©The Author(s) 2022.
World J Gastrointest Surg. Dec 27, 2022; 14(12): 1425-1431
Published online Dec 27, 2022. doi: 10.4240/wjgs.v14.i12.1425
Published online Dec 27, 2022. doi: 10.4240/wjgs.v14.i12.1425
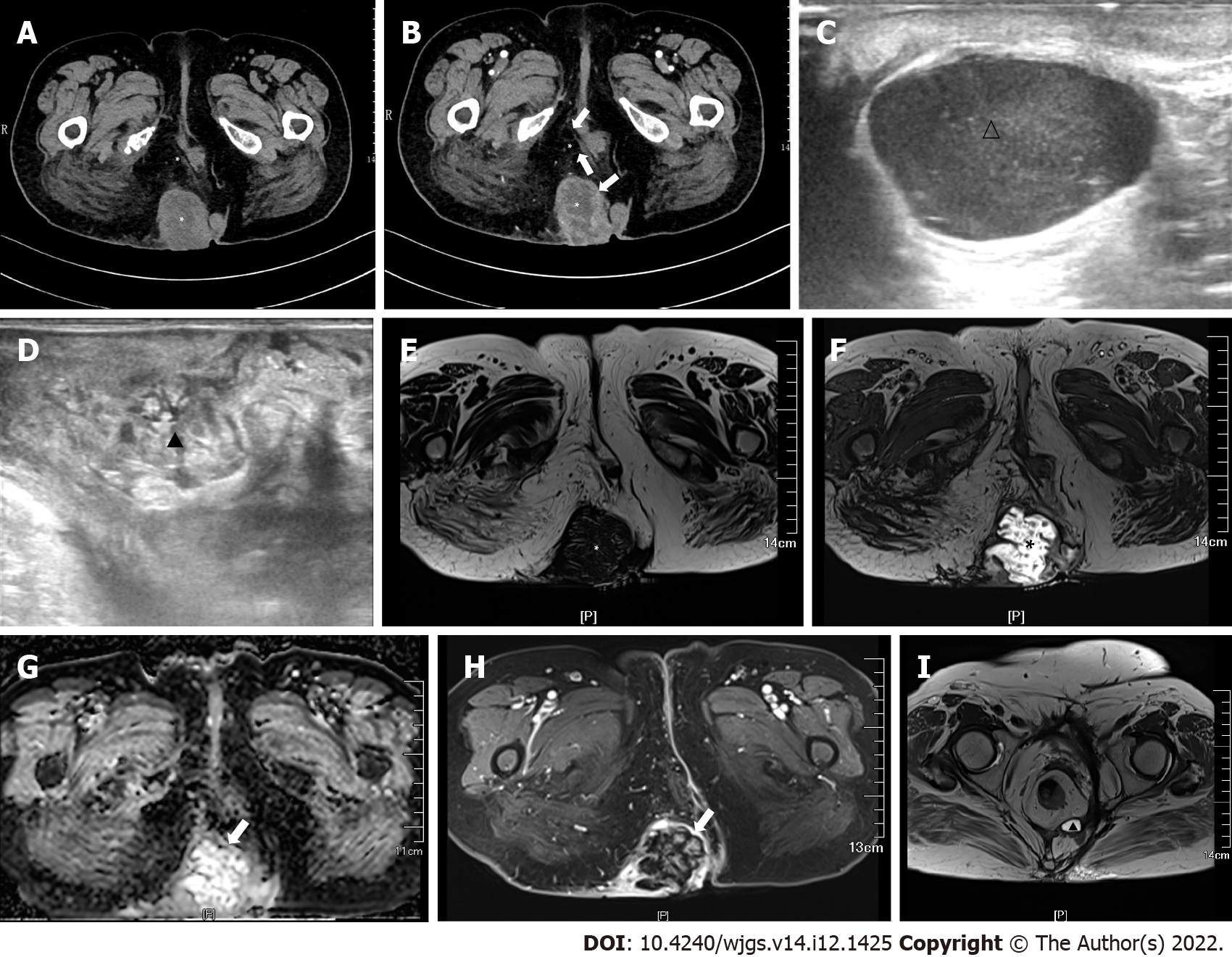
Figure 1 Computed tomography and magnetic resonance imaging.
A: A soft tissue mass and cystic density shadow were observed in the right hip and sacrococcygeal region (*), and the largest range was approximately 6.0 cm × 5.8 cm × 9.5 cm; B: The cyst was uneven, and the edge and septal of the focus were enhanced (↑); C and D: Multiple hypoechoic areas with a clear boundary (1.0–2.5 cm) were observed in the sacral region (∆) (C), and uneven echo areas in the right hip (▲) (D); E and F: The lesion had low-attenuation on T1 (*) (E) and high-attenuation on T2 (*) (F); G: Diffusion weighted image (↑). The longest diameter of the sagittal position was approximately 107 mm; H: The edge of the lesion was obviously enhanced (↑); I: Magnetic resonance imaging (T2) revealed a small cyst (▲) under the right levator ani.
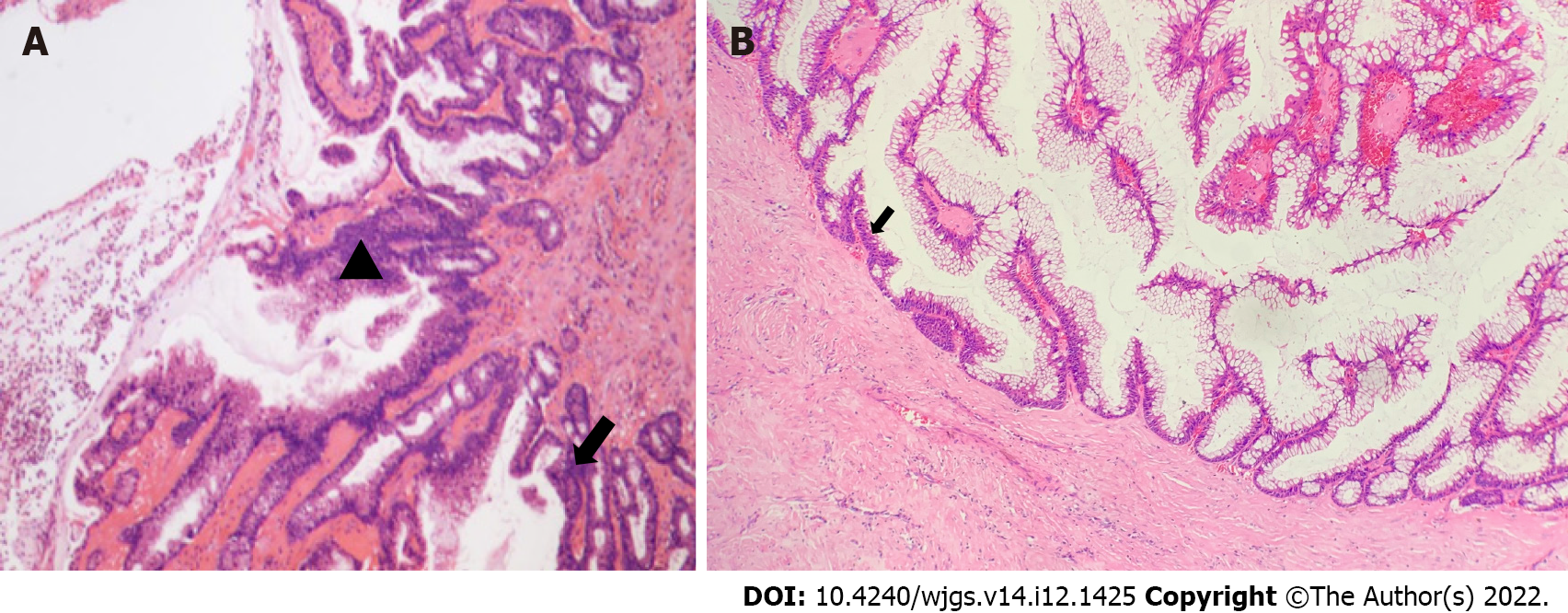
Figure 2 Histopathological analysis.
A: Moderate (▲)-to-severe (↑) dysplasia of the glandular epithelium; B: The columnar epithelial lining of the cyst wall had a large amount of mucus secretion, some of the epithelium had moderate dysplasia, and deranged smooth muscle bundles could be observed in the cyst wall (↑).
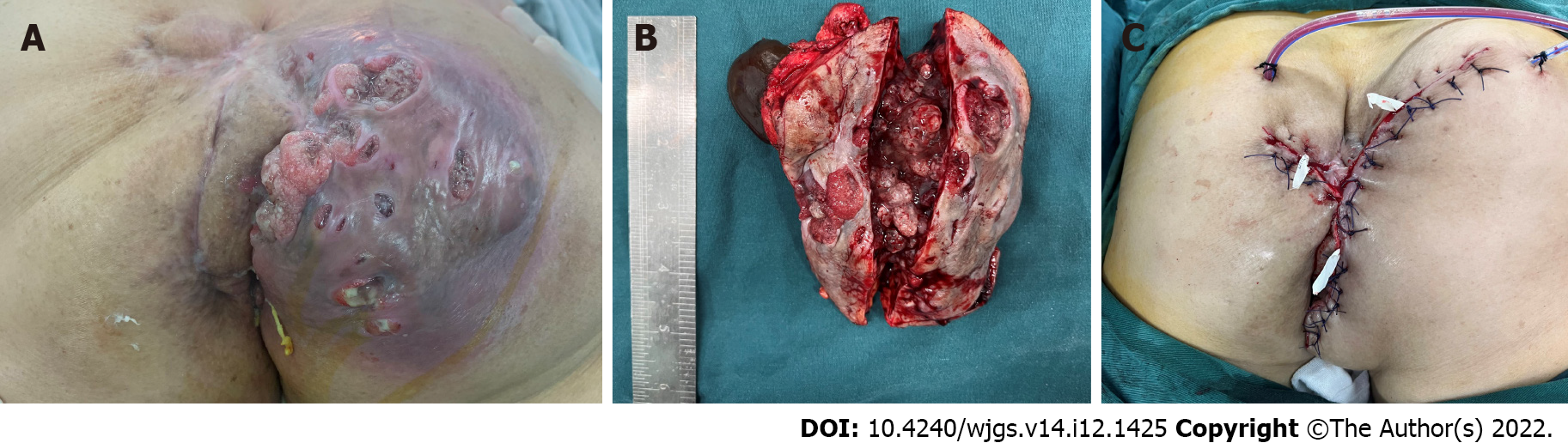
Figure 3 Macroscopic examination.
A: A 13 cm × 12 cm lesion was found on the right hip, with obvious fluctuation, reddish skin on the surface, multiple ruptures, jelly-like fluid outflow, and cauliflower-like objects attached to the base; B: Gross examination of the specimen revealed brown and jelly-like fluid in the cyst; C: The orthopedists assisted with the free skin flap, and closed the incision.
- Citation: Fang Y, Zhu Y, Liu WZ, Zhang XQ, Zhang Y, Wang K. Malignant transformation of perianal tailgut cyst: A case report. World J Gastrointest Surg 2022; 14(12): 1425-1431
- URL: https://www.wjgnet.com/1948-9366/full/v14/i12/1425.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v14.i12.1425