©The Author(s) 2024.
World J Gastrointest Surg. Nov 27, 2024; 16(11): 3590-3597
Published online Nov 27, 2024. doi: 10.4240/wjgs.v16.i11.3590
Published online Nov 27, 2024. doi: 10.4240/wjgs.v16.i11.3590
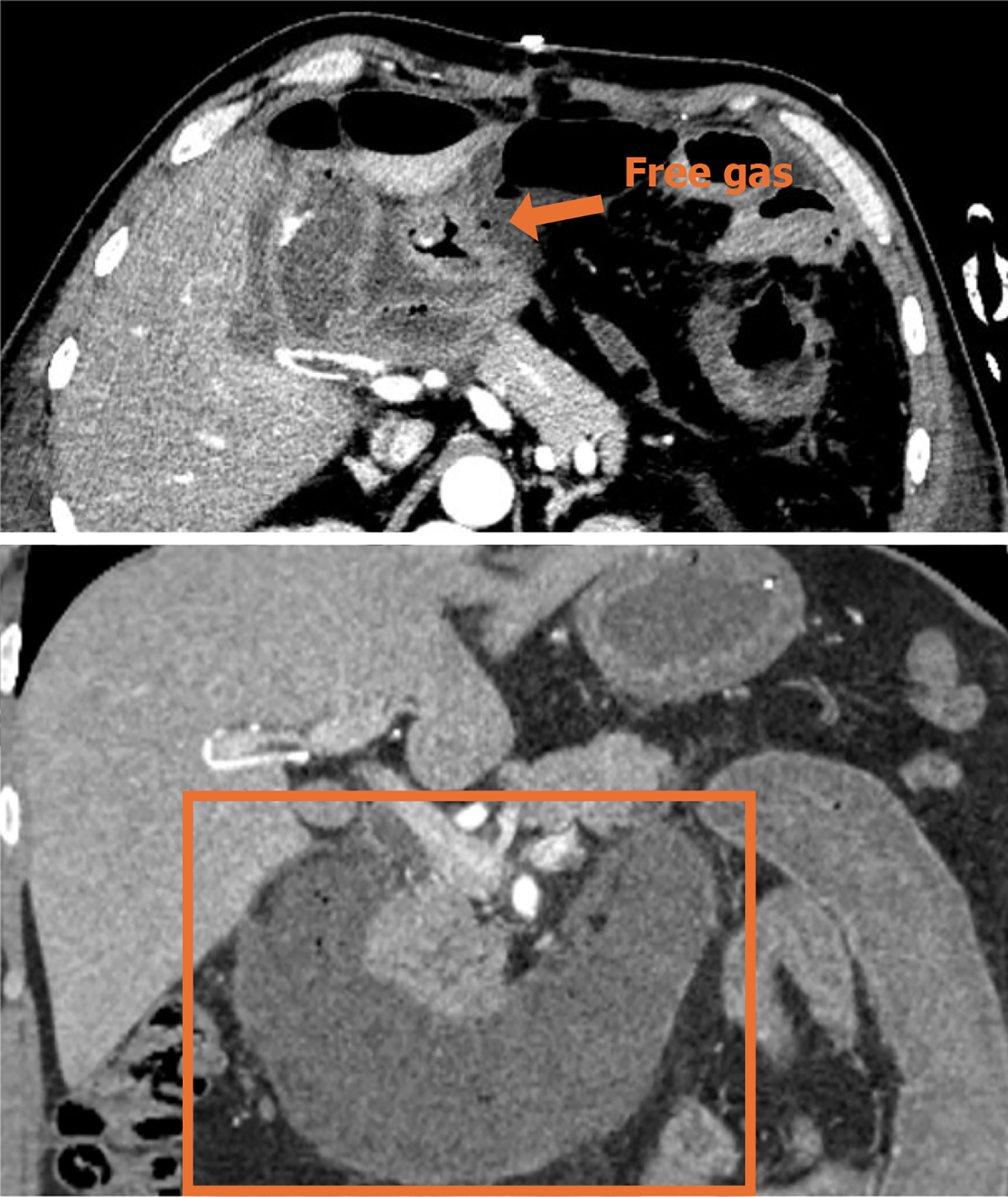
Figure 1 Preoperative contrast-enhanced computed tomography of the abdominopelvic cavity.
Diffuse thickening of the gastric wall and duodenal intestinal wall in the gastric sinus department, blurring of the plasma membrane surface, blurring of the peripheral fat interstitial space with multiple plaques and cord shadows, a few gas-dense shadows were seen at the edge of the gastric sinus, and the head of the neighboring pancreas was also seen. The head of the neighboring pancreas was full, with blurred borders, the dilatation of the lumen of the gastric sinus and the duodenal tube, and the edema and thickening of the wall of the gastric sinus. Thickening of the wall of the proximal jejunum. Diagnostic imaging considered sulcus pancreatitis suspected perforation of the gastric sinus.
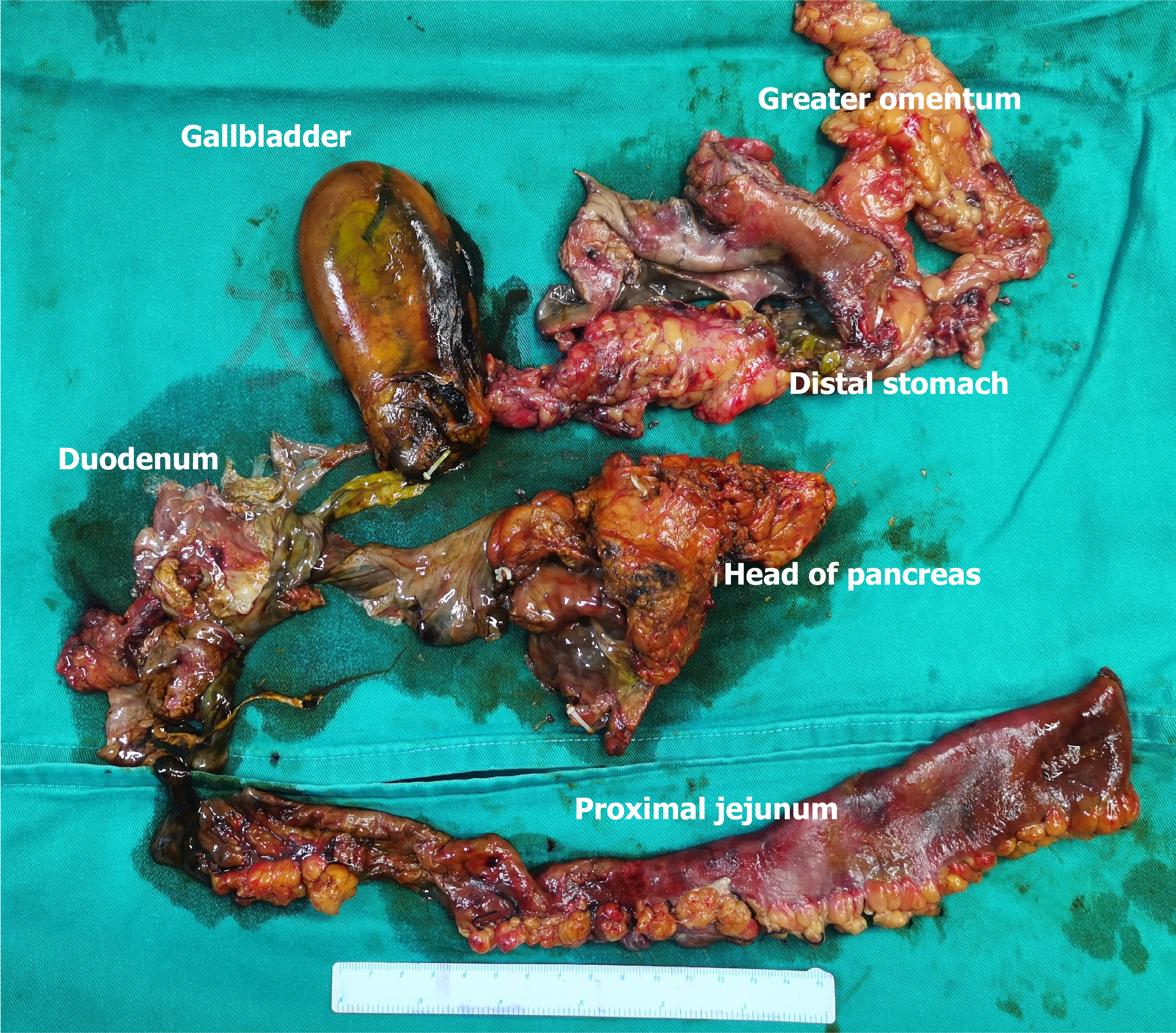
Figure 2 Specimen.
The distal part of the stomach, the entire length of the duodenum, and the proximal 30 cm of the jejunum were necrotic. Most of the gastric wall and duodenal tissue was necrotic and disappeared, and the proximal jejunal wall structure remained.
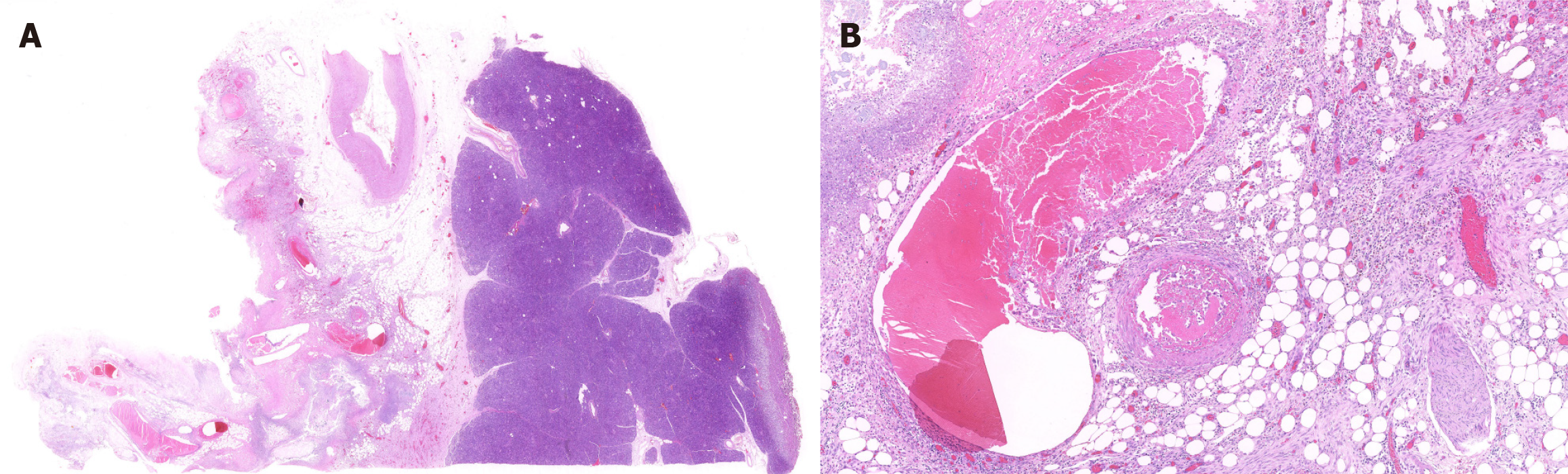
Figure 3 Pathological sections of the pancreas and peripancreatic tissue.
A: 1 × pancreas (right) and peripancreatic tissue (left); B: 10 × inflammatory infiltration of peripancreatic tissue, necrosis, with thrombosis.
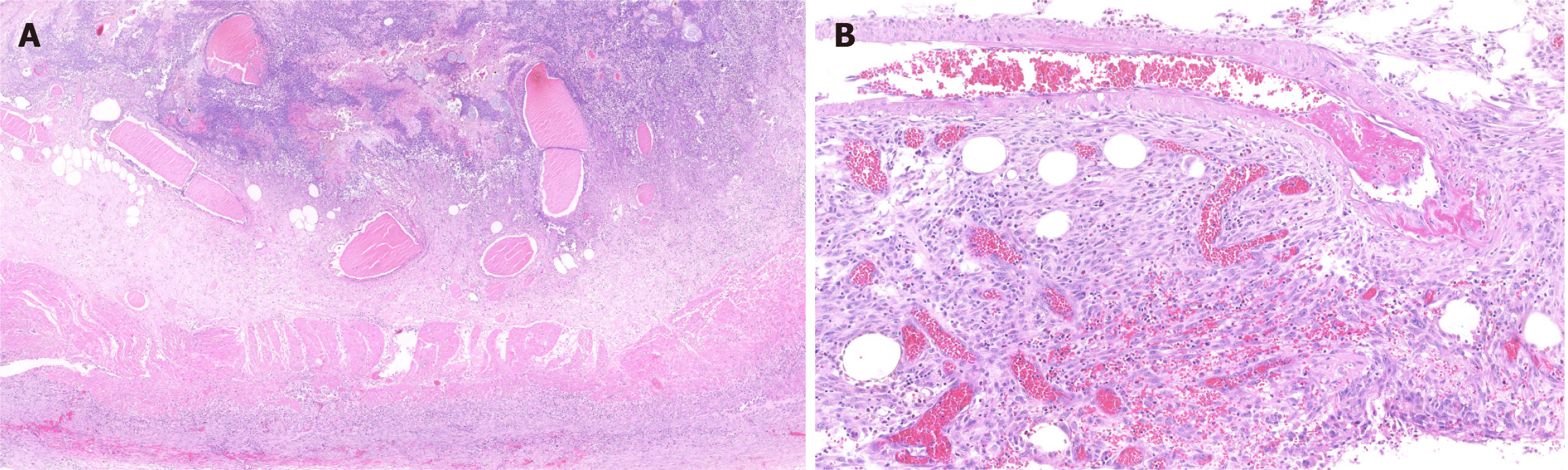
Figure 4 Pathological section of the jejunal wall.
A: 4 × acute inflammatory exudation with necrosis of the entire jejunal wall; B: 20 × extensive thrombosis within the jejunal wall.
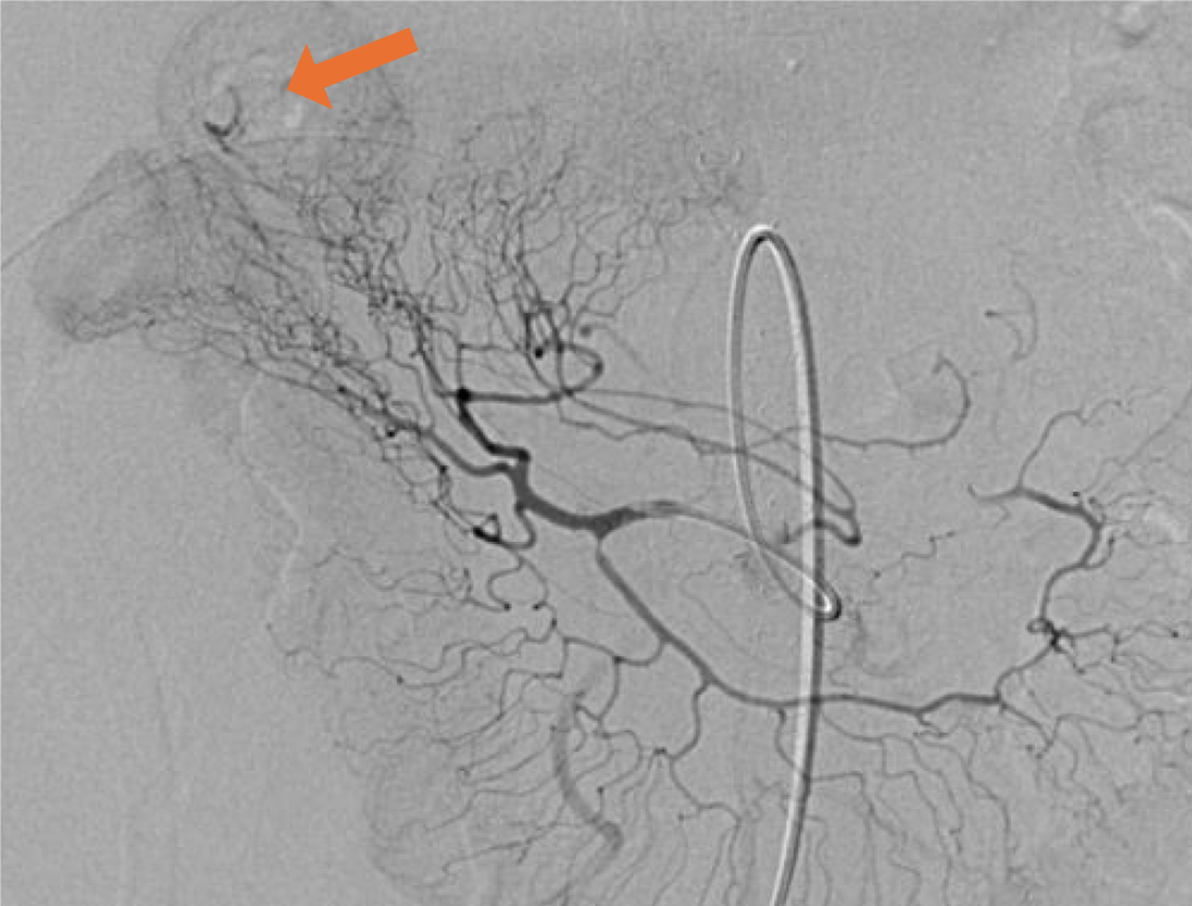
Figure 5 Postoperative superselective intra-arterial embolization for gastrointestinal bleeding.
Postoperative day 7, angiography showed a contrast spillage from one of the first jejunal artery, which was considered to be intestinal hemorrhage at the billiary-enteric anastomosis.
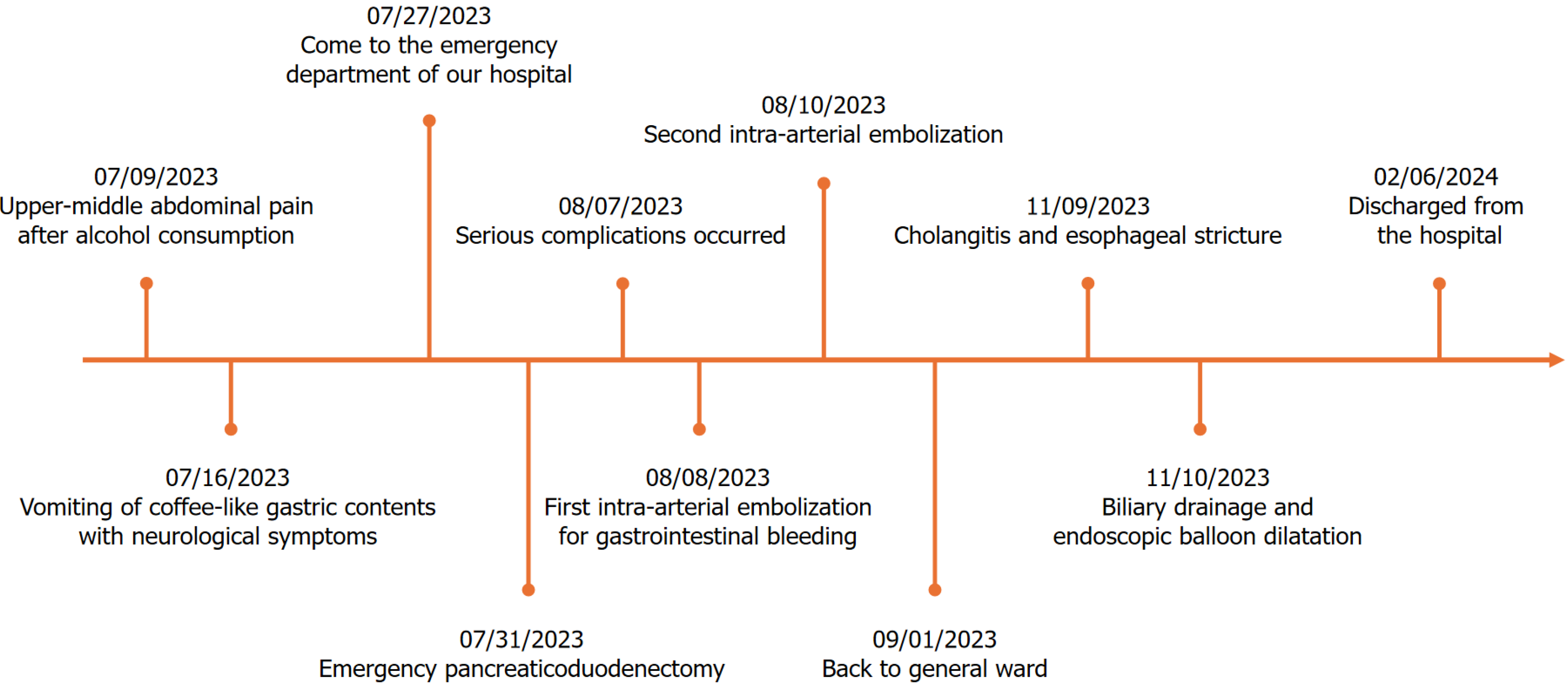
Figure 6 Time points correspond to the diagnostic and therapeutic process.
- Citation: Tong KN, Zhang WT, Liu K, Xu R, Guo W. Emergency pancreaticoduodenectomy for pancreatitis-associated necrotic perforation of the distal stomach and full-length duodenum: A case report. World J Gastrointest Surg 2024; 16(11): 3590-3597
- URL: https://www.wjgnet.com/1948-9366/full/v16/i11/3590.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i11.3590