©The Author(s) 2025.
World J Gastrointest Surg. Jul 27, 2025; 17(7): 105925
Published online Jul 27, 2025. doi: 10.4240/wjgs.v17.i7.105925
Published online Jul 27, 2025. doi: 10.4240/wjgs.v17.i7.105925
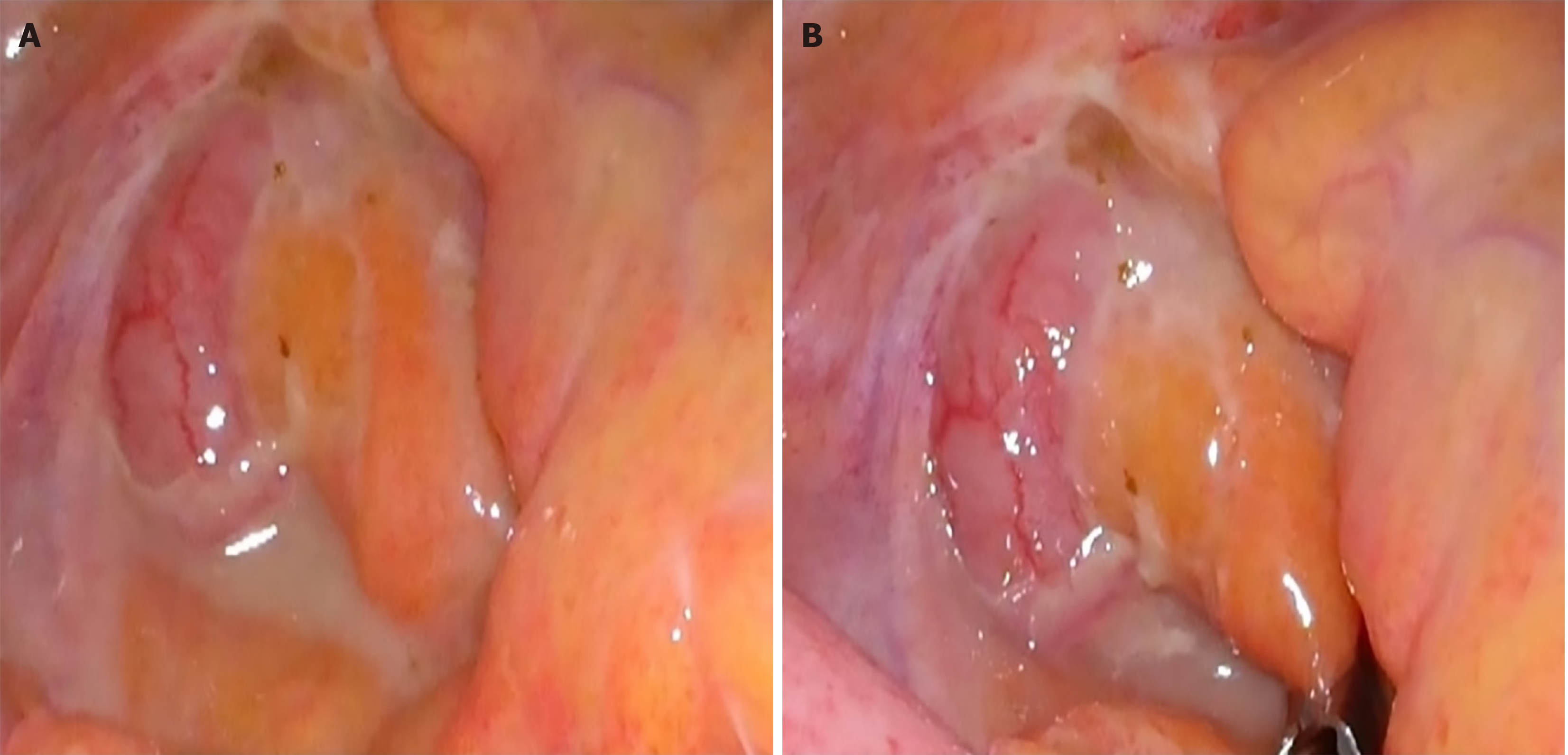
Figure 1 Acute appendicitis located in retrocecal position.
This figure is generated based on a case performed at Konyang University Hospital.
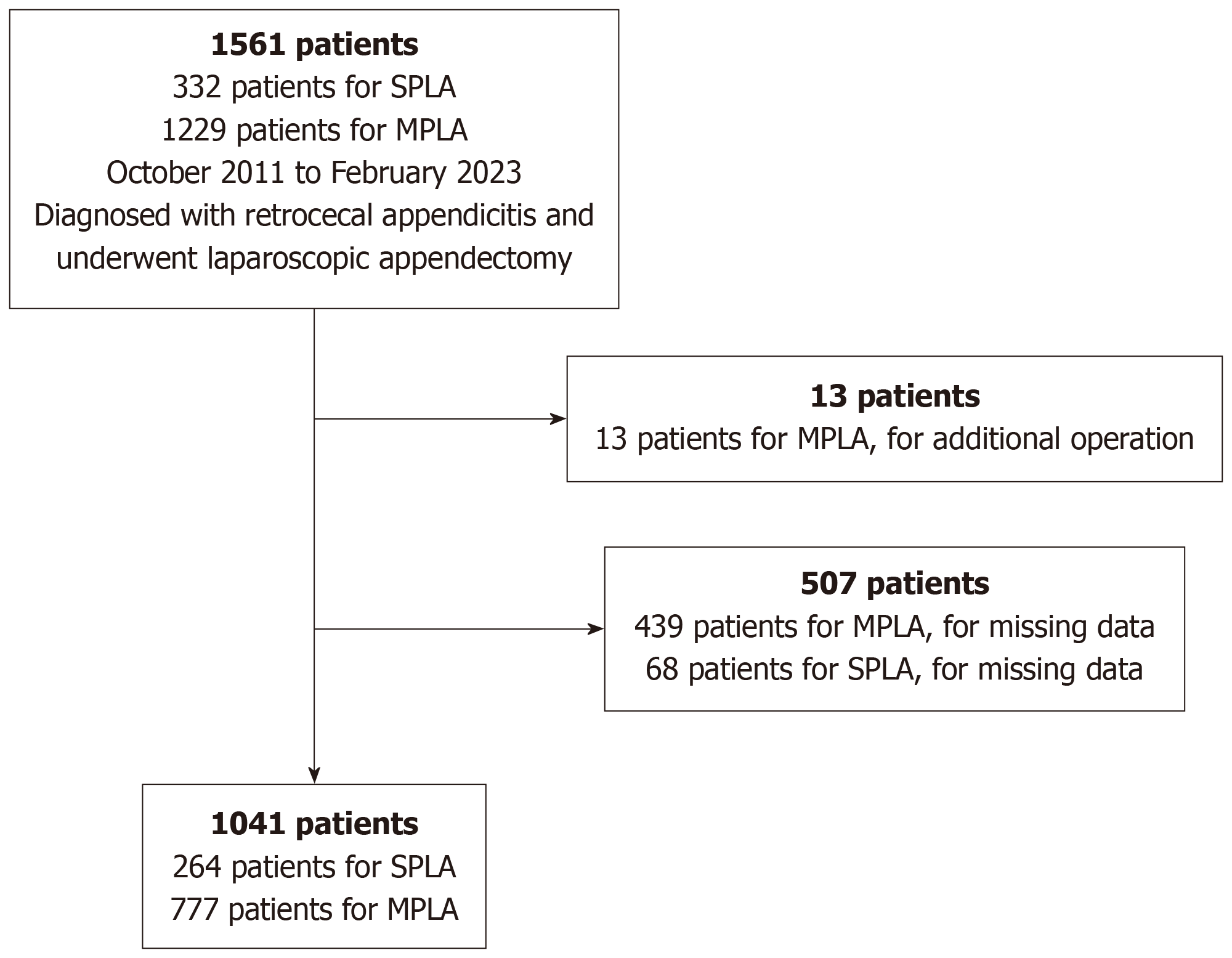
Figure 2 Flow charts of patient selection process.
SPLA: Single-port laparoscopic appendectomy; MPLA: Multi-port laparoscopic appendectomy.
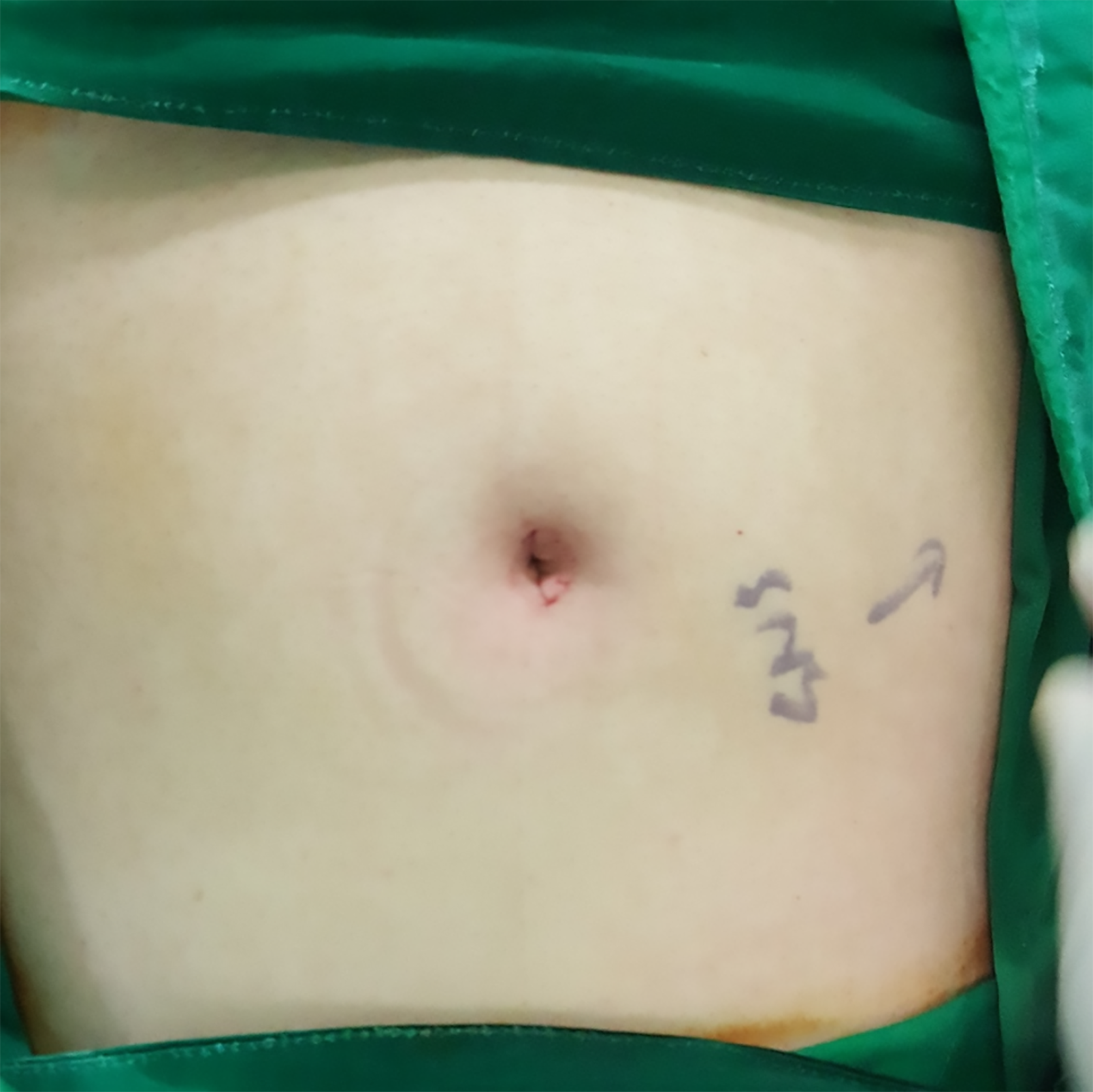
Figure 3 Postoperative surgical wound site after single-port laparoscopic appendectomy.
This figure is generated based on a case performed at Konyang University Hospital.
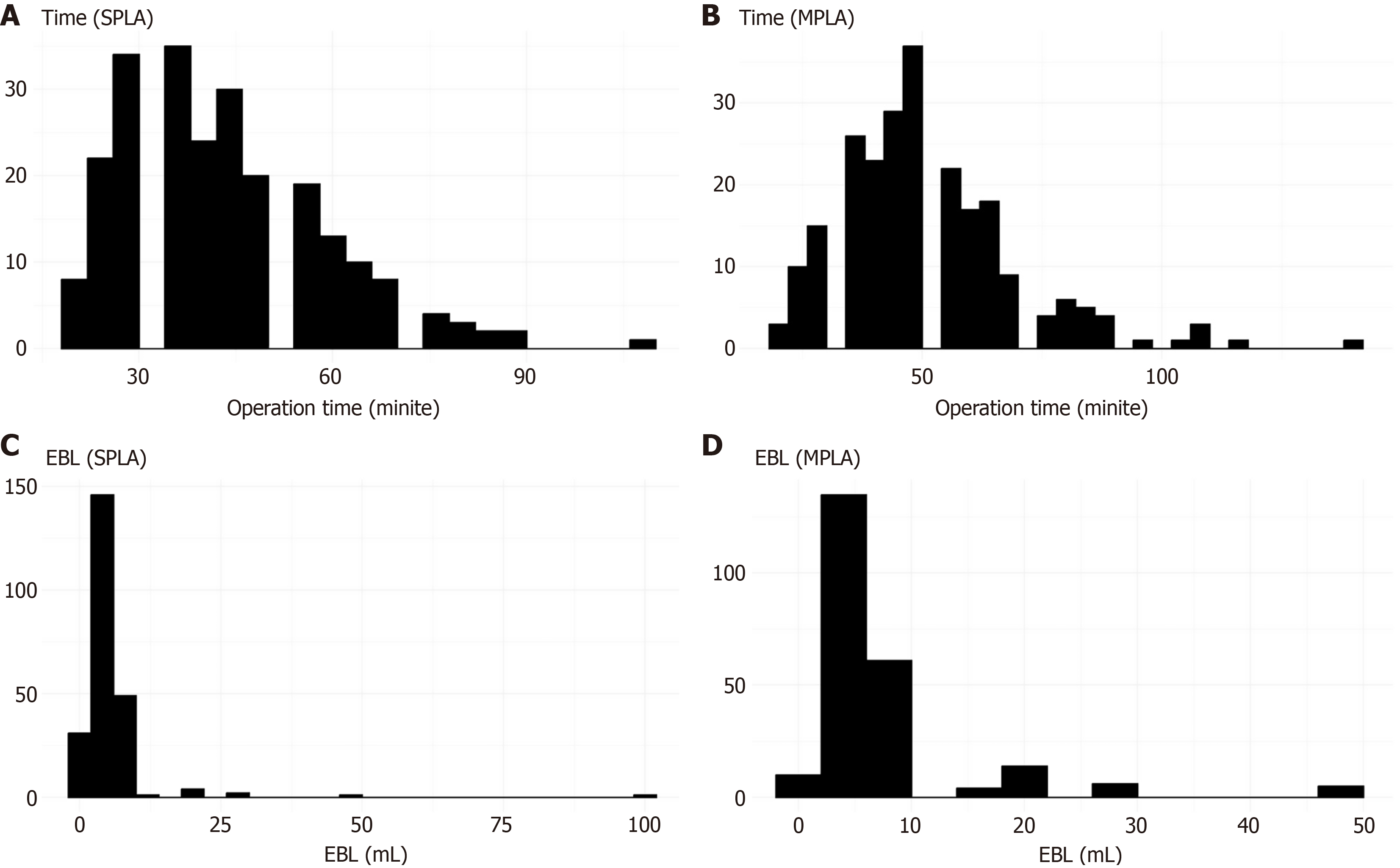
Figure 4 Histogram for comparing operation time and estimated blood loss between the single-port laparoscopic appendectomy group and multi-port laparoscopic appendectomy group.
A: Histogram of operation time for single-port laparoscopic appendectomy (SPLA); B: Histogram of operation time for multi-port laparoscopic appendectomy (MPLA); C: Histogram of estimated blood loss (EBL) for SPLA; D: Histogram of EBL for MPLA. SPLA: Single-port laparoscopic appendectomy; MPLA: Multi-port laparoscopic appendectomy; EBL: Estimated blood loss.
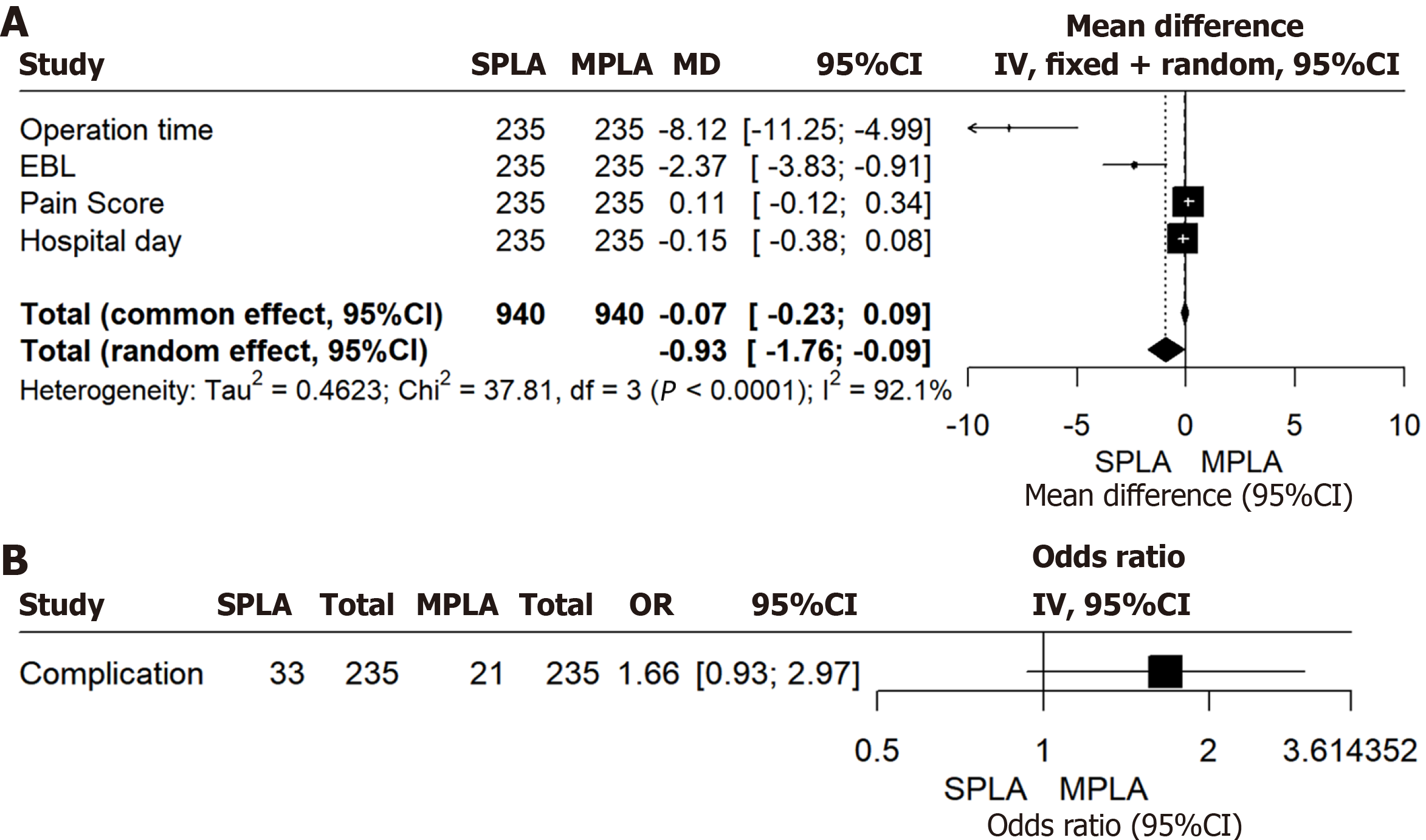
Figure 5 Non-inferiority test.
A: Continuous variables; B: Categorical variables. SPLA: Single-port laparoscopic appendectomy; MPLA: Multi-port laparoscopic appendectomy; EBL: Estimated blood loss; OR: Odds ratio.
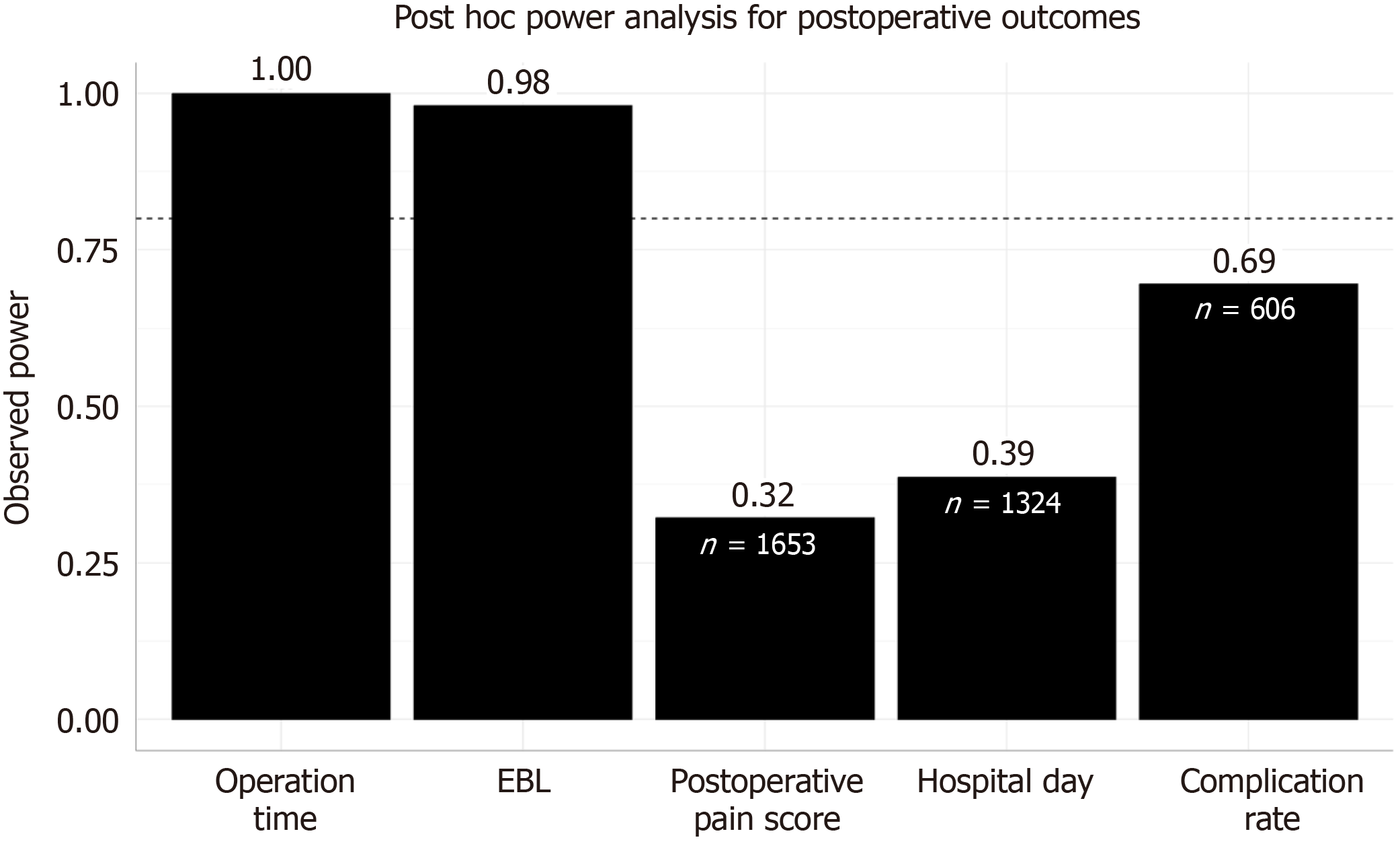
Figure 6 Post-hoc power analysis for postoperative outcomes.
EBL: Estimated blood loss.
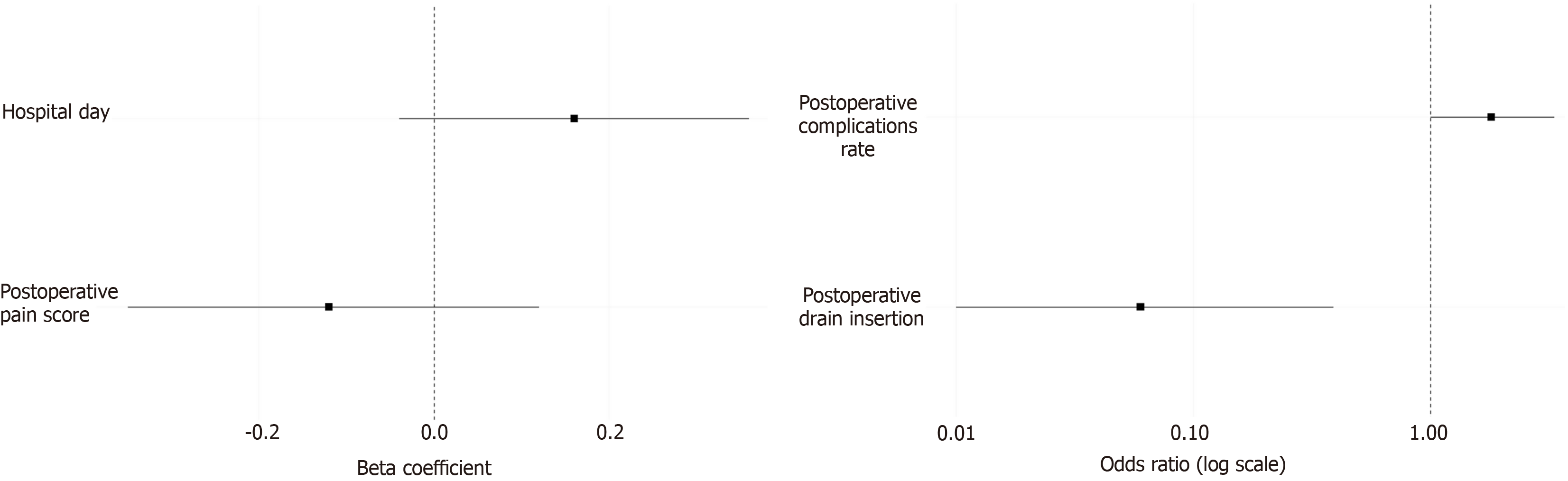
Figure 7 Forest plot for multivariable logistic regression comparing the single-port laparoscopic appendectomy and multi-port laparoscopic appendectomy groups.
- Citation: Woo SA, Roh SJ, Sung NS, Choi WJ. Feasibility of single-port laparoscopic appendectomy for retrocecal appendicitis: A propensity score-matched study with multi-port laparoscopic appendectomy. World J Gastrointest Surg 2025; 17(7): 105925
- URL: https://www.wjgnet.com/1948-9366/full/v17/i7/105925.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i7.105925