Copyright
©The Author(s) 2025.
World J Gastrointest Surg. May 27, 2025; 17(5): 106784
Published online May 27, 2025. doi: 10.4240/wjgs.v17.i5.106784
Published online May 27, 2025. doi: 10.4240/wjgs.v17.i5.106784
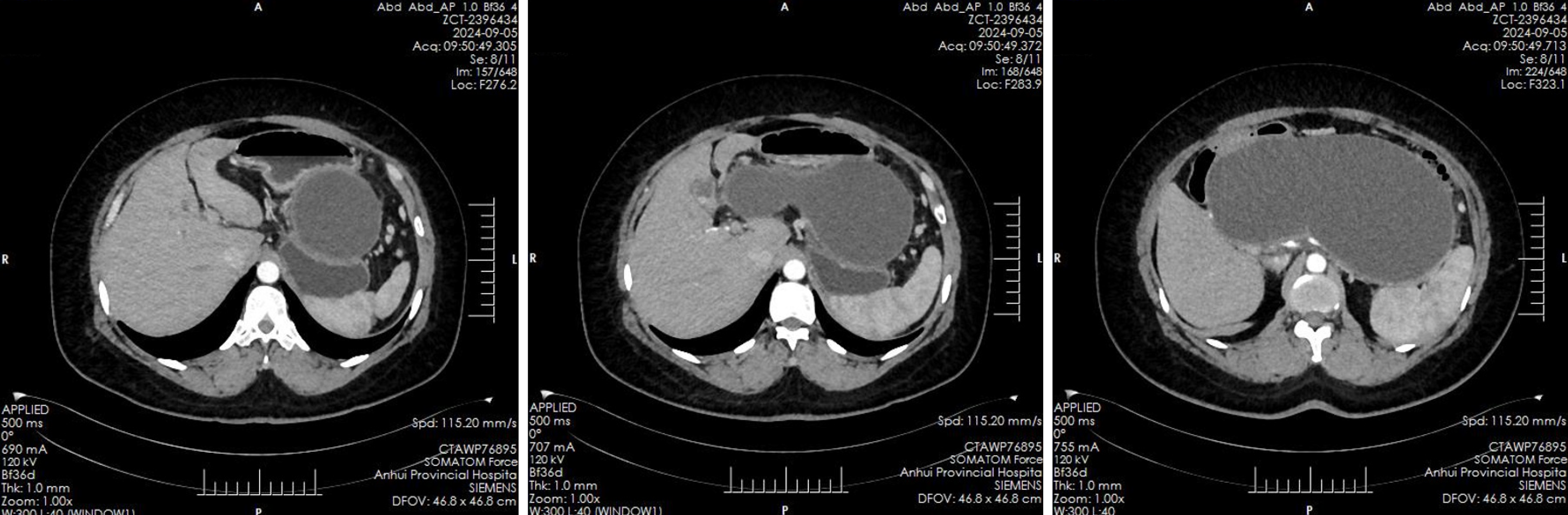
Figure 1 Enhanced computed tomography scan of the upper abdomen.
The computed tomography scan reveals the presence of an irregular elliptical cystic low-density shadow measuring approximately 232 mm by 114 mm in the region of the pancreas, which is not distinctly delineated from the surrounding pancreatic tissue. Notably, there is no significant dilation observed in the intrahepatic and extrahepatic bile ducts, nor in the common bile duct. Additionally, multiple gallstones are identified within the gallbladder.
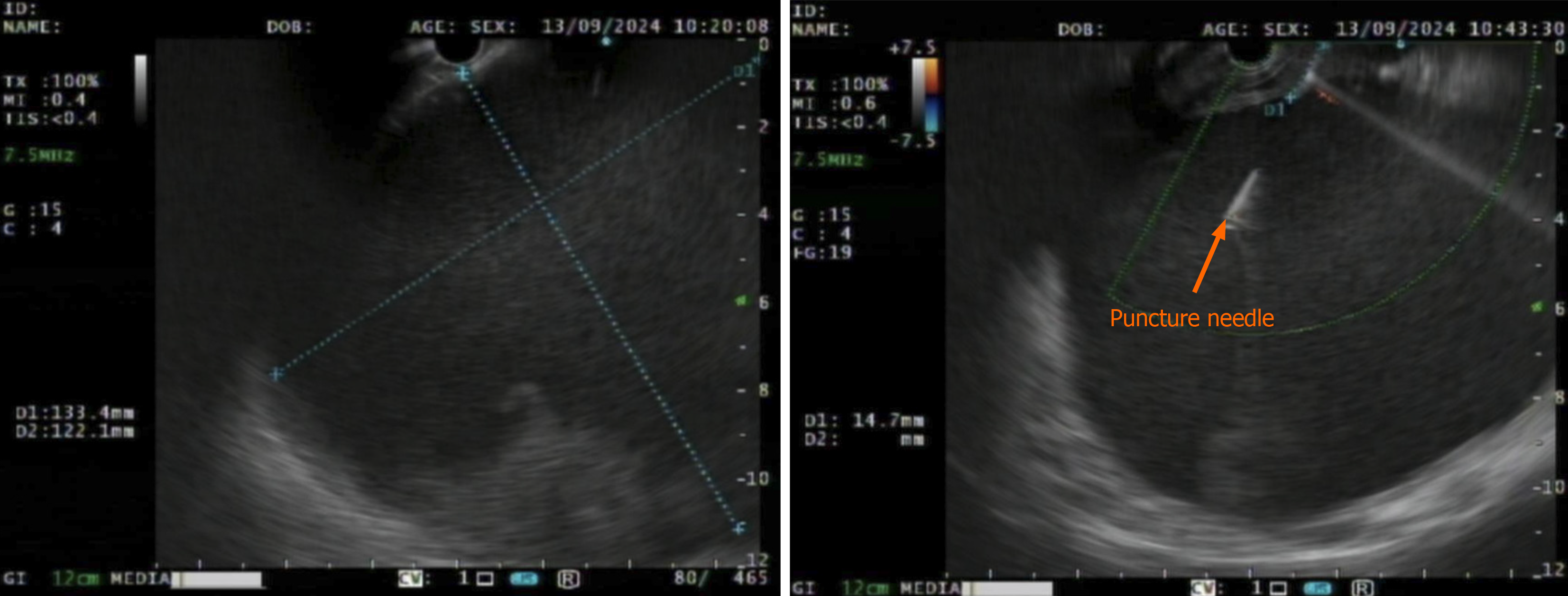
Figure 2 Endoscopic ultrasound findings.
Endoscopic ultrasound indicates a circular hypoechoic lesion surrounding the body of the pancreas, accompanied by scattered hyperechoic changes in certain areas. A puncture was performed using a Boco 23G needle, resulting in the extraction of a coffee-colored liquid.
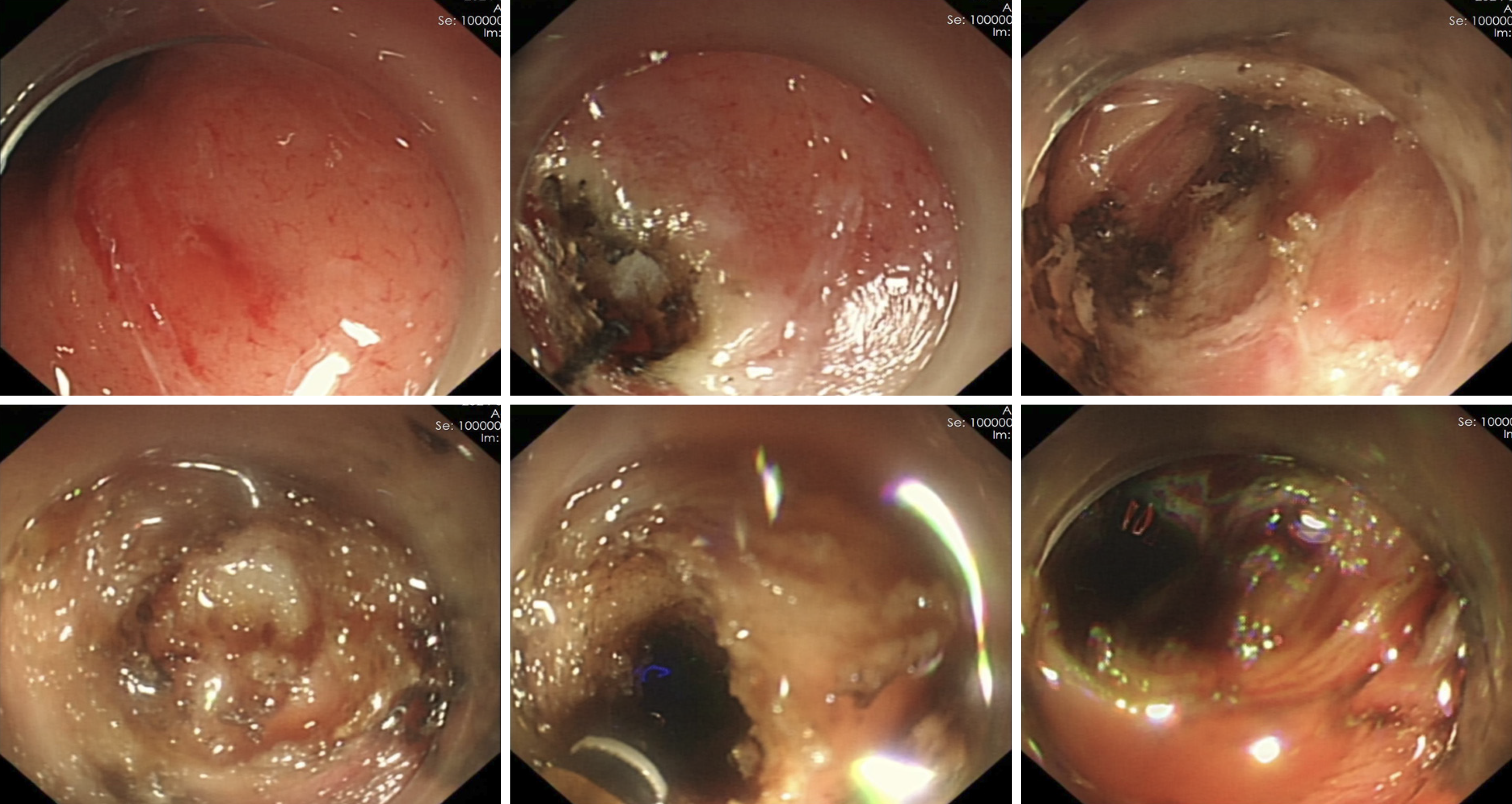
Figure 3 The endoscopic treatment.
The puncture site was marked, and an incision was made in the gastric wall using an electric knife, revealing a white, wall-like tissue exterior to the gastric wall. Upon aspiration with the puncture needle, the coffee-colored liquid was observed, prompting a deeper incision at this site, which resulted in a significant outflow of liquid.
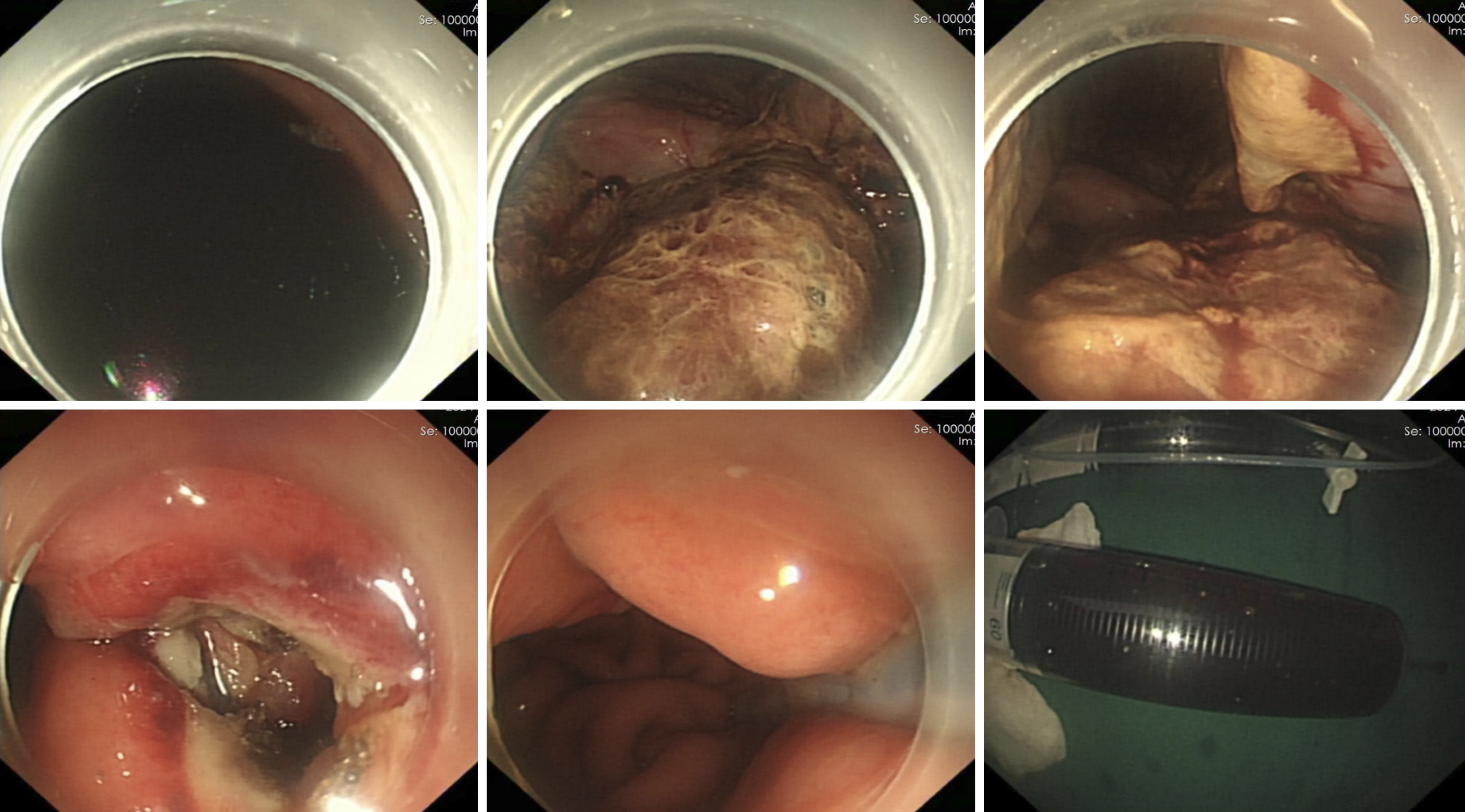
Figure 4 A gastric tube was subsequently placed under endoscopic guidance.
The gastroscope was introduced into the cystic cavity to aspirate the liquid, revealing flocculent material at the base of the cavity. Hemostasis was achieved, and a gastric tube was positioned.
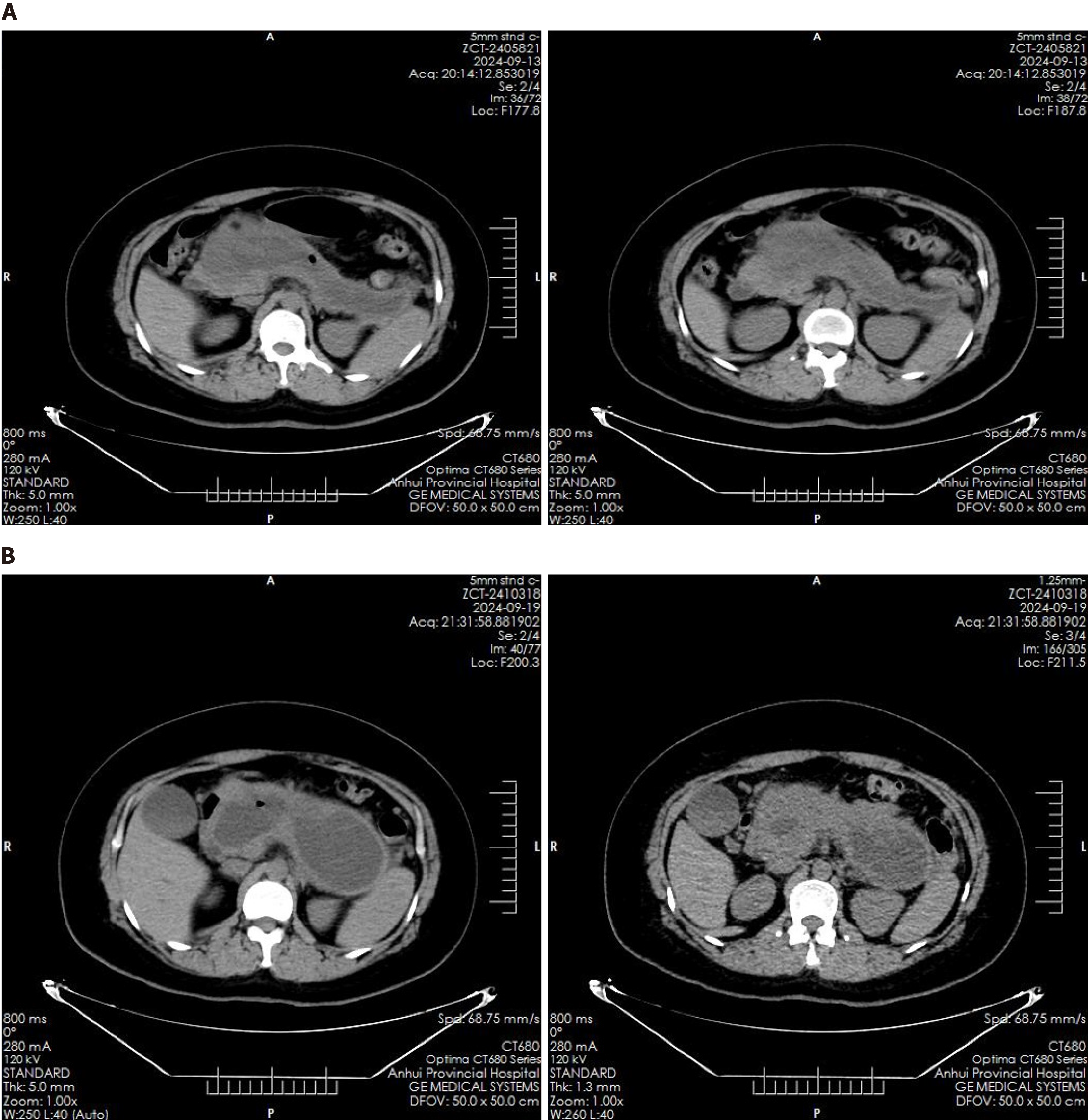
Figure 5 Postoperative computed tomography imaging.
A: Computed tomography imaging conducted eight hours post-endoscopic intervention indicated no immediate complications; B: Follow-up gastroscopy performed six days postoperatively revealed the presence of ulcers on the gastric wall at the incision site, with no evidence of a fistula.
- Citation: Liu YL, Liu J, Jiang WJ, Zhang KG, Wang YT. Ultrasound-guided endoscopic drainage for the management of pancreatic pseudocysts: A case report. World J Gastrointest Surg 2025; 17(5): 106784
- URL: https://www.wjgnet.com/1948-9366/full/v17/i5/106784.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i5.106784