©The Author(s) 2025.
World J Gastrointest Surg. May 27, 2025; 17(5): 105894
Published online May 27, 2025. doi: 10.4240/wjgs.v17.i5.105894
Published online May 27, 2025. doi: 10.4240/wjgs.v17.i5.105894
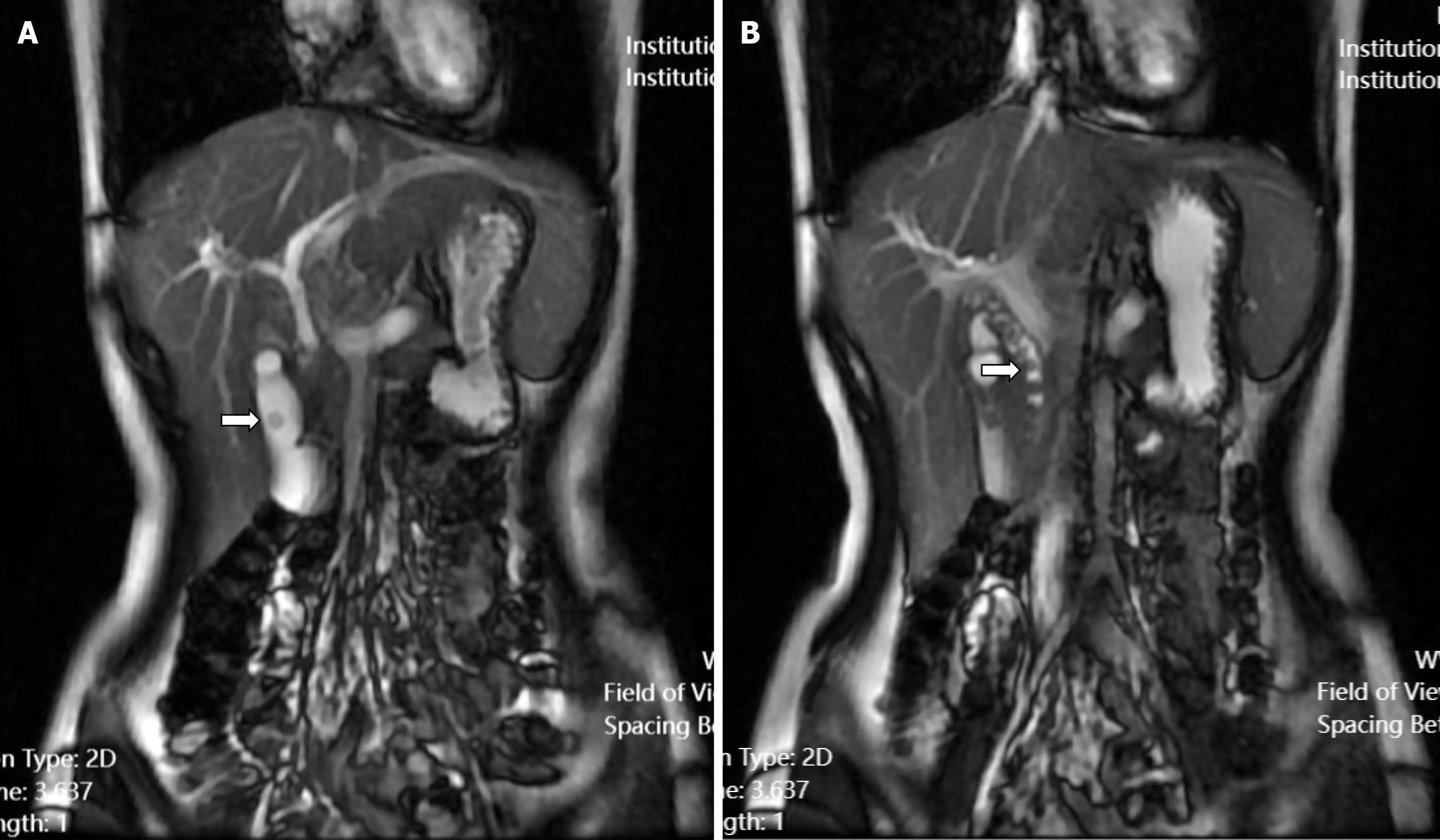
Figure 1 Preoperative magnetic resonance cholangiopancreatography of the abdomen.
A: A stone (white arrow) in the gallbladder; B: Multiple stones (white arrow) in the common bile duct.
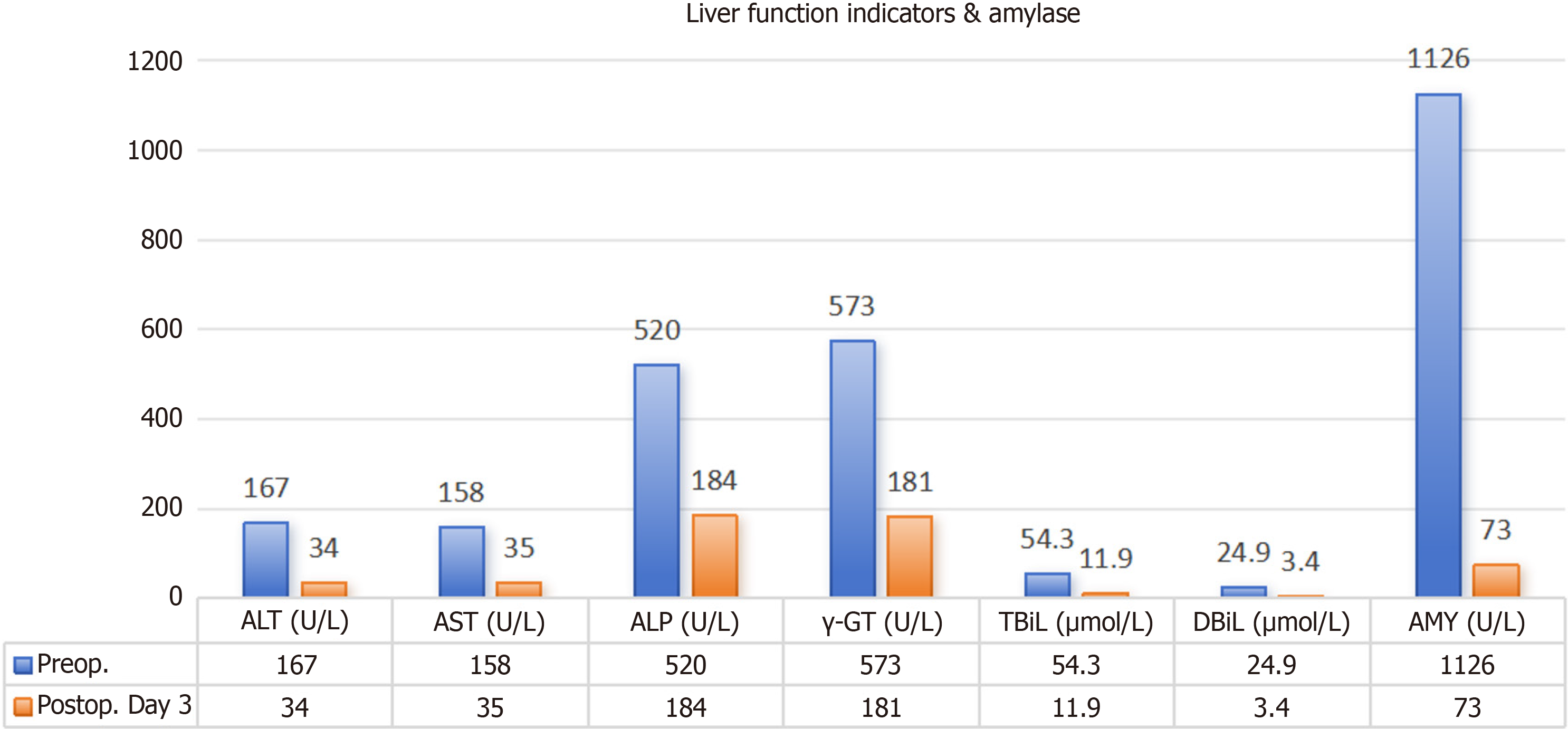
Figure 2 Comparative liver function tests and serum amylase levels in the patient before surgery and on postoperative day 3.
ALT: Alanine aminotransferase; AST: Aspartate aminotransferase; ALP: Alkaline phosphatase; γ-GT: γ-glutamyl transferase; TBiL: Total bilirubin; DBil: Direct bilirubin; AMY: Amylase; Preop: Preoperative; Postop: Postoperative.
Figure 3 Preoperative computed tomography scan of the upper abdomen.
A: Plain phase revealed an enlarged gallbladder and dilated common bile duct, with the common bile duct measuring approximately 1.3 cm in maximum diameter (white arrow); B: Arterial phase revealed a slightly dilated main pancreatic duct (black arrow); C: Venous phase.
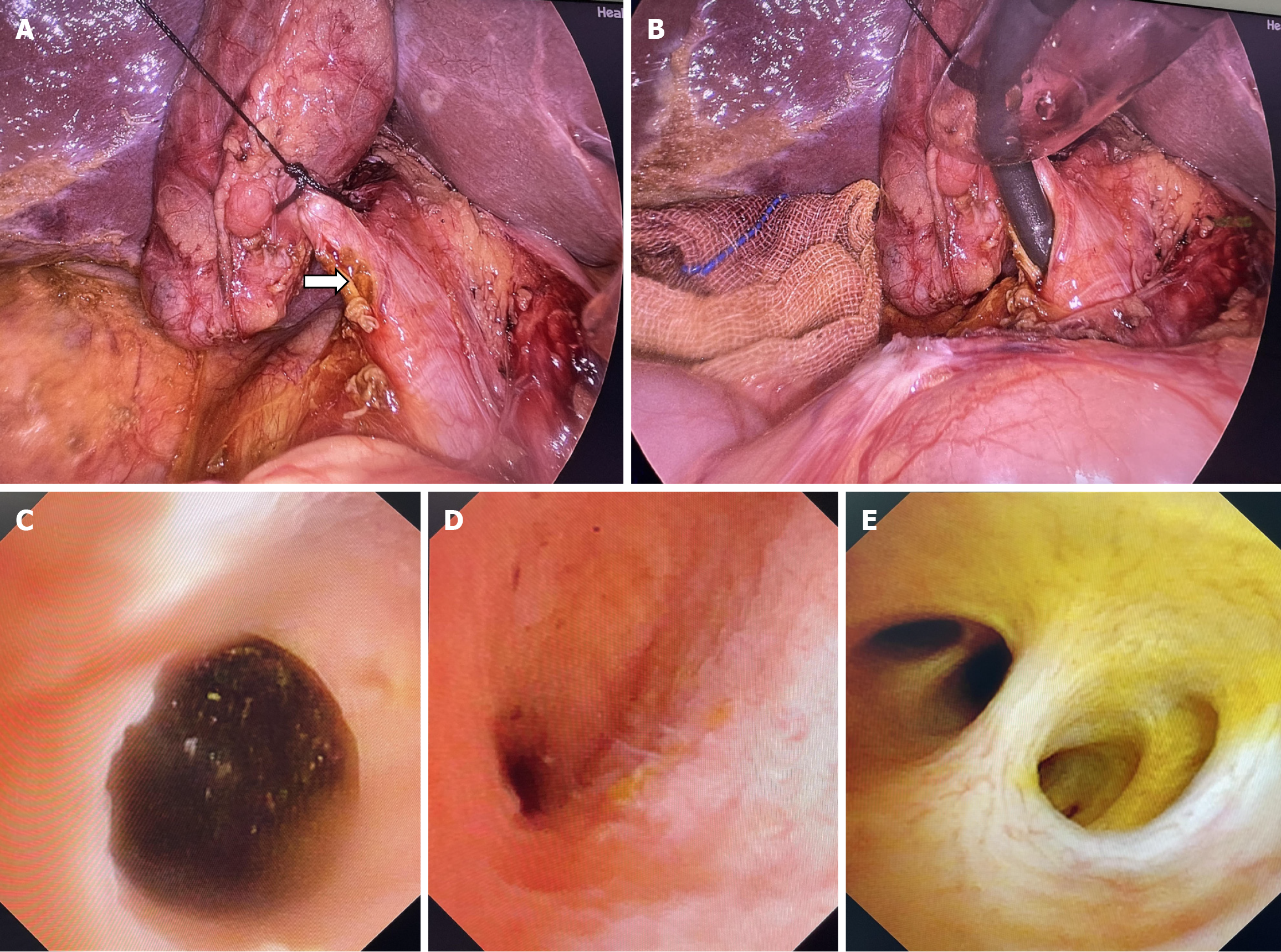
Figure 4 Laparoscopic micro-incision technique applied at the cystic duct confluence during laparoscopic common bile duct exploration procedure.
A: Pre-ligating and applying traction to the distal cystic duct with a 4-0 silk suture, the Calot’s triangle was exposed, and a microincision was made at the cystic duct-common bile duct (CBD) confluence (white arrow); B: Choledochoscope insertion through the micro-incision at cystic duct confluence; C: During choledochoscopy, stones were identified in the middle and lower segments of the CBD, which were subsequently extracted using a basket retrieval technique; D: Upon reinsertion of the choledochoscope, no stones were observed in the distal and middle segments of the CBD; E: Upon repositioning the choledochoscope, no stones were identified in the proximal segment of the CBD.
Figure 5
The drainage tube was removed prior to the patient's discharge, leaving only a small drain site (white arrow).
- Citation: Chen GB, Sha YG, Wang ZL, Wang DB, Tang RM, Chen YS. Laparoscopic micro-incision technique at cystic duct confluence for pediatric choledocholithiasis management: A case report. World J Gastrointest Surg 2025; 17(5): 105894
- URL: https://www.wjgnet.com/1948-9366/full/v17/i5/105894.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i5.105894