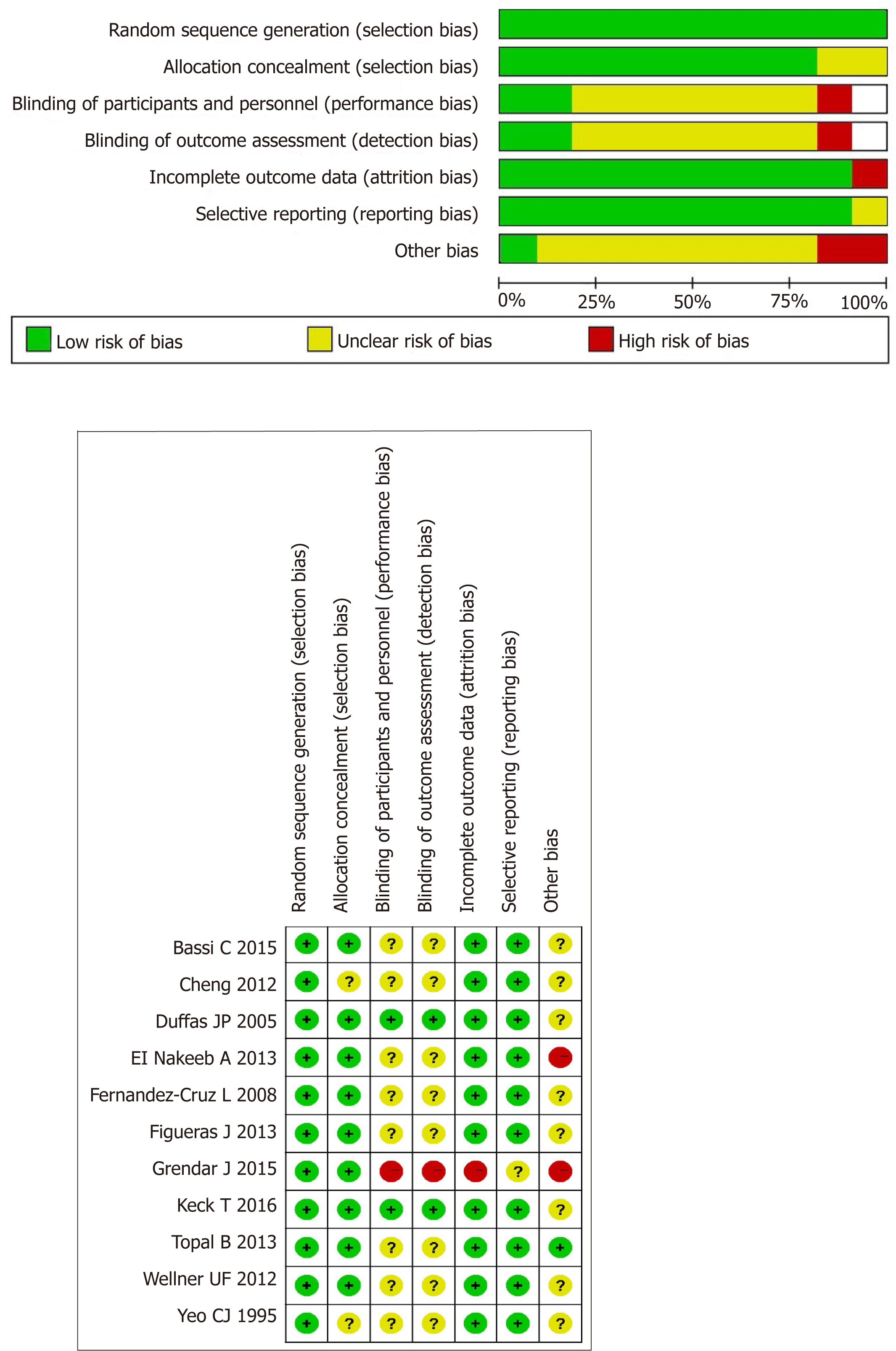
To ascertain the validity of eligible randomized trials, two independent reviewers with adequate reliability determined the adequacy of randomization, concealment of allocation, blinding of patients, healthcare providers, data collectors, and outcome assessors.
The meta-analysis was performed using Review Manager 5.3. The Chi-square test was used to test heterogeneity among studies. The heterogeneity level was judged accor-ding to I2. Relative risk (RR), weighted mean difference (WMD), standardized mean difference (SMD), and 95%CI (confidence interval) were used.
For data with clinical heterogeneity, it is not easy to merge effect quantities. First, we tested heterogeneity among studies. Then subgroup analysis or meta-regression analysis was conducted according to heterogeneity. If data were insufficient or heterogeneity cannot be found, a random-effects model was used. The homogeneity of data was tested by the χ2 test, and the homogeneity was quantitatively analyzed by the I2 test. If there was no statistical heterogeneity, a fixed-effects model was used. When statistical analysis showed heterogeneity, a random-effects model was used. The significance level of the hypothesis test was set at P < 0.05.
To assess the risk of bias across studies, we plotted the effect by the inverse of its standard error for each trial. The symmetry was assessed both visually, and formally by the Egger's test.
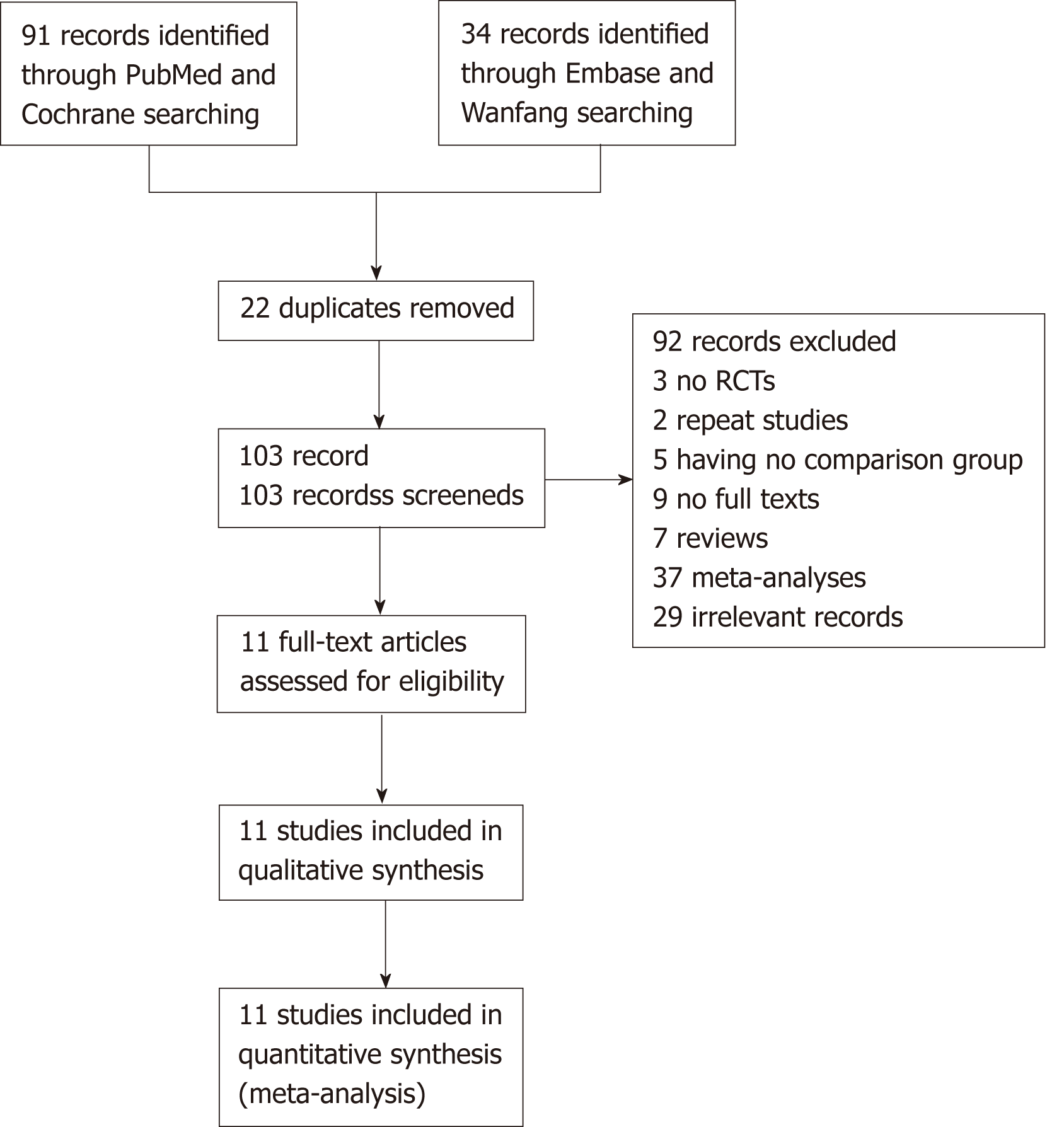
A total of 11 studies involving 11 trials were identified for inclusion in the review[14-24]. The search of PubMed, Wanfang Data, Embase, and the Cochrane Library provided 125 citations. Of the total 125 citations, 29 studies were discarded because they did not meet the inclusion criteria. Nine additional studies were discarded because full texts for these were not available. The full texts of the remaining 65 citations were exam-ined in further detail. Following this, 51 studies were found not to meet the inclusion criteria as described, and three were repeat studies from the same institute at different time points (we chose the latest study in this case). Finally, 11 studies met the inclusion criteria and were included in the systematic review. Figure 1 shows the flow diagram of study selection (Figure 1).
From 1995 to 2016, 11 trials were included from nine counties. In all, 909 patients underwent PG and 856 underwent PJ. PF was defined and classified following the International Study Group on Pancreatic Fistula (ISGPF) consensus guidelines in seven trials[15,17-22] (Table 1). The quality of these 11 trials is presented in Figure 2.
| Author | Year | Country | Study type | Number of PG | Number of PJ | Definition of PF |
| Yeo et al[14] | 1995 | United States | Single blind, controlled randomized, single center trial | 73 | 72 | PF was defined as drainage of greater than 50 mL of amylase-rid fluid on or after postoperative day 10 |
| Duffas et al[23] | 2005 | France | Single blind, controlled randomized, multicenter trial | 81 | 68 | Fluid obtained through drains or percutaneous aspiration, containing at least 4 times normal serum values of amylase for 3 day |
| Bassi et al[25] | 2005 | Italy | Single blind, controlled randomized, single center trial | 69 | 82 | Any clinically significant output of fluid, rich in amylase, confirmed by fistulography |
| Bassi et al[8] | 2008 | Spain | Single blind, controlled randomized, single center trial | 53 | 55 | ISGPF definition |
| Wellner et al[15] | 2012 | Germany | Single blind, controlled randomized, single center trial | 59 | 57 | ISGPF definition |
| Wang et al[30] | 2012 | China | Single blind, controlled randomized, multicenter trial | 83 | 53 | ISGPF definition |
| El Nakeeb et al[20] | 2013 | Egypt | Single blind, controlled randomized, single center trial | 45 | 45 | ISGPF definition |
| Topal et al[18] | 2013 | Belgium | Single blind, controlled randomized, multicenter trial | 162 | 167 | ISGPF definition |
| Figueras et al[22] | 2013 | Spain | Single blind, controlled randomized, multicenter trial | 65 | 58 | ISGPF definition |
| Grendar et al[24] | 2015 | Canada | Single blind, controlled randomized, single center trial | 48 | 50 | Either radiologically proven anastomotic leak or continued drainage (via drain, enterocutaneous fistula, or wound) of lipaserich fluid on postoperative day 10 |
| Keck et al[19] | 2016 | Germany | Single blind, controlled randomized, multicenter trial | 171 | 149 | ISGPF definition |
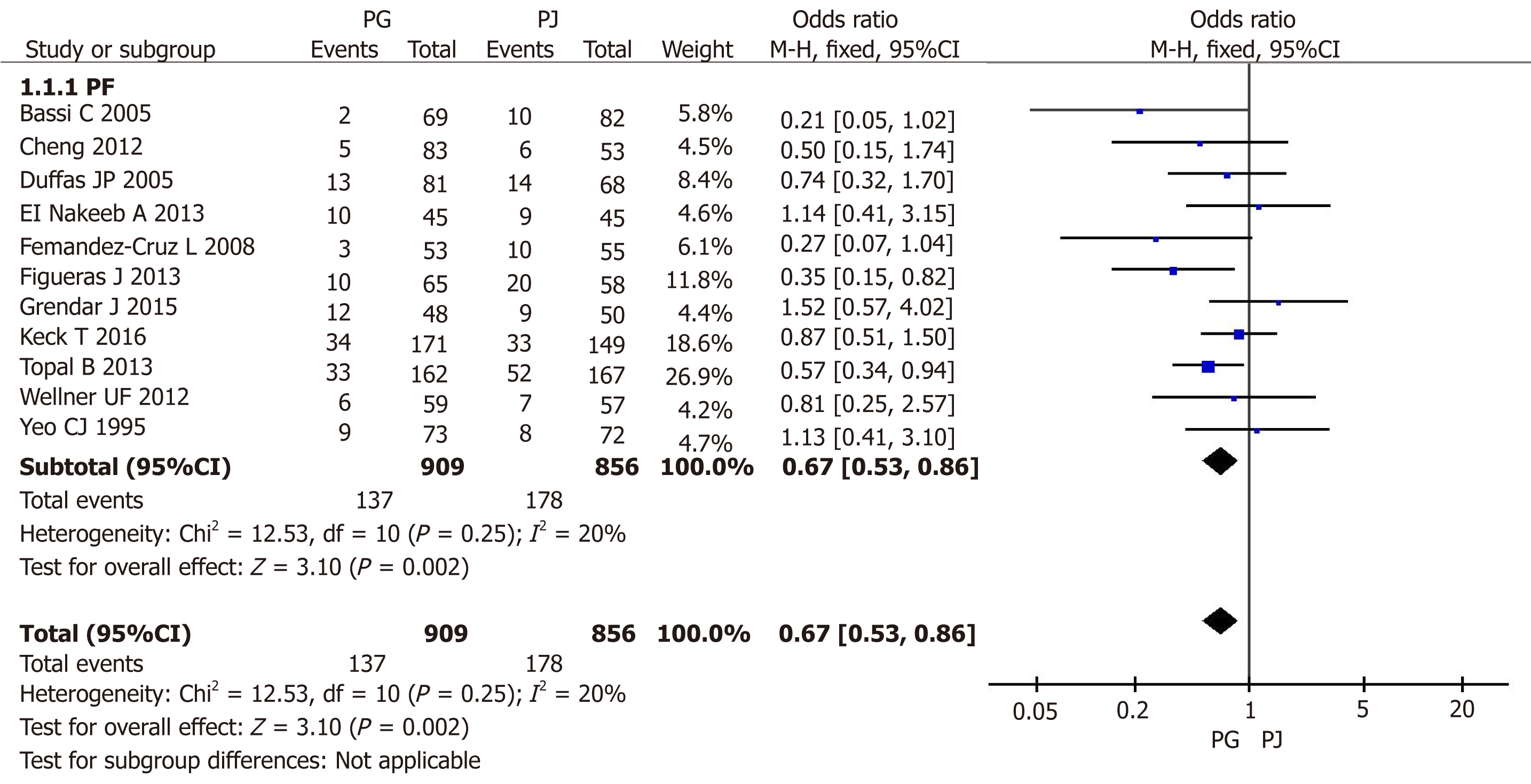
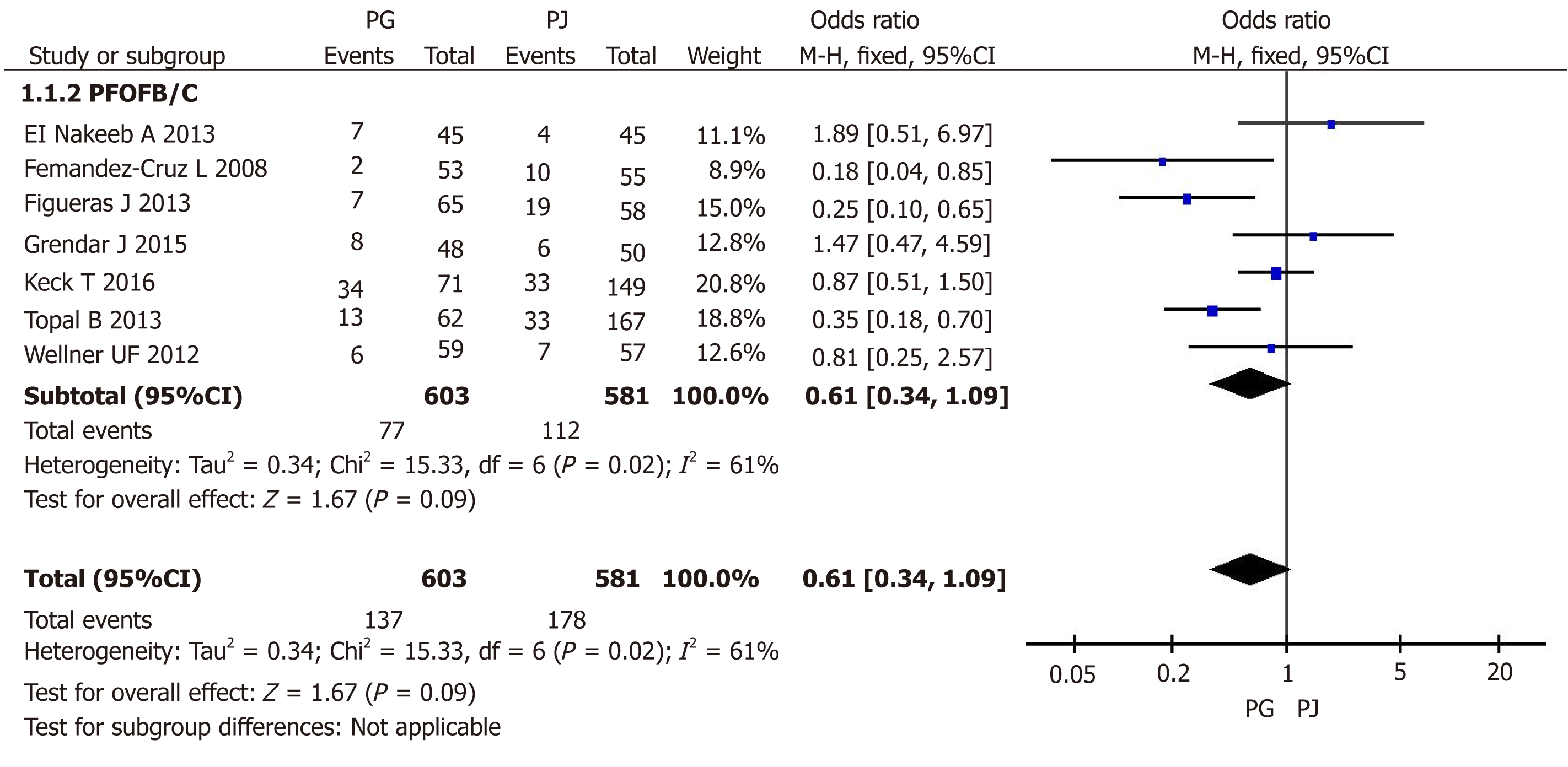
PF data were available for all 11 trials randomizing 1765 patients and reporting data for them. In the meta-analysis, there was no significant hetero-geneity between these studies (I2 = 20%); therefore, a fixed-effects model was applied. PF showed a significantly lower morbidity in the PG group than in the PJ group (odds ratio [OR] = 0.67, 95%CI: 0.53-0.86, P = 0.002) (Figure 3). Grade A PF did not affect the disease outcome; therefore, we further analyzed the incidence of grades B and C PF. Seven trials with 603 PG and 581 PJ patients were included. In the meta-analysis, there was a significant difference in heterogeneity between these studies (I2 = 61%); accordingly, a random-effects model was applied. Grades B and C PF was not significantly different between the two groups (OR = 0.61, 95%CI: 0.34-1.09, P = 0.09) (Figure 4).
Nine trials with 788 PG and 734 PJ patients were included for analyzing postoperative hemorrhage. In the meta-analysis, there was no significant hetero-geneity between these studies (I2 = 0%); accordingly, a fixed-effects model was applied. Postoperative hemorrhage showed a significantly lower morbidity in the PJ group than in the PG group (OR = 1.47, 95%CI: 1.05-2.06, P = 0.03) (Figure 5).
Nine trials including 780 PG and 738 PJ patients were included for the analysis of DGE. In the meta-analysis, there was no significant heterogeneity between these studies (I2 = 47%), and therefore a fixed-effects model was applied. DGE was not significantly different between the two groups (OR = 1.09, 95%CI: 0.83-1.41, P = 0.54) (Figure 6).
PF is one of the most common complications after PD. PF not only causes serious complications such as abdominal bleeding but also increases the length of hospital stay and cost for patients. Our study showed that PG anastomosis can reduce the incidence of all grades of PF than PJ anastomosis. In 2005, the ISGPF defined PF and divided it into three levels[25]. In 2016, the group adjusted the classification of PF and defined grade A PF as a biochemical fistula[8]. Therefore, in this study, we considered the incidence of grades B/C PF in subgroup analysis. We believe that this statistical analysis has more clinical value and significance. We found no statistical difference in grades B/C PF between the two groups (PJ and PG). However, our result showed that PG anastomosis may increase the incidence of bleeding compared with PJ anasto-mosis.
Our group has studied the anastomosis of the pancreas and digestive tract for more than 20 years, and has accumulated some experiences[7,26,27]. In 1996, we established the binding pancreaticojejunostomy (BPJ). The main feature of this surgery is that the anastomosis between the jejunum and pancreas is mainly made with a binding line. It avoids the needle hole penetrating the intestinal cavity on the surface of the anastomotic site, thus preventing the leakage of pancreatic juice from the pinholes, to fundamentally eliminate the possibility of PF. At present, BPJ has been applied in more than a thousand of cases, which has a significant effect on the prevention of PF after surgery[7]. In 2010, Buc, a French scholar, named BPJ procedure as Peng's PJ and reported that BPJ was a safe and secure technique[28]. In 2008, Peng created the binding pancreaticogastrostomy (BPG), which simplified the operation steps of the previous pancreas-stomach anastomosis[29]. After continuous improvement, only the bundled method was used in the posterior wall of the stomach, avoiding the suture of pancreas parenchyma and thus greatly shortening the surgical time and preventing anasto-motic leakage. BPG not only solves the problem of excessive pancreatic stump but also reduces the harm of bile leakage because the biliary-enteric anastomosis is not in the same channel as PG anastomosis[27]. The mid-term results of the randomized controlled study showed that the incidence of PF in BPG and BPJ was acceptable[17].
In recent years, with the continuous development of laparoscopic technology, laparoscopic PD has gradually become an alternative method, used as a routine treatment in some pancreatic surgeries[30-32]. Thus, laparoscopic pancreatico-gastrointestinal anastomosis has become a new focus for research. Owing to the limitation of the laparoscopic visual field, pancreatic duct to mucosa anastomosis is the first choice of procedure under laparoscopy[30].
The attempt of various methods makes the technique of PJ dazzling. However, the basic content cannot be separated from pancreas-jejunum (stomach) anastomosis or pancreatic duct-jejunum (stomach) anastomosis. The objective of evaluation should be as simple as possible. Moreover, the lower the incidence of pancreatic leakage compared with classical anastomosis, the better. As long as these principles are followed, sample enlargement and randomized controlled trials should be conducted to find the best method.
Pancreatoduodenectomy (PD) is one of the most important operations in hepatobiliary and pancreatic surgery. Pancreatico-digestive tract reconstruction includes pancreaticojejunostomy (PJ) and pancreaticogastrostomy (PG). Unlike gastrointestinal anastomosis, these two types of reconstruction after pancreatic surgery are diverse, with different results and evaluations. Therefore, there is still room for improvement in PJ and PG, and these procedures are still the focus of future research in PD.
This systematic and meta-analysis aimed to evaluate the role and importance of pancreatico-digestive tract anastomosis. Advantages and disadvantages of PJ and PG were compared to provide a valuable reference and safe choice in the future.
This search was applied to Medline, Wanfang Data, Embase, Science Citation Index Expanded, and the Cochrane Library. The last search was run on March 15, 2019. All clinical randomized controlled trials, in which patients underwent PD with pancreatico-digestive tract reconstruction via PJ or PG, were included. The Chi-square test was used to test heterogeneity among studies. The heterogeneity level was judged according to I2. Relative risk (RR), weighted mean difference (WMD), standardized mean difference (SMD), and 95%CI were used.
In the meta-analysis of postoperative hemorrhage, there was no significant heterogeneity between these studies (I2 = 0%); accordingly, a fixed-effect model was applied. Postoperative hemorrhage showed a significantly lower morbidity in the PJ group than in the PG group (OR = 1.47, 95%CI: 1.05-2.06, P = 0.03). In the meta-analysis of DGE, there was no significant heterogeneity between these studies (I2 = 47%), and therefore a fixed-effects model was applied. DGE was not significantly different between the two groups (OR = 1.09, 95%CI: 0.83-1.41, P = 0.54).
Our group has studied the anastomosis of the pancreas and digestive tract for more than 20 years, and has accumulated some experiences. We established the binding pancreaticoje-junostomy (BPJ) and binding pancreaticogastrostomy (BPG). The mid-term results of the randomized controlled study showed that the incidence of PF in BPG and BPJ was acceptable.
Laparoscopic pancreaticogastrointestinal anastomosis has become a new focus for research. The objective of evaluation should be as simple as possible. Moreover, the lower the incidence of pancreatic leakage compared with classical anastomosis, the better. As long as these principles are followed, sample enlargement and randomized controlled trials should be conducted to find the best method.
| 1. | Whipple AO, Parsons WB, Mullins CR. TREATMENT OF CARCINOMA OF THE AMPULLA OF VATER. Ann Surg. 1935;102:763-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 882] [Cited by in RCA: 909] [Article Influence: 47.8] [Reference Citation Analysis (0)] |
| 2. | Giuliano K, Ejaz A, He J. Technical aspects of pancreaticoduodenectomy and their outcomes. Chin Clin Oncol. 2017;6:64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | McMillan MT, Allegrini V, Asbun HJ, Ball CG, Bassi C, Beane JD, Behrman SW, Berger AC, Bloomston M, Callery MP, Christein JD, Dickson E, Dixon E, Drebin JA, Fernandez-Del Castillo C, Fisher WE, Fong ZV, Haverick E, Hollis RH, House MG, Hughes SJ, Jamieson NB, Kent TS, Kowalsky SJ, Kunstman JW, Malleo G, McElhany AL, Salem RR, Soares KC, Sprys MH, Valero V, Watkins AA, Wolfgang CL, Zureikat AH, Vollmer CM. Incorporation of Procedure-specific Risk Into the ACS-NSQIP Surgical Risk Calculator Improves the Prediction of Morbidity and Mortality After Pancreatoduodenectomy. Ann Surg. 2017;265:978-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 79] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 4. | Reyna-Sepúlveda F, Muñoz-Maldonado G, Pérez-Rodríguez E, Hernández-Trejo F, Guevara-Charles A, Hernández-Guedea M. Prognostic factors for survival and surgical complications in Whipple's pancreatoduodenectomy during a 10-year experience. Cir Cir. 2019;87:205-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Brown EG, Yang A, Canter RJ, Bold RJ. Outcomes of pancreaticoduodenectomy: where should we focus our efforts on improving outcomes? JAMA Surg. 2014;149:694-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 6. | Büchler MW, Wagner M, Schmied BM, Uhl W, Friess H, Z'graggen K. Changes in morbidity after pancreatic resection: toward the end of completion pancreatectomy. Arch Surg. 2003;138:1310-4; discussion 1315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 433] [Cited by in RCA: 452] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 7. | Peng SY, Wang JW, Lau WY, Cai XJ, Mou YP, Liu YB, Li JT. Conventional versus binding pancreaticojejunostomy after pancreaticoduodenectomy: a prospective randomized trial. Ann Surg. 2007;245:692-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 182] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 8. | Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, Conlon K, Del Chiaro M, Falconi M, Fernandez-Cruz L, Fernandez-Del Castillo C, Fingerhut A, Friess H, Gouma DJ, Hackert T, Izbicki J, Lillemoe KD, Neoptolemos JP, Olah A, Schulick R, Shrikhande SV, Takada T, Takaori K, Traverso W, Vollmer CR, Wolfgang CL, Yeo CJ, Salvia R, Buchler M; International Study Group on Pancreatic Surgery (ISGPS). The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery. 2017;161:584-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3041] [Cited by in RCA: 3201] [Article Influence: 355.7] [Reference Citation Analysis (35)] |
| 9. | Eisenberg JD, Rosato EL, Lavu H, Yeo CJ, Winter JM. Delayed Gastric Emptying After Pancreaticoduodenectomy: an Analysis of Risk Factors and Cost. J Gastrointest Surg. 2015;19:1572-1580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 73] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 10. | Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Büchler MW. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1771] [Cited by in RCA: 2451] [Article Influence: 129.0] [Reference Citation Analysis (0)] |
| 11. | Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Büchler MW. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142:20-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1411] [Cited by in RCA: 2064] [Article Influence: 108.6] [Reference Citation Analysis (0)] |
| 12. | Lessing Y, Pencovich N, Nevo N, Lubezky N, Goykhman Y, Nakache R, Lahat G, Klausner JM, Nachmany I. Early reoperation following pancreaticoduodenectomy: impact on morbidity, mortality, and long-term survival. World J Surg Oncol. 2019;17:26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Cameron JL, He J. Two thousand consecutive pancreaticoduodenectomies. J Am Coll Surg. 2015;220:530-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 456] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 14. | Yeo CJ, Cameron JL, Maher MM, Sauter PK, Zahurak ML, Talamini MA, Lillemoe KD, Pitt HA. A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg. 1995;222:580-588; discussion 588-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 530] [Cited by in RCA: 525] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 15. | Wellner UF, Sick O, Olschewski M, Adam U, Hopt UT, Keck T. Randomized controlled single-center trial comparing pancreatogastrostomy versus pancreaticojejunostomy after partial pancreatoduodenectomy. J Gastrointest Surg. 2012;16:1686-1695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 86] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 16. | Bassi C, Falconi M, Molinari E, Salvia R, Butturini G, Sartori N, Mantovani W, Pederzoli P. Reconstruction by pancreaticojejunostomy versus pancreaticogastrostomy following pancreatectomy: results of a comparative study. Ann Surg. 2005;242:767-771, discussion 771; 773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 340] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 17. | Jian C. Comparsion of clinical effect between Binding Pancreaticojejunostomy and Binding Pancreaticogastrostomy-Multi-center Prospective Randomized Controlled Trial Study (Mid-term Data Analysis). Medical college of Zhejiang University. 2012;. |
| 18. | Topal B, Fieuws S, Aerts R, Weerts J, Feryn T, Roeyen G, Bertrand C, Hubert C, Janssens M, Closset J; Belgian Section of Hepatobiliary and Pancreatic Surgery. Pancreaticojejunostomy versus pancreaticogastrostomy reconstruction after pancreaticoduodenectomy for pancreatic or periampullary tumours: a multicentre randomised trial. Lancet Oncol. 2013;14:655-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 221] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 19. | Keck T, Wellner UF, Bahra M, Klein F, Sick O, Niedergethmann M, Wilhelm TJ, Farkas SA, Börner T, Bruns C, Kleespies A, Kleeff J, Mihaljevic AL, Uhl W, Chromik A, Fendrich V, Heeger K, Padberg W, Hecker A, Neumann UP, Junge K, Kalff JC, Glowka TR, Werner J, Knebel P, Piso P, Mayr M, Izbicki J, Vashist Y, Bronsert P, Bruckner T, Limprecht R, Diener MK, Rossion I, Wegener I, Hopt UT. Pancreatogastrostomy Versus Pancreatojejunostomy for RECOnstruction After PANCreatoduodenectomy (RECOPANC, DRKS 00000767): Perioperative and Long-term Results of a Multicenter Randomized Controlled Trial. Ann Surg. 2016;263:440-449. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 195] [Cited by in RCA: 248] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 20. | El Nakeeb A, Hamdy E, Sultan AM, Salah T, Askr W, Ezzat H, Said M, Zeied MA, Abdallah T. Isolated Roux loop pancreaticojejunostomy versus pancreaticogastrostomy after pancreaticoduodenectomy: a prospective randomized study. HPB (Oxford). 2014;16:713-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 83] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 21. | Fernández-Cruz L, Cosa R, Blanco L, López-Boado MA, Astudillo E. Pancreatogastrostomy with gastric partition after pylorus-preserving pancreatoduodenectomy versus conventional pancreatojejunostomy: a prospective randomized study. Ann Surg. 2008;248:930-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 152] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 22. | Figueras J, Sabater L, Planellas P, Muñoz-Forner E, Lopez-Ben S, Falgueras L, Sala-Palau C, Albiol M, Ortega-Serrano J, Castro-Gutierrez E. Randomized clinical trial of pancreaticogastrostomy versus pancreaticojejunostomy on the rate and severity of pancreatic fistula after pancreaticoduodenectomy. Br J Surg. 2013;100:1597-1605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 142] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 23. | Duffas JP, Suc B, Msika S, Fourtanier G, Muscari F, Hay JM, Fingerhut A, Millat B, Radovanowic A, Fagniez PL; French Associations for Research in Surgery. A controlled randomized multicenter trial of pancreatogastrostomy or pancreatojejunostomy after pancreatoduodenectomy. Am J Surg. 2005;189:720-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 219] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 24. | Grendar J, Ouellet JF, Sutherland FR, Bathe OF, Ball CG, Dixon E. In search of the best reconstructive technique after pancreaticoduodenectomy: pancreaticojejunostomy versus pancreaticogastrostomy. Can J Surg. 2015;58:154-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 25. | Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M; International Study Group on Pancreatic Fistula Definition. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3282] [Cited by in RCA: 3551] [Article Influence: 169.1] [Reference Citation Analysis (35)] |
| 26. | Peng SY, Wang JW, Li JT, Mou YP, Liu YB, Cai XJ. Binding pancreaticojejunostomy--a safe and reliable anastomosis procedure. HPB (Oxford). 2004;6:154-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 27. | Peng SY, Wang JW, Hong DF, Liu YB, Wang YF. Binding pancreaticoenteric anastomosis: from binding pancreaticojejunostomy to binding pancreaticogastrostomy. Updates Surg. 2011;63:69-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 28. | Buc E, Flamein R, Golffier C, Dubois A, Nagarajan G, Futier E, Pezet D. Peng's binding pancreaticojejunostomy after pancreaticoduodenectomy: a French prospective study. J Gastrointest Surg. 2010;14:705-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 29. | Peng SY, Hong DF, Liu YB, Tan ZJ, Li JT, Tao F. [Binding pancreaticogastrostomy]. Zhonghua Wai Ke Za Zhi. 2009;47:139-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 30. | Wang M, Peng B, Liu J, Yin X, Tan Z, Liu R, Hong D, Zhao W, Wu H, Chen R, Li D, Huang H, Miao Y, Liu Y, Liang T, Wang W, Cai Y, Xing Z, Cheng W, Zhong X, Zhao Z, Zhang J, Yang Z, Li G, Shao Y, Lin G, Jiang K, Wu P, Jia B, Ma T, Jiang C, Peng S, Qin R. Practice Patterns and Perioperative Outcomes of Laparoscopic Pancreaticoduodenectomy in China: A Retrospective Multicenter Analysis of 1029 Patients. Ann Surg. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 114] [Article Influence: 22.8] [Reference Citation Analysis (1)] |
| 31. | Palanivelu C, Jani K, Senthilnathan P, Parthasarathi R, Rajapandian S, Madhankumar MV. Laparoscopic pancreaticoduodenectomy: technique and outcomes. J Am Coll Surg. 2007;205:222-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 178] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 32. | Kendrick ML, van Hilst J, Boggi U, de Rooij T, Walsh RM, Zeh HJ, Hughes SJ, Nakamura Y, Vollmer CM, Kooby DA, Asbun HJ; Minimally Invasive Pancreatic Resection Organizing Committee. Minimally invasive pancreatoduodenectomy. HPB (Oxford). 2017;19:215-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 68] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
PRISMA2009 Checklist statement: PRISMA2009 Checklist has been adopted.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Invited Manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Aoki H, Bandyopadhyay SK, Uhlmann D S-Editor: Cui LJ L-Editor: Wang TQ E-Editor: Wang J