Published online Jun 16, 2017. doi: 10.4253/wjge.v9.i6.267
Peer-review started: February 10, 2017
First decision: March 28, 2017
Revised: April 7, 2017
Accepted: May 3, 2017
Article in press: May 5, 2017
Published online: June 16, 2017
Processing time: 139 Days and 6.2 Hours
To describe a modified technique of deployment of stents using the overtube developed for balloon-assisted enteroscopy in post-sleeve gastrectomy (SG) complications.
Between January 2010 and December 2015, all patients submitted to an endoscopic stenting procedure to treat a post-SG stenosis or leakage were retrospectively collected. Procedures from patients in which the stent was deployed using the balloon-overtube-assisted modified over-the-wire (OTW) stenting technique were described. The technical success, corresponding to proper placement of the stent in the stomach resulting in exclusion of the SG leak or the stenosis, was evaluated. Complications related to stenting were also reported.
Five procedures were included to treat 2 staple line leaks and 3 stenoses. Two types of stents were used, including a fully covered self-expandable metal stent designed for the SG anatomy (Hanarostent, ECBB-30-240-090; M.I. Tech, Co., Ltd, Seoul, South Korea) in 4 procedures and a biodegradable stent (BD stent 019-10A-25/20/25-080, SX-ELLA, Hradec Kralove, Czech Republic) in the remaining procedure. In all cases, an overtube was advanced with the endoscope through the SG to the duodenum. After placement of the guidewire and removal of the endoscope, the stent was easily advanced through the overtube. The overtube was pulled back and the stent was successfully deployed under fluoroscopic guidance. Technical success was achieved in all patients.
The adoption of a modified technique of deployment of OTW stents using an overtube may represent an effective option in the approach of SG complications.
Core tip: Sleeve gastrectomy (SG) represents a type of bariatric surgery, whose postoperative complications include anastomotic leaks and strictures. Endoscopic treatment may encompass stenting, which may be technically challenging in angulated and tortuous SG anatomies. Furthermore, the delivery systems of some stents used in this indication are larger and less flexible. These aspects may result in recurrent kinking of the delivery system of the stent preventing its correct progression in the altered gastric cavity. Therefore, the adoption of a modified technique of deployment of stents using the overtube developed for balloon-assisted enteroscopy may represent an effective option to overcome those technical difficulties.
- Citation: Ponte A, Pinho R, Proença L, Silva J, Rodrigues J, Sousa M, Silva JC, Carvalho J. Utility of the balloon-overtube-assisted modified over-the-wire stenting technique to treat post-sleeve gastrectomy complications. World J Gastrointest Endosc 2017; 9(6): 267-272
- URL: https://www.wjgnet.com/1948-5190/full/v9/i6/267.htm
- DOI: https://dx.doi.org/10.4253/wjge.v9.i6.267
Sleeve gastrectomy (SG) represents one of the most commonly performed type of bariatric surgeries[1,2]. The increased number of SG has also lead to an increased prevalence of postoperative complications, namely anastomotic and staple line leaks and strictures[2]. The management of post-SG complications has also evolved and endoscopic treatment may currently play an important role in these patients[2]. Endoscopic treatment of staple line leaks and stenoses includes stenting, which may be technically challenging in angulated and tortuous SG anatomies. Furthermore, the delivery systems of some stents used in this indication are larger and less flexible. In some patients these difficulties may result in recurrent kinking of the delivery system of the stent preventing its correct progression in the stomach. Therefore, the adoption of a modified technique of deployment of stents using the overtube developed for balloon-assisted enteroscopy may represent an effective option to overcome those technical difficulties[3].
This study aims to describe a case series of patients with post-SG complications submitted to endoscopic stenting, in whom a conventional over-the-wire (OTW) technique failed and a modified OTW technique with the adaptation of an overtube was adopted.
Between January 2010 and December 2015, all patients submitted to an endoscopic stenting procedure to treat a post-SG stenosis or leakage were retrospectively collected. Procedures from patients in which the stent was deployed using the balloon-overtube-assisted (STSB1, Olympus) modified OTW stenting technique, after failure of the standard OTW stenting deployment, were described.
SG leaks were diagnosed based on clinical symptoms including fever and radiological evidence of fistula or abdominal abscesses. Patients were referred for stent placement only after resolution of sepsis and drainage of the abdominal collections. SG stenoses were diagnosed based on clinical symptoms including vomiting and endoscopic or barium studies revealing a narrowing of the stomach.
All procedures using the balloon-overtube assisted technique were performed under deep propofol sedation by two experienced endoscopists (RP and LP) with endoscopic and fluoroscopic guidance. Two types of stents were used, including a fully covered self-expandable metal stent (SEMS) designed for the SG anatomy (Hanarostent, ECBB-30-240-090; M.I. Tech, Co., Ltd, Seoul, South Korea) in four procedures and a biodegradable stent (BD stent 019-10A-25/20/25-080, SX-ELLA, Hradec Kralove, Czech Republic) in the remaining procedure. Informed consent was provided by all patients for this technique. The technical success, corresponding to proper placement of the stent in the stomach resulting in exclusion of the SG leak or the stenosis, was evaluated. Complications related to stenting were also reported.
During this period, 13 stents were placed to treat complications of SG, including anastomotic leaks (n = 6), stenoses (n = 4) and leaks associated with stenoses (n = 3). In 3 procedures, standard esophageal covered SEMS were used; in 1 procedure a biodegradable self-expandable stent was used and in the remaining 10 patients a covered SEMS specifically designed to the SG anatomy was used (Hanarostent, ECBB; M.I. Tech, Co., Ltd, Seoul, South Korea). These later 2 stents have a larger and stiffer delivery device that adds difficulty in the passage of angulations and stenosis, resulting in kinking and subsequent damage to the stent. In five (38%) of all procedures, representing 50% of patients (5/10) with these larger delivery devices, the presence of angulations and/or stenosis prevented the advancement of the stent delivery system (4 bariatric surgery stents and 1 biodegradable stent), precluding the standard OTW technique. In these 5 cases, the balloon-overtube-assisted modified OTW stenting technique was used to overcome these angulated stenoses. In Table 1 the characteristics of the five procedures are summarized.
| Procedure | SG complication | Reasons for failure of conventional OTW stenting | Type of stent | Technical success |
| 1 | Dehiscence | Angulation in the antrum | Bariatric SEMS | Yes |
| 2 | Dehiscence | Angulation in the antrum | Bariatric SEMS | Yes |
| 3 | Stenosis | Long and angulated stenosis in the antrum | Biodegradable stent | Yes |
| 4 | Stenosis | Angulated stenosis in the antrum | Bariatric SEMS | Yes |
| 5 | Stenosis | Angulated stenosis in the antrum | Bariatric SEMS | Yes |
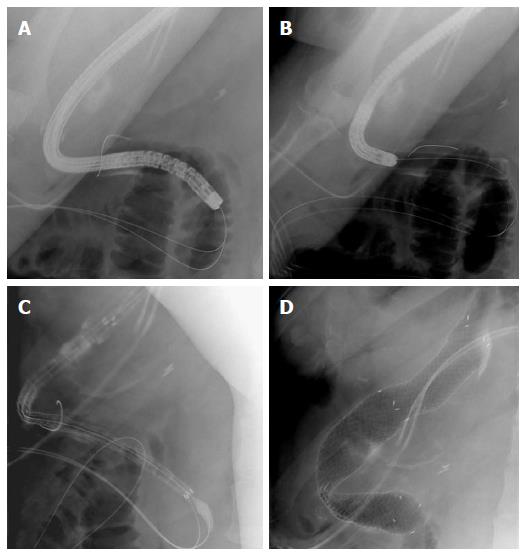
This patient was referred for our department to treat a large early leak post-SG in the proximal antrum. Endoscopy revealed a 30-mm dehiscence in the proximal antrum and a marked angulation in the distal antrum. This angulation caused persistent kinking of the delivery device, preventing the technical success of stenting using the standard OTW approach. Hence, an overtube was used to overcome the initial difficulties. The overtube and endoscope were advanced through the SG to the duodenum (Figure 1A). After placement of the guidewire and removal of the endoscope leaving the overtube in place (Figure 1B), a fully covered SEMS (Hanarostent, ECBB-30-240-090; M.I. Tech, Co., Ltd, Seoul, South Korea) was easily advanced through the overtube (Figure 1C). The overtube was then pulled back and the stent was successfully deployed under fluoroscopic guidance (Figure 1D). Correct placement of the stent was confirmed by injection of contrast revealing no extravasation of contrast through the leak. No immediate or late complications related to the stent were reported.
This procedure was performed to treat early dehiscences post-SG. Endoscopy revealed 3 small leaks, one located in the proximal body and two located in the proximal antrum. The angulated configuration of the SG caused repeated kinking preventing the advancement of the stent using the standard OTW technique. Therefore, an overtube was used and was advanced with the endoscope through the SG to the duodenum. After placement of the guidewire up to the duodenum and removal of the endoscope leaving the overtube in place, a fully covered SEMS (Hanarostent, ECBB-30-240-090; M.I. Tech, Co., Ltd, Seoul, South Korea) was easily advanced through the overtube that was left in situ. The overtube was then pulled back and the stent was successfully deployed under fluoroscopic guidance. Correct placement of the stent was confirmed endoscopically and with fluoroscopy that showed no extravasation of contrast through the leak.
This patient was referred to our department to stent a chronic fibrotic stenosis post-SG in the distal antrum refractory to balloon dilation. The stenosis was 4-cm long and angulated, which prevented the advancement of the stent’s delivery system using the standard OTW technique. Before stenting, the fibrotic stenosis was dilated using a controlled radial expansion balloon with a diameter up to 15 mm. Then, the limits of the stenosis were marked using submucosal contrast injection and the endoscope mounted with the overtube was advanced to the duodenum. The guidewire was then inserted to the jejunum and the endoscope was removed, leaving the overtube through the stenosis. A biodegradable stent (BD stent 019-10A-25/20/25-080, SX-ELLA, Hradec Kralove, Czech Republic) was used, which was advanced through the overtube under fluoroscopic guidance. Then the overtube was split and removed, and the stent was successfully deployed under fluoroscopic guidance. The luminal patency was confirmed with injection of contrast which progressed easily to the jejunum.
This patient was submitted to a SG which complicated with a stenosis. Firstly, serial balloon dilations were attempted with no clinical success. Therefore, the patient underwent endoscopy to place a stent. The stenosis was dilated with a balloon up to 15 mm. The angulation of the stenosis in the antrum resulted in recurrent kinking of thedelivery system, preventing the advancement of the stent using the standard OTW technique. The overtube-assisted modified OTW stenting technique previously described was then used enabling the advancement of the endoscope and overtube to the duodenum, after delimitation of the limits of the stenosis. The guidewire was subsequently advanced, the endoscope was removed and the overtube was left through the angulation. A fully covered SEMS (Hanarostent, ECBB-30-240-090; M.I. Tech, Co., Ltd, Seoul, South Korea) was then advanced through the overtube, under fluoroscopic guidance. The overtube was slightly pulled back to prevent the release of the stent in its interior, and finally the stent was deployed under fluoroscopic guidance. Luminal patency was confirmed with administration of oral contrast. Three weeks later, stent migration occurred due to dilation of the stenosis caused by the stent, requiring endoscopic retrieval of the stent.
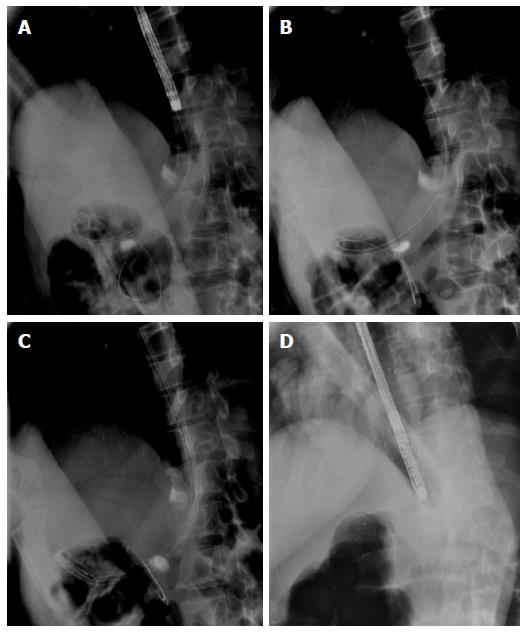
This patient underwent an overtube-assisted modified OTW stenting technique to treat a chronic and angulated stenosis post-SG refractory to balloon dilation. The configuration and angulation of the stenosis prevented the technical success of the standard OTW technique and the modified technique described above using the overtube was adopted. As in procedure 4, after delimitation of the limits of the stenosis with submucosal contrast injection, the overtube and endoscope were advanced through the stenosis to the duodenum. After placement of the guidewire and removal of the endoscope (Figure 2A and B), the fully covered SEMS (Hanarostent, ECBB-30-240-090; M.I. Tech, Co., Ltd, Seoul, South Korea) was easily advanced through the overtube (Figure 2C). The overtube was then pulled back and the stent was successfully deployed under fluoroscopic guidance (Figure 2D). No immediate or late complications related to the stent were reported.
Laparoscopic SG is a new surgical procedure for morbid obesity that has gained wide acceptance due to its simplicity and efficacy compared to the gastric bypass technique[4]. Nevertheless, its long staple line and altered intragastric pressures may lead to postoperative complications, including staple line leaks and stenoses[5].
The main early postoperative complication after SG is staple line leak, which affects 0.5%-5% of the patients and typically occurs in the proximal third of the stomach, near the gastroesophageal junction[1,4,6]. Clinical suspicion and imaging are the cornerstone in the diagnosis[1]. Patients may present with fever, tachycardia, abdominal pain, peritonitis, septic shock and multiorgan failure or may be asymptomatic[1,7,8]. Tachycardia is the earliest sign of a possible leak[8]. Management mainly depends on the timing and clinical presentation of the leak, being a new surgical approach indicated in septic or hemodynamically unstable patients[1,6-9]. After controlling the septic state, efforts must be focused on healing the gastric leak and various endoscopic techniques have been successfully applied, namely endoclips, fibrin glue, over-the-scope clips, septotomy combined with balloon dilation and covered stents[2,4,6,8,10-13]. Covered stents are a novel treatment approach for leaks after bariatric surgery, being minimally invasive, relatively safe and successful in 88% of cases[4,7,9]. Post-SG stenoses range from 0.26% to 4% and may result from a prior leak or anastomotic ulceration, unintentional narrow gastric tubularization, a twisted or spiral suture and segmental imbrication[2,5]. Segmental imbrication usually results in stenoses at the level of the incisura due to the retraction of tissues[5]. The diagnosis is based on clinical symptoms including vomiting and endoscopic or barium studies revealing a narrowing of the stomach[6]. Endoscopic therapy may encompass balloon dilation and stenting to prevent restenosis[2].
Endoluminal stents provide a physical barrier between the gastric lumen and the leak, preventing further peritoneal contamination and allowing its healing while affording enteral nutrition[2,8]. The main limitations of stent employment are distal migration and mucosal hypertrophy[7-9]. The SEMS used in 4 procedures of our series may obviate these complications as it was specifically designed for bariatric surgery allowing better adjustment to the anatomy of the SG and it is fully covered preventing mucosal hypertrophy.
The placement of self-expanding stents is usually easily accomplished, using either the through-the-scope (TTS) or the OTW technique. The TTS technique is easier to perform in stenoses that are angulated or located after sharp angulations. Nevertheless, some stents as the models used in our case series have a larger delivery system, which prevents the use of the TTS technique. Furthermore, this stent is larger and stiffer than usual SEMS, turning its advancement over angulated stenoses challenging. Conversely, as occurred with these stents in 50% of patients (5/10) in our case series, the conventional OTW procedure may not be technically successful due to recurrent kinking or looping of the delivery system in an angulated stenosis. To overcome these limitations, the adaptation of an overtube to the OTW technique may prevent kinking of the delivery system as the overtube will have a role similar to a working channel[3,14,15]. In our case series, this technical modification of the OTW procedure resulted in technical success in all cases.
In conclusion, this modified overtube-assisted OTW technique represents a safe and easy method for stent insertion in challenging SG anatomies, allowing the placement of different models of stents and the technical success in all 5 procedures.
Sleeve gastrectomy (SG) represents a type of bariatric surgery, whose postoperative complications include anastomotic leaks and strictures. Endoscopic treatment of staple line leaks and stenoses includes stenting, which may be technically challenging in angulated and tortuous SG anatomies. Furthermore, the delivery systems of some stents used in this indication are larger and less flexible preventing the through-the-scope stenting technique. In some patients these difficulties may result in recurrent kinking of the delivery system of the stent preventing its correct progression over-the-wire (OTW) in the stomach.
The adoption of a modified technique of deployment of stents OTW using the overtube developed for balloon-assisted enteroscopy may represent an effective option to overcome technical difficulties of stenting deployment.
The adaptation of an overtube to the OTW technique may prevent kinking of the delivery system as the overtube will have a role similar to a working channel. The overtube-assisted modified OTW stenting technique enables the advancement of the endoscope and overtube through the SG to the duodenum. The guidewire is subsequently advanced, the endoscope removed and the overtube is left in place. The stent is then advanced through the overtube, under fluoroscopic guidance. The overtube is slightly pulled back to prevent the release of the stent in its interior, and finally the stent is deployed under fluoroscopic guidance.
The modified overtube-assisted OTW technique represents a safe and easy method for stent insertion in challenging SG anatomies and a good option in cases of conventional OTW stenting failure.
SG is a type of bariatric surgery resulting in tubulization of the gastric cavity.
The most interesting topic of the paper is the novelty of the technique described. This technique seems easy to perform, in expert hand, and can impact positively on the resolution of serious complications due to laparoscopic SG.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Portugal
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Fogli L, Galloro G, Ziogas DE S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Tringali A, Bove V, Perri V, Landi R, Familiari P, Boškoski I, Costamagna G. Endoscopic treatment of post-laparoscopic sleeve gastrectomy leaks using a specifically designed metal stent. Endoscopy. 2017;49:64-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Puig CA, Waked TM, Baron TH, Wong Kee Song LM, Gutierrez J, Sarr MG. The role of endoscopic stents in the management of chronic anastomotic and staple line leaks and chronic strictures after bariatric surgery. Surg Obes Relat Dis. 2014;10:613-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 3. | Pinho R, Proença L, Ponte A, Fernandes C, da Ribeiro I, Silva J, Carvalho J. Balloon overtube-assisted stenting in difficult upper and lower gastrointestinal locations using a modified over-the-wire technique. Endoscopy. 2015;47:266-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 4. | Ponte A, Pinho R, Proença L. Modified positioning of a bariatric surgery stent to manage an atypical staple line leak after sleeve gastrectomy. Clin Gastroenterol Hepatol. 2015;13:e23-e24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Parikh A, Alley JB, Peterson RM, Harnisch MC, Pfluke JM, Tapper DM, Fenton SJ. Management options for symptomatic stenosis after laparoscopic vertical sleeve gastrectomy in the morbidly obese. Surg Endosc. 2012;26:738-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 99] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 6. | Rebibo L, Hakim S, Brazier F, Dhahri A, Cosse C, Regimbeau JM. New endoscopic technique for the treatment of large gastric fistula or gastric stenosis associated with gastric leaks after sleeve gastrectomy. Surg Obes Relat Dis. 2016;12:1577-1584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Simon F, Siciliano I, Gillet A, Castel B, Coffin B, Msika S. Gastric leak after laparoscopic sleeve gastrectomy: early covered self-expandable stent reduces healing time. Obes Surg. 2013;23:687-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 71] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 8. | de Aretxabala X, Leon J, Wiedmaier G, Turu I, Ovalle C, Maluenda F, Gonzalez C, Humphrey J, Hurtado M, Benavides C. Gastric leak after sleeve gastrectomy: analysis of its management. Obes Surg. 2011;21:1232-1237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 74] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 9. | Puli SR, Spofford IS, Thompson CC. Use of self-expandable stents in the treatment of bariatric surgery leaks: a systematic review and meta-analysis. Gastrointest Endosc. 2012;75:287-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 124] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 10. | Sakran N, Goitein D, Raziel A, Keidar A, Beglaibter N, Grinbaum R, Matter I, Alfici R, Mahajna A, Waksman I. Gastric leaks after sleeve gastrectomy: a multicenter experience with 2,834 patients. Surg Endosc. 2013;27:240-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 287] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 11. | Shnell M, Gluck N, Abu-Abeid S, Santo E, Fishman S. Use of endoscopic septotomy for the treatment of late staple-line leaks after laparoscopic sleeve gastrectomy. Endoscopy. 2017;49:59-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Haito-Chavez Y, Kumbhari V, Ngamruengphong S, De Moura DT, El Zein M, Vieira M, Aguila G, Khashab MA. Septotomy: an adjunct endoscopic treatment for post-sleeve gastrectomy fistulas. Gastrointest Endosc. 2016;83:456-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Campos JM, Ferreira FC, Teixeira AF, Lima JS, Moon RC, D’Assunção MA, Neto MG. Septotomy and Balloon Dilation to Treat Chronic Leak After Sleeve Gastrectomy: Technical Principles. Obes Surg. 2016;26:1992-1993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 14. | Ponte A, Pinho R, Rodrigues A, Proença L, Costa A, Carvalho J. Jejunal Stent-in-Stent for Recurrent Malignant Occlusion Using Single-Balloon Enteroscopy. GE Port J Gastroenterol. 2016; Epub ahead of print. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Ponte A, Pinho R, Proença L, Bernardes C, Costa A, Francisco E, Carvalho J. Palliative stenting of a jejunal stricture secondary to malignant compression using single-balloon enteroscopy. Gastroenterol Hepatol. 2016; Jul 30; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |