©The Author(s) 2026.
World J Gastrointest Surg. Jan 27, 2026; 18(1): 112416
Published online Jan 27, 2026. doi: 10.4240/wjgs.v18.i1.112416
Published online Jan 27, 2026. doi: 10.4240/wjgs.v18.i1.112416
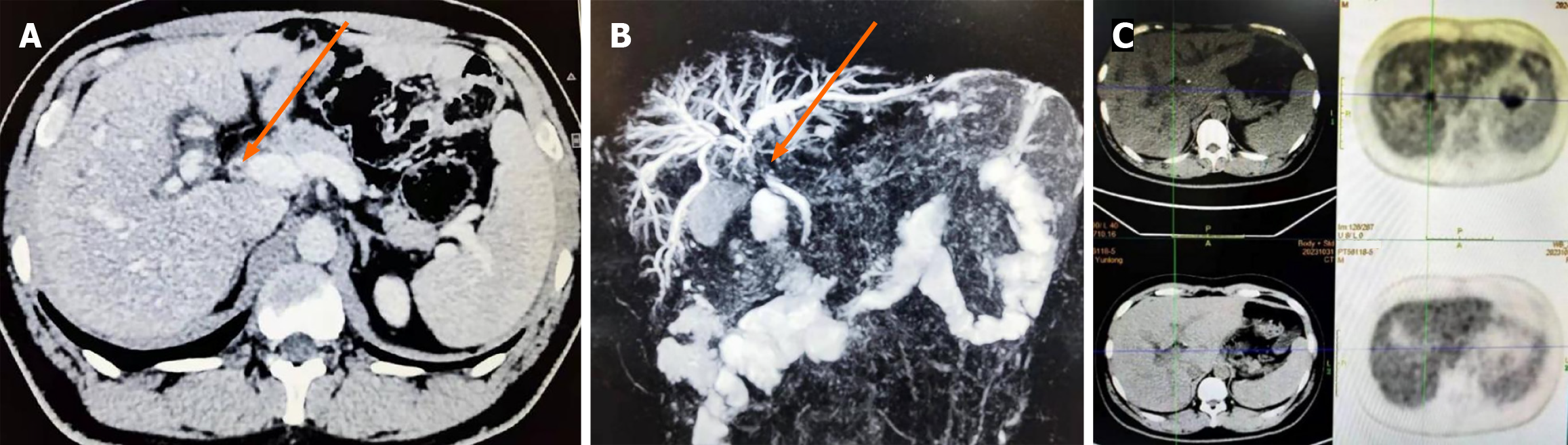
Figure 1 Imaging examinations.
A: Contrast-enhanced computed tomography suggested thickening of the cystic duct walls, common hepatic duct, and proximal common bile duct; B: Magnetic resonance cholangiopancreatography suggested partial dilatation of intrahepatic bile duct as well as stenosis of common hepatic duct and common bile duct; C: Positron emission tomography/computed tomography suggested nodular-like foci of metabolic increased in the area of biliary tracts of the hepatic hilar region. Orange arrow: The stenosis of common bile duct.
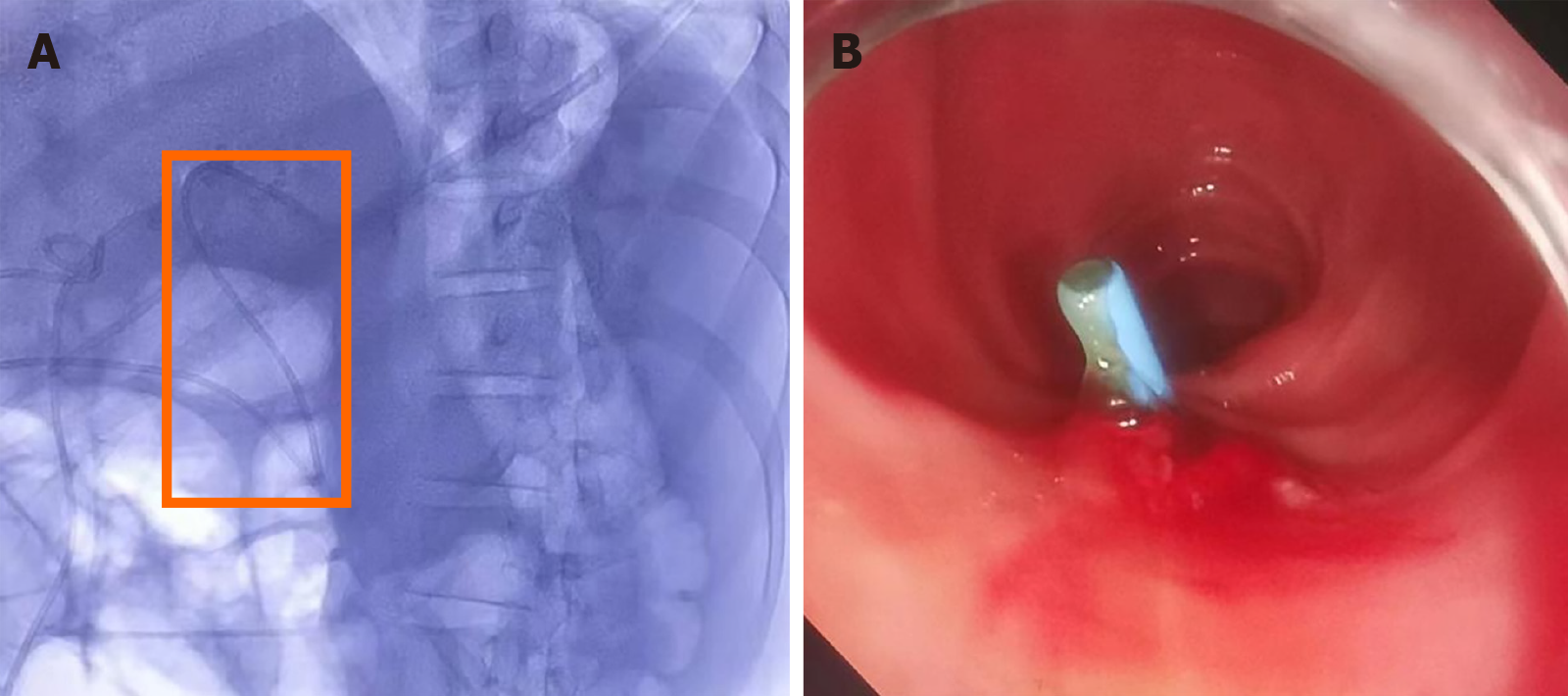
Figure 2 Endoscopic retrograde cholangiopancreatography combined with choledochoscopy.
Orange arrow: A stenosis with reddened and slightly rough mucosa at the upper section of the common bile duct.
Figure 3 Placement of a plastic biliary stent across the stenosis.
A: The anterior end of the stent (8.5 Fr diameter, 15 cm length) was positioned within the left hepatic duct; B: The terminal end of the stent terminates was positioned within the duodenum. Orange box: A stent in the left hepatic duct.
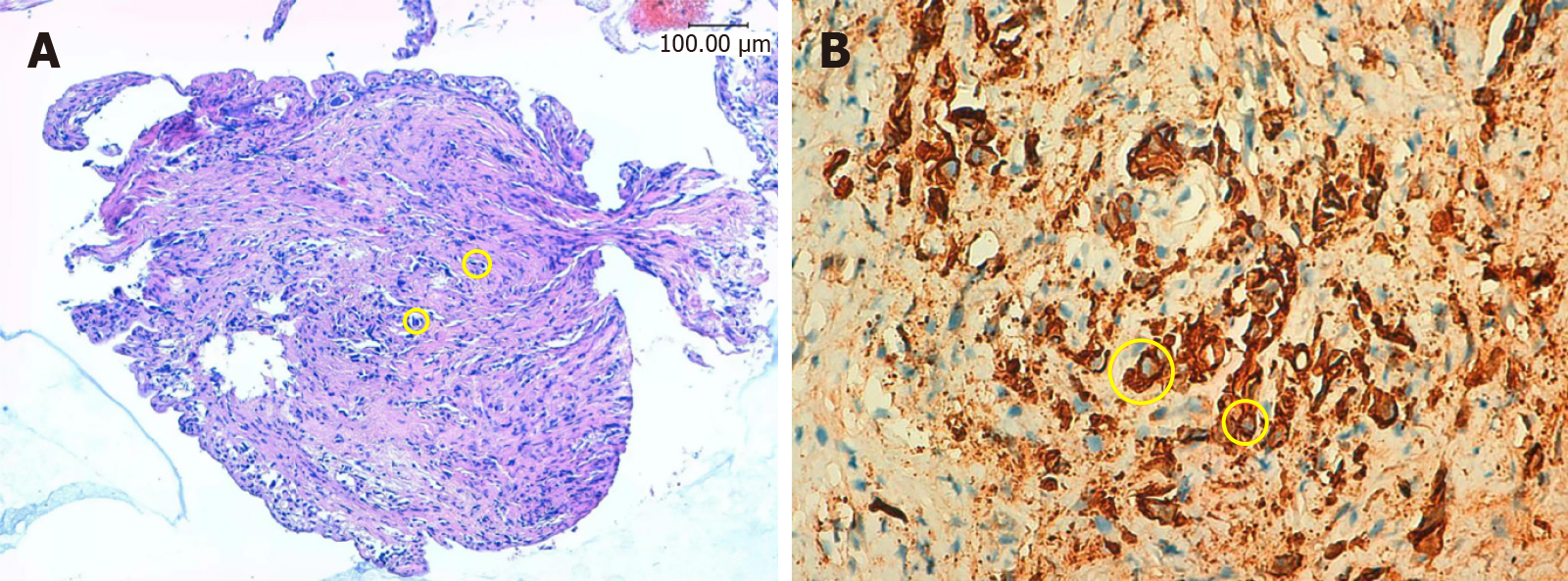
Figure 4 Pathological examination of the stenosis locating at the upper section of the common bile duct.
A: Hematoxylin and eosin showed clusters of heterogeneous cells beneath the mucosal layer, suggesting poorly differentiated adenocarcinoma; B: Immunohistochemical staining showed cytokeratin (+). Yellow circle: Poorly differentiated adenocarcinoma cells.
- Citation: Li CK, Cao RR, Su DS, Ming J, Li YC, Shao XD, Qi XS. Diagnosis of bile duct metastasis from gastric cancer by endoscopic retrograde cholangiopancreatography combined with choledochoscopy: A case report. World J Gastrointest Surg 2026; 18(1): 112416
- URL: https://www.wjgnet.com/1948-9366/full/v18/i1/112416.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v18.i1.112416