Published online Aug 16, 2017. doi: 10.4253/wjge.v9.i8.425
Peer-review started: December 31, 2016
First decision: March 27, 2017
Revised: March 30, 2017
Accepted: April 23, 2017
Article in press: April 24, 2017
Published online: August 16, 2017
Processing time: 226 Days and 5.4 Hours
Presence of Courvoisier’s or double duct signs in a jaundiced patient is suggestive of malignant obstruction of the pancreaticobiliary ductal system. The oncologic impact of the simultaneous occurrence of these signs on the survival of patients with periampullary cancer is unknown. We report a case of obstructive jaundice secondary to an ampullary cancer demonstrating the Courvoisier’s sign on clinical examination and a double duct sign on imaging. The patient underwent a pancreaticoduodenectomy which confirmed an ampullary adenocarcinoma.
Core tip: Presence of Courvoisier’s or double duct signs in a jaundiced patient is indicative of obstruction of the pancreaticobiliary ductal system most likely of malignant etiology. This study reports classic clinical and radiologic findings in ampullary adenocarcinoma. The oncologic impact of the simultaneous occurrence of these signs on the survival of patients with ampullary cancer is unknown.
- Citation: Agrawal S, Vohra S. Simultaneous Courvoisier’s and double duct signs. World J Gastrointest Endosc 2017; 9(8): 425-427
- URL: https://www.wjgnet.com/1948-5190/full/v9/i8/425.htm
- DOI: https://dx.doi.org/10.4253/wjge.v9.i8.425
Recent studies validate Courvoisier’s observation that gallbladder distension seldom occurs in stone obstruction of the bile duct and is usually seen with other causes of biliary obstruction[1,2]. The radiographic double duct sign comprising of the simultaneous dilation of the common bile duct (CBD) and main pancreatic duct (MPD) secondary to biductal obstruction is highly suggestive but not diagnostic of pancreatic cancer[3,4]. Despite a common etiology there is little data on the simultaneous occurrence of the two signs.
A 52-year-old male presented to the clinic with complaints of yellow discoloration of eyes and generalized pruritis since one month. He denied fever, chills or weight loss and maintained a normal appetite. He denied abdominal pain or backache. He quit smoking 15 years ago and denied consumption of alcohol. His past medical, surgical or family history were noncontributory. On examination he was icteric with no supraclavicular lymphadenopathy. Abdominal examination revealed a palpable liver edge 3 cm below the costal margin and a distended gall bladder consistent with a Courvoisier’s sign. Laboratory tests were remarkable for elevated liver function tests- total bilirubin 5.4 mg/dL, direct bilirubin 4.4 mg/dL, glutamic-oxalacetic transaminase (AST) 107 IU/L, alanine aminotransferase (ALT) 189 IU/L, alkaline phosphatase 489 U/L with a normal tumor marker CA 19-9.
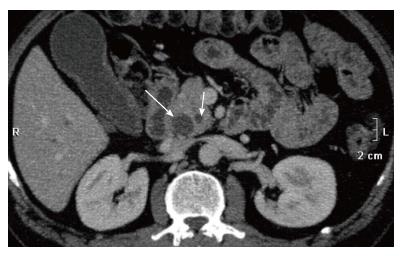
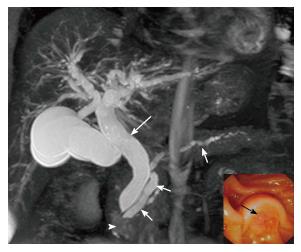
Abdominal ultrasound (US) demonstrated hepatomegaly, distended gallbladder with sludge, dilated MPD, CBD and intrahepatic biliary radicles. Pancreatic protocol computed tomography (CT) demonstrated a sessile enhancing mass in the medial wall of the second portion of the duodenum in the region of the ampulla with upstream dilation of the CBD, MPD, IHBR and a distended gallbladder. CBD and MPD measured 16 mm and 7 mm respectively and pancreatic parenchyma was normal (Figure 1). MR cholangiopancreatography confirmed an ampullary mass, a double duct sign with MPD dilated in its entire course and a prominent cystic duct (Figure 2). Upper gastrointestinal endoscopy demonstrated a periampullary tumor with surface ulceration and biopsy confirmed an adenocarcinoma (Figure 2, inset). The patient underwent a classic pancreaticoduodenectomy or Whipple operation. Postoperative course was unremarkable and the patient was discharged home on postoperative day six. Surgical pathology demonstrated a pT1N1M0 ampullary adenocarcinoma with vascular invasion. Adjuvant chemotherapy was administered and the patient remains without evidence of tumor recurrence at 18 mo following surgery.
The lack of gallbladder distension in 80.4% patients with calculous obstruction of the CBD was first reported by Courvoisier and is typically explained by fibrotic or atrophic changes in the gallbladder wall secondary to repeated inflammatory episodes however, recent data suggests that gallbladders are equally distensible regardless of the underlying pathology and it is the markedly higher and sustained elevation in ductal pressure in malignant obstruction that results in a distended gallbladder in contrast to the intermittent obstruction produced by gallstones[1,5,6]. The double duct sign initially described on endoscopic retrograde cholangiopancreatography (ERCP) has also been seen with US, CT or MRCP and is usually caused by cancer of the pancreatic head or ampulla of Vater and less commonly, chronic pancreatitis or ampullary stenosis[3]. Other malignant causes include cholangiocarcinoma, metastatic lymphadenopathy, lymphoma and rare causes include primary retroperitoneal fibrosis, Kaposi sarcoma or parasitic infestation of the bile ducts[3]. The prevalence of malignancy in patients with the double duct sign varies from 58%-85% particularly, in association with obstructive jaundice[4,7,8]. However, the MPD caliber is normal in 20% patients with pancreatic cancer and isolated dilation of the MPD (single duct dilation) is due to chronic pancreatitis in the majority of the patients[9,10].
Biductal obstruction of the CBD and MPD may result in the Courvoisier’s and/or double duct signs and the diagnostic value of these signs in the evaluation of a patient with obstructive jaundice is widely accepted. Despite extensive evaluation of the etiology, pathogenesis and mechanism of these signs no study has reported the incidence or prognostic significance of the simultaneous occurrence of these signs in a patient with an ampullary cancer. The impact of the simultaneous occurrence of the Courvoisier’s and double duct signs on survival outcome is unknown and an area for future investigation.
A 52-year-old male presented to the clinic with obstructive jaundice and abdominal examination revealed a palpable liver edge and a distended gall bladder consistent with the Courvoisier’s sign. Abdominal imaging revealed an ampullary mass and a double duct sign. Upper endoscopy and biopsy confirmed ampullary adenocarcinoma. A classic pancreaticoduodenectomy was performed. Postoperative recovery was uneventful and adjuvant chemotherapy was administered. The patient remains without evidence of tumor recurrence at 18 mo following surgery.
Obstructive jaundice with ampullary tumor.
Ampullary adenoma.
Blood investigations confirmed obstructive jaundice.
Triphasic computed tomography and magnetic resonance cholangiopancreatography confirmed an ampullary mass, a double duct sign with the common bile and main pancreatic ducts dilated in thier entire course.
Ampullary adenocarcinoma on esophagogastroduodenoscopy and biopsy.
A classic pancreaticoduodenectomy (Whipple Operation).
A double duct sign in a patient with obstructive jaundice is indicative of an ampullary tumor. A pancreaticoduodenectomy is potentially curative for ampullary adenocarcinoma.
This is a good clinical case report with good quality imaging studies to support the case.
| 1. | Ludwig Courvoisier (1843-1918). Courvoisier's sign. JAMA. 1968;204:627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Murphy K, McLaughlin P, O’Connor BR, Breen M, O’Súilleabháin C, Maceneaney P, Maher MM. Does Courvoisier’s sign stand the test of time? Clin Radiol. 2012;67:e27-e30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Ahualli J. The double duct sign. Radiology. 2007;244:314-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 42] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Menges M, Lerch MM, Zeitz M. The double duct sign in patients with malignant and benign pancreatic lesions. Gastrointest Endosc. 2000;52:74-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 44] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Chung RS. Pathogenesis of the “Courvoisier gallbladder”. Dig Dis Sci. 1983;28:33-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Fitzgerald JE, White MJ, Lobo DN. Courvoisier’s gallbladder: law or sign? World J Surg. 2009;33:886-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Kalady MF, Peterson B, Baillie J, Onaitis MW, Abdul-Wahab OI, Howden JK, Jowell PS, Branch MS, Clary BM, Pappas TN. Pancreatic duct strictures: identifying risk of malignancy. Ann Surg Oncol. 2004;11:581-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Krishna N, Tummala P, Reddy AV, Mehra M, Agarwal B. Dilation of both pancreatic duct and the common bile duct on computed tomography and magnetic resonance imaging scans in patients with or without obstructive jaundice. Pancreas. 2012;41:767-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Vitellas KM, Keogan MT, Spritzer CE, Nelson RC. MR cholangiopancreatography of bile and pancreatic duct abnormalities with emphasis on the single-shot fast spin-echo technique. Radiographics. 2000;20:939-957; quiz 1107-1108, 1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 100] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 10. | Edge MD, Hoteit M, Patel AP, Wang X, Baumgarten DA, Cai Q. Clinical significance of main pancreatic duct dilation on computed tomography: single and double duct dilation. World J Gastroenterol. 2007;13:1701-1705. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 45] [Cited by in RCA: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Imagawa A, John S S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ