©2010 Baishideng Publishing Group Co.
World J Gastrointest Surg. Oct 27, 2010; 2(10): 331-336
Published online Oct 27, 2010. doi: 10.4240/wjgs.v2.i10.331
Published online Oct 27, 2010. doi: 10.4240/wjgs.v2.i10.331
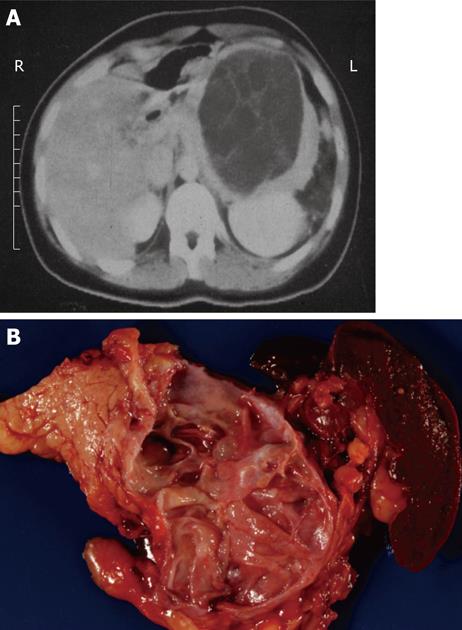
Figure 1 Typical computed tomography (A) and gross (B) appearance of a mucinous cystic neoplasm showing the distal location and the lack of communication with the duct, respectively.
Figure 2 Typical computed tomography (A) and gross (B) appearance of a small pancreatic pseudocyst showing the typical spheroid shape, unilocularity, and necrotic debris contents.
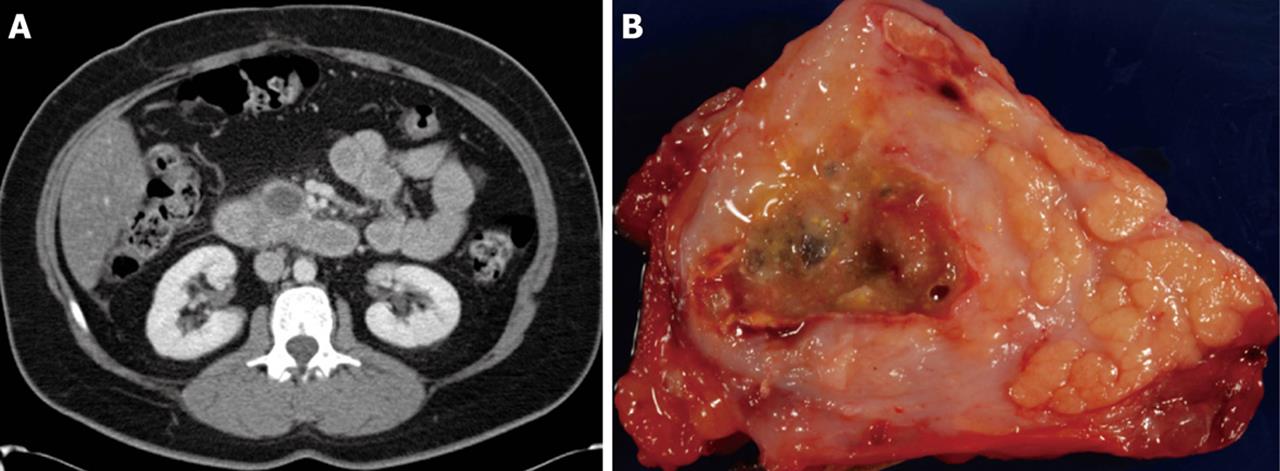
Figure 3 Typical computed tomography (A) and gross (B) appearance of a solid pseudopapillary neoplasm showing the typical ovoid shape and necrotic debris contents.
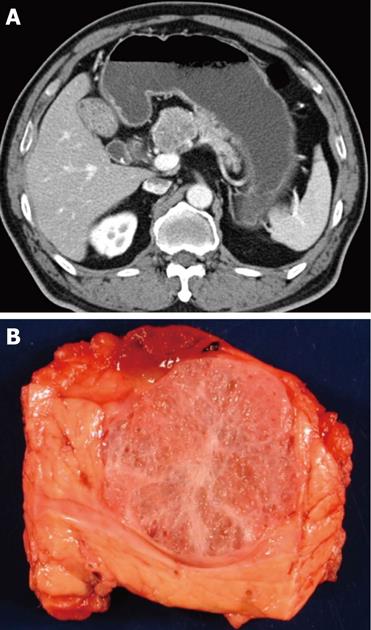
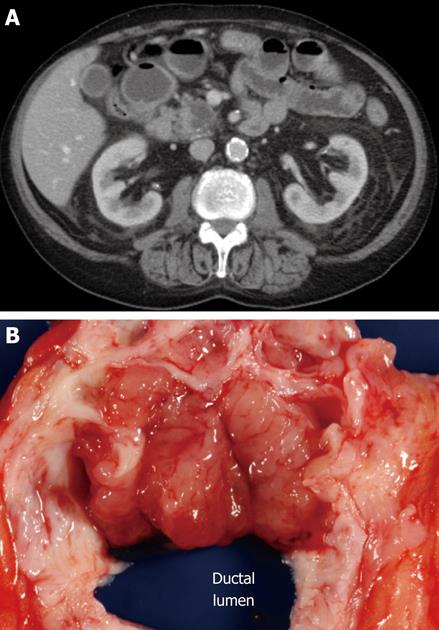
Figure 4 Typical computed tomography (A) and gross (B) appearance of a serous cystadenoma showing the honeycomb appearance.
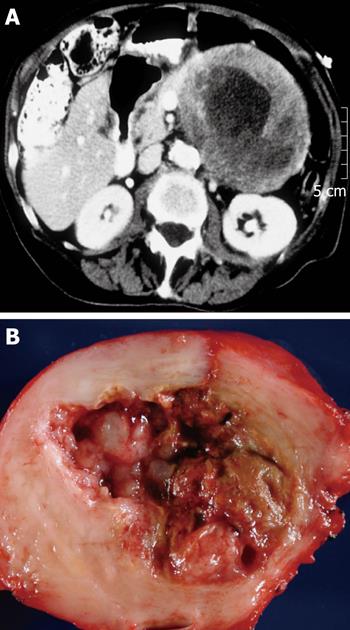
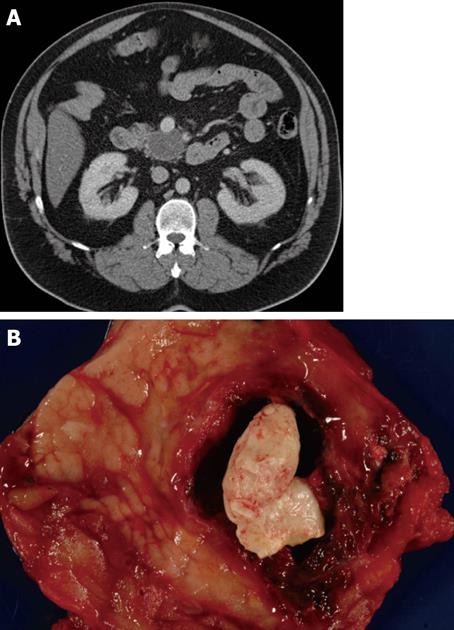
Figure 5 Typical computed tomography (A) and gross (B) appearance of a cystic neuroendocrine tumor showing the spherical shape and the occasionally seen calcification.
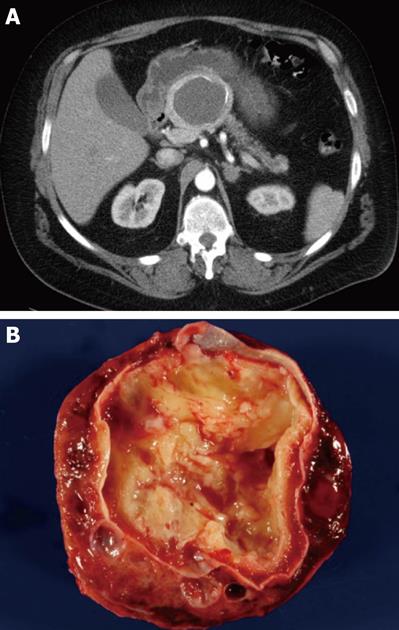
Figure 6 Typical computed tomography (A) and gross (B) appearance of an intraductal papillary mucinous neoplasm showing the ovoid shape and communication with the duct, respectively.
Figure 7 Typical computed tomography (A) and gross (B) appearance of a lymphoepithelial cyst showing the typical ovoid shape, peripheral location, and proteinaceous concretions (not always present on computed tomography imaging).
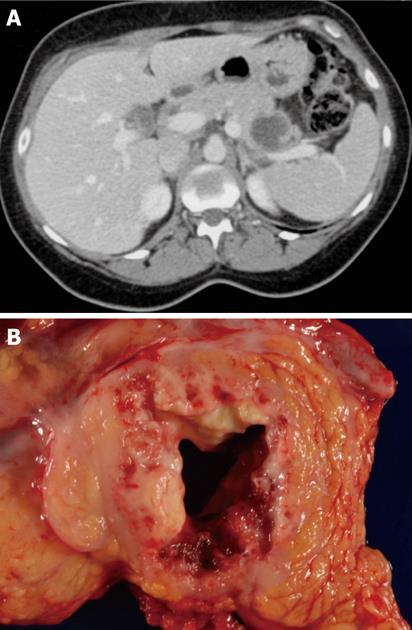
Figure 8 Typical computed tomography (A) and gross (B) appearance of an invasive carcinoma with cystic degeneration.
- Citation: Cunningham SC, Hruban RH, Schulick RD. Differentiating intraductal papillary mucinous neoplasms from other pancreatic cystic lesions. World J Gastrointest Surg 2010; 2(10): 331-336
- URL: https://www.wjgnet.com/1948-9366/full/v2/i10/331.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v2.i10.331