©The Author(s) 2023.
World J Gastrointest Surg. Mar 27, 2023; 15(3): 488-494
Published online Mar 27, 2023. doi: 10.4240/wjgs.v15.i3.488
Published online Mar 27, 2023. doi: 10.4240/wjgs.v15.i3.488
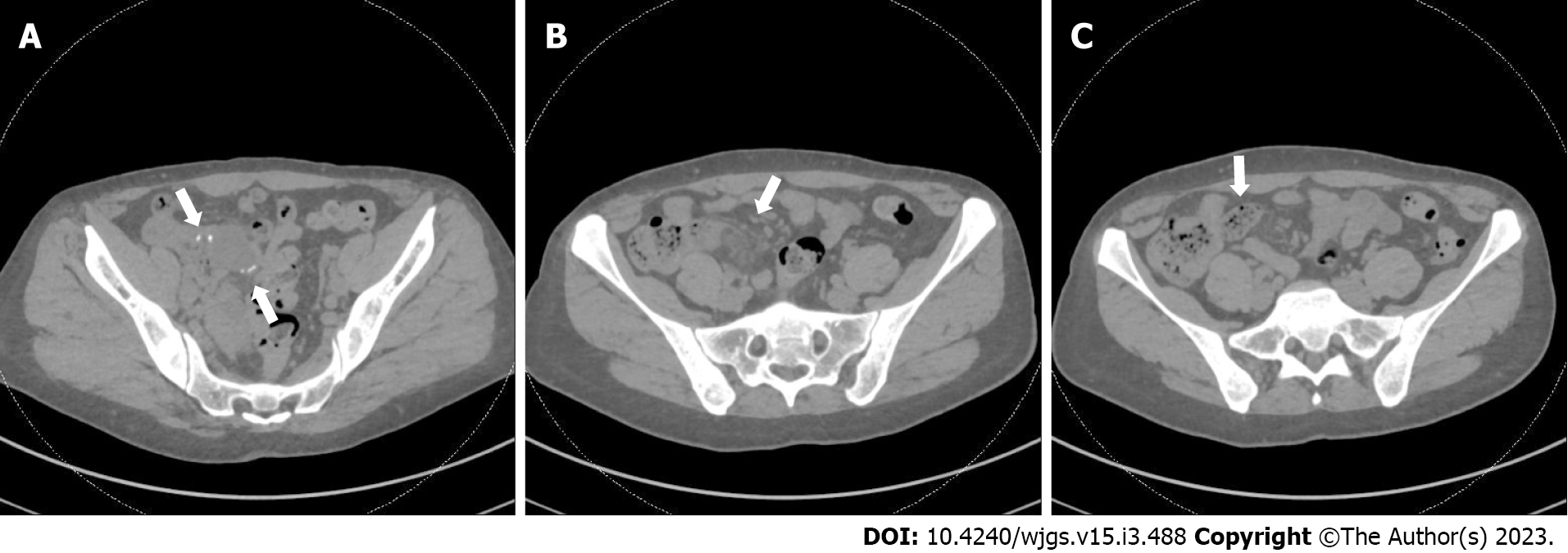
Figure 1 Computed tomography scan of her abdomen and pelvis without contrast.
A: Prior anastomotic suture line is visualized (arrows) and appeared intact; B: Mild surrounding inflammatory stranding (arrow) seen near the prior anastomosis; C: Fecalization (arrow) noted in small bowel adjacent to anastomosis.
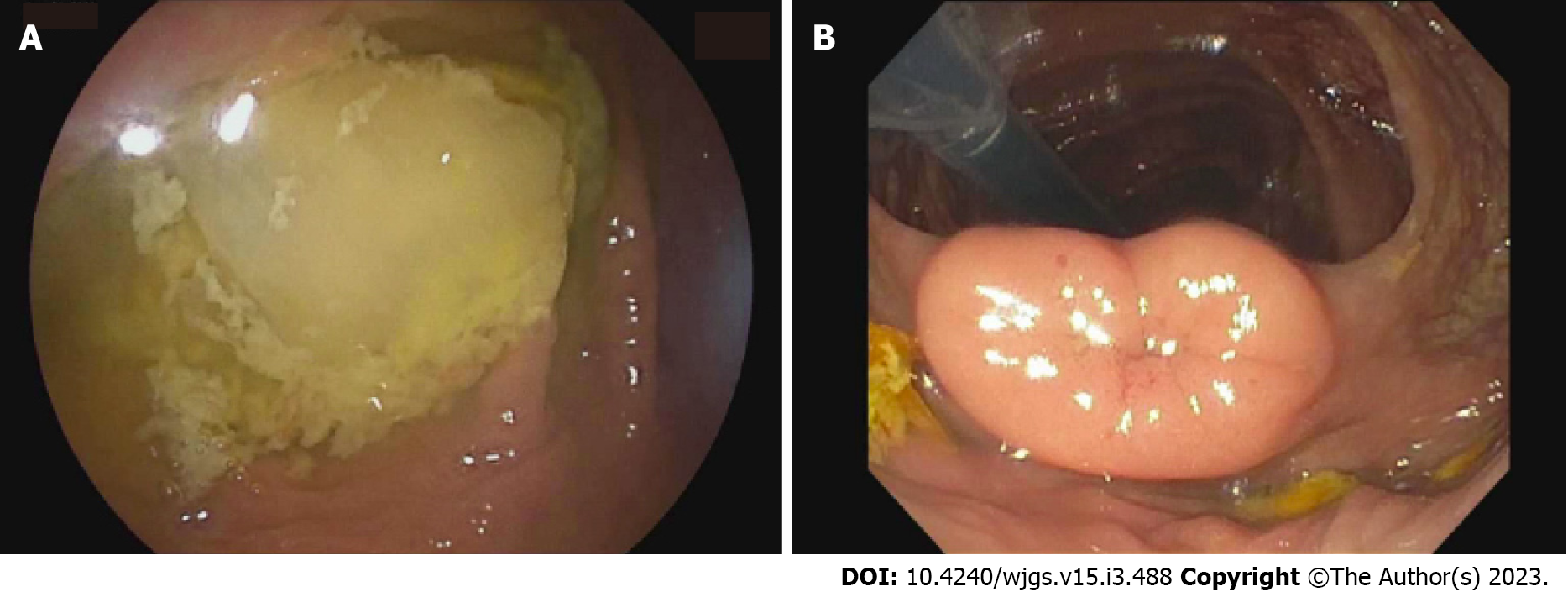
Figure 2 Double balloon enteroscopy.
A: The entire examined colon appeared normal, including the cecum; B: The ileocecal valve. The terminal ileum (TI) was only marginally intubated and could not be advanced further. The visualized portion of the TI (approximately 3 cm) appeared normal.
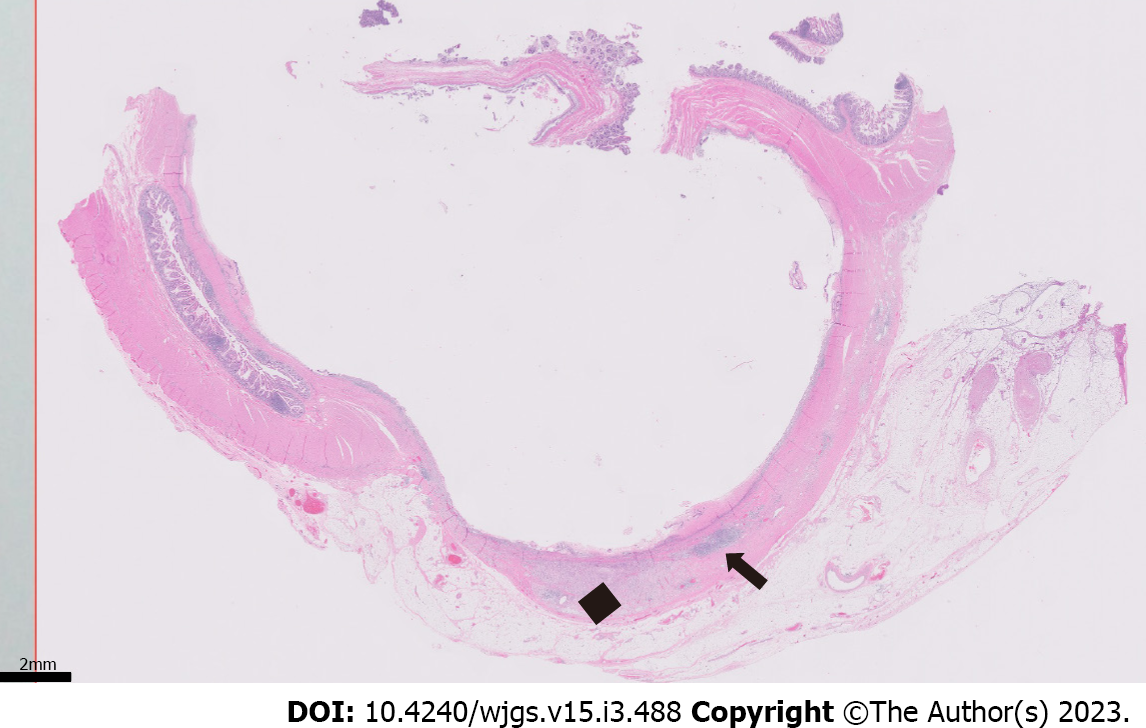
Figure 3 Gross specimen.
Gross examination revealed a 7 cm long region of cystically dilated small intestine immediately adjacent to the anastomosis, which was filled with abundant intraluminal pus.
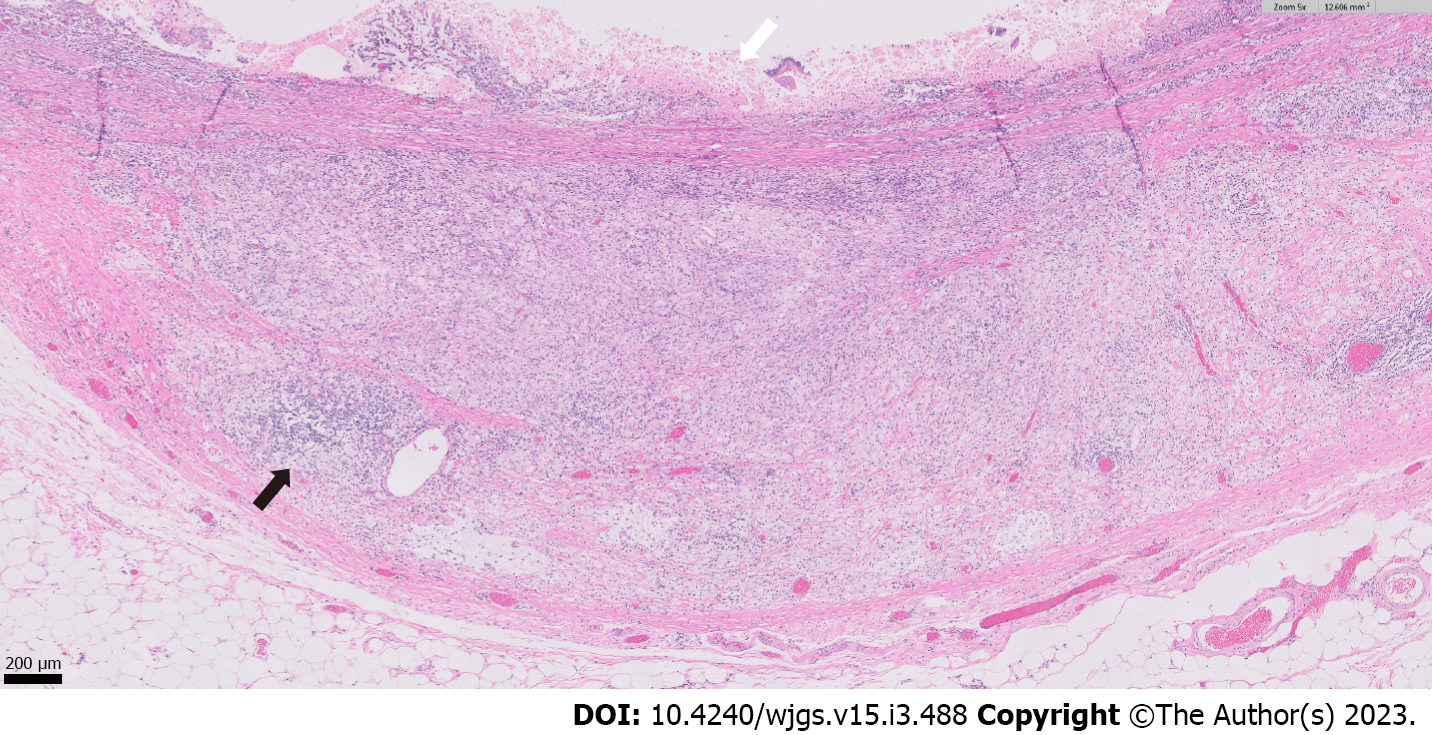
Figure 4 Low-magnification section of the specimen.
Microscopic (0.5 × objective magnification) cross section of the cystically dilated small intestine with mucosal ulceration (diffusely involving the luminal surface) and chronic inflammation (arrow), fibrosis, and xanthogranulomatous inflammation (black diamond) of the underlying wall.
Figure 5 High-magnification section of the specimen.
Higher magnification (5 × objective magnification) image showing mucosal ulceration (white arrow) with abundant infiltration of the underlying small intestinal wall by collections of foamy, lipid-laden histiocytes (xanthogranulomatous inflammation), along with lymphocytes and plasma cells (example highlighted by black arrow).
- Citation: Wang W, Korah M, Bessoff KE, Shen J, Forrester JD. Xanthogranulomatous inflammation requiring small bowel anastomosis revision: A case report. World J Gastrointest Surg 2023; 15(3): 488-494
- URL: https://www.wjgnet.com/1948-9366/full/v15/i3/488.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i3.488