Published online Feb 25, 2016. doi: 10.4253/wjge.v8.i4.205
Peer-review started: May 7, 2015
First decision: July 22, 2015
Revised: September 30, 2015
Accepted: December 17, 2015
Article in press: December 18, 2015
Published online: February 25, 2016
Processing time: 298 Days and 6.1 Hours
New endoscopic techniques for hemostasis in nonvariceal bleeding were introduced and known methods further improved. Hemospray and Endoclot are two new compounds for topical treatment of bleeding. Initial studies in this area have shown a good hemostatic effect, especially in active large scale oozing bleeding, e.g., tumor bleedings. For further evaluation larger prospective studies comparing the substanced with other methods of endoscopic hemostasis are needed. For localized active arterial bleeding primary injection therapy in the area of bleeding as well as in the four adjacent quadrants offers a good method to reduce bleeding activity. The injection is technically easy to learn and practicable. After bleeding activity is reduced the bleeding source can be localized more clearly for clip application. Today many different through-the-scope (TTS) clips are available. The ability to close and reopen a clip can aid towards good positioning at the bleeding site. Even more important is the rotatability of a clip before application. Often multiple TTS clips are required for secure closure of a bleeding vessel. One model has the ability to use three clips in series without changing the applicator. Severe arterial bleeding from vessels larger than 2 mm is often unmanageable with these conventional methods. Here is the over-the-scope-clip system another newly available method. It is similar to the ligation of esophageal varices and involves aspiration of tissue into a transparent cap before closure of the clip. Thus a greater vascular occlusion pressure can be achieved and larger vessels can be treated endoscopically. Patients with severe arterial bleeding from the upper gastrointestinal tract have a very high rate of recurrence after initial endoscopic treatment. These patients should always be managed in an interdisciplinary team of interventional radiologist and surgeons.
Core tip: An increasing rate of patients who present with nonvariceal hemorrhage present with an anticoagulative or antithrombotic medication. Often the patient suffers from concomitant disease. In the recent years new methods for flexible endoscopic treatment of hemorrhage have been developed. The following article discusses the current literature of the new endoscopic methods in the context of every day practice in endoscopic treatment for nonvariceal hemorrhage.
- Citation: Goelder SK, Brueckner J, Messmann H. Endoscopic hemostasis state of the art - Nonvariceal bleeding. World J Gastrointest Endosc 2016; 8(4): 205-211
- URL: https://www.wjgnet.com/1948-5190/full/v8/i4/205.htm
- DOI: https://dx.doi.org/10.4253/wjge.v8.i4.205
Endoscopic hemostatic treatment is the gold standard for active gastrointestinal bleeding, as well as for recent bleeding with stigmata of a high recurrence rate. International treatment guidelines recommend an early risk stratification by immediate endoscopic diagnosis and treatment[1]. Injection therapy, clip application and thermal hemostasis are well established methods of mono therapies. However a combination of two hemostatic methods have been found to be superior to an individual method alone and should therefore be preferred[2]. Mechanical hemostasis with clips can be limited due to poor angulation and mobility of the endoscope, e.g., in the duodenal bulb. Also some conventional clips cannot be reopened after closing even after poor placement.
In this review we highlight recent innovations in the field of endoscopic hemostasis in nonvariceal bleeding in the upper gastrointestinal tract with a focus on new topically applied substances (e.g., Ankafer, Hemospray and EndoClot) and newly developed clips [instinct clip and over-the-scope-clip (OTSC)].
Before endoscopic treatment of a nonvariceal bleeding certain factors that correlate with a high rate of rebleeding, should be considered. Interdisciplinary solutions should be evaluated at an early stage. Ogasawara et al[3] described in a single center retrospective study the parameters: Age > 70 years, hemorrhagic shock on admission, hemoglobin < 8 mg/dL, serum albumin < 3.3 g/dL, vessels > 2 mm and Forrest Ia and Ib ulcers as negative predictors. The strongest predictors of failure of endoscopic therapy is a vessel diameter > 2 mm (OR = 4:38; 95%CI: 1.25-7.01) and the presence of hemorrhagic shock (OR = 5.26, 95%CI: 2.43-11.6)[3].
The authors describe precisely the approach when initial hemostasis fails. From 2000-2010, n = 428 patients were treated with Forrest Ia/Ib (FIa/FIb) and Forrest IIa/b (FIIa/FIIb) lesions. The authors describe a standardized second-look endoscopy after 24 h in all patients. A recurrent bleeding occurred in 69 (16%) of the patients. Twelve percent of those received surgery, 4% died. For the entire population of 428 patients with FIa/FIb and FIIa/FIIb bleeding endoscopic failure rate of 17/428 (4%).
The second endoscopic hemostasis was successful in 46/69 (66.7%). A third intervention was successful in 11/23 (47.8%) of the patients. With this approach, the authors were able to treat 57/69 (82%) recurrences during follow-up.
This work shows that by endoscopic hemostasis a large proportion of patients with upper nonvariceal gastrointestinal bleeding can be permanently treated with the first endoscopic hemostasis.
Attention should be paid to the special situation of a large visible vessel (> 2 mm). Especially arterial vessels on the posterior wall of the duodenal bulb should gain attention. Surprisingly, the proportion of intractable bleeding in the study of Ogasawara et al[3] were more frequent in the duodenal bulb, but this did not reach statistical significance.
Another crucial parameter before starting any endoscopic therapy in the presence of bleeding is the fact that especially non-bleeding-related comorbidities cause the mortality of non variceal bleeding[4]. The number of comorbidities and the probably of taking anticoagulative or antithrombotic drugs will affect decisively the prognosis in the individual cases.
Surface bleeding provides a problem for common hemostatic methods. Injections work better with localized active bleeding sources. Also, after injection of NaCl or diluted epinephrine solution a decongestion of the injected volume cause a reactivation of bleeding. Mechanical hemostatic methods can cannot easily be used for diffuse mucosal bleeding. Hemostasis with argon plasma coagulation would be the method of choice but a High Frequency (HF) Generator is required, which must be frequently initially activated in emergency examinations or on the intensive care unit.
Over the past 50 years, various substances for topical hemostasis were developed especially in open surgery. Bergel in 1909 described the application of fibrin to accelerate hemostasis. Other locally applied substances include thrombin clotting factors and sucralfate, which have been described with differing results in small case series[5].
Currently the literature describes three substances, used for endoscopic hemostasis (Table 1). Hemospray (Cook Medical, Limerik, Ireland) and EndoClot (EPI, Santa Clara CA, United States) are eligible for endoscopic treatment of nonvariceal bleeding. The preparation of ankaferd [ankaferd blood stopper (ABS)] is not available for endoscopic hemostasis in Germany.
| Contains | Mechanism of action | Approved human application | Formulation | |
| Ankaferd blood stopper | Herbal mixture | Forms protein networks, activates clotting cascade | Dental procedures, first aid services | Tampons, sprays, ampoules |
| Hemospray | Mineral powder | Absorbs H2O, mechanical tamponade, activates clotting cascade | Nonvariceal GI bleeding | CO2 pressurized handheld canister (20 g) |
| EndoClot | Absorbable polymere | Absorbs H2O and concentrate cells, activates clotting cascade | Adjuvant hemostatic therapy | Pressurized air compressor |
ABS is a preparation of Turkish medicine, specified by the manufacturer as a blend of vegetable ingredients. A preparation of 100 mL of ABS is composed of a standardized mixture of plants, including 5 mg Thymus vulgaris (dried grass extract), 9 mg Glycyrrhiza glaba (dried leaf extract), 8 mg Vitis vinifera (dried leaf extract), 7 mg Alpinia officinarum (dried leaf extract), and 6 mg Urtica dioica (dried root extract)[6].
The endoscopic application of ABS is published in case reports and series for treatment of Mallory-Weiss tears, Dieulafoy ulcers, GAVE, anastomotic bleeding, post sphincterotomy and tumor bleeding[7]. Prospective randomized trials compairing ABS to other endoscopic hemostasis procedures are lacking.
Hemospray (also named TC-325) is a mineral-based powder from Cook Medical Limerick Irland. It was developed by the armed forces for control of bleeding in military operations. The powder is applied via a CO2 pressurized handle. The powder is sprayed onto the source of bleeding and it is important for the application that an active bleeding is present. Only then the effect of the substance can occur.
In an animal model with an artificial arterial bleeding in the stomach, endoscopic hemostasis could successfully be achieved[8]. There was no evidence for an embolic removal of the substance into the circulatory system or local reactions at the site of bleeding. Sung et al[9] reported 2011 on the first application of hemostasis for n = 20 patients with peptic ulcer bleeding. The acute hemostasis rate was 95% (19/20). One patient with a FIa hemorrhage had to be embolized radiologically due to a pseudoaneurysm. Out of the patients with a successful initial treatment, 2/10 (11%) showed a recurrence of bleeding within 72 h, however these could again be treated endoscopically[9].
In 2013, the results of the “Evaluate Survey of the Application of Hemospray in the luminal tract”, a European database, were published[10]. The authors report on n = 30 patients with peptic ulcers and n = 33 patients with other nonvariceal bleeding sources (e.g., post EMR, tumor bleeding, Dieulafouy ulcer). Monotherapy with Hemospray was carried out in 87%. The primary hemostasis rate was 85%. A rebleeding within 7 d occurred in 15% of all treated patients. In 8 cases Hemospray was applied adjuvantly after ineffective primary hemostasis with other methods. In all eight cases, treatment with Hemospray was successful, however, rebleeding occurred in 25%.
Another typical indication for Hemospray are large diffuse tumor bleedings. Chen et al[11] described the successful treatment of n = 5 patients with different tumor bleedings. Binkau et al[12] successfully treated two cases of an ulcerated carcinoma of the stomach and one case of small cell lung cancer, with bleeding from a metastasis in the stomach. The advantage of Hemospray is the contact-free application of the substance to a diffusely bleeding tumor surface. Upon blood contact, local hemostasis is accelerated (Figure 1).
EndoClot contains absorbable polysaccharide particles, which are polysaccharides that absorb the blood fluid and form a gel to accelerate coagulation.
The substance is applied over a catheter with an air compressor. During application, the catheter tip has to be held at a distance from the bleeding source in order to prevent blockage of the catheter.
Müller-Gerbes et al[13] report their experience of treating 22 patients either with EndoClot alone (17 patients) or in combination with other hemostatic methods (5 patients). Overall, hemostasis was successful in 21/22 patients. Out of these cases 8 involved diffuse tumor bleeding which could be stopped.
However, Holster et al[14] could report sufficient hemostasis in patients with active arterial bleeding who were under anticoagulants.
Overall topically applied substances are particularly helpful for diffuse bleedings with low activity and without a clearly localized source. Also, patients taking anticoagulants or antithrombotic medication can well be treated with the new substances. Other indications such as arterial bleeding have shown less favorable results. In order to more firmly establish topically applied substances in the algorithm of endoscopic hemostatic therapy, larger studies comparing them to conventional methods are at need.
If positioning of the endsocope is adequate and the endoscopic team is clip-experienced, a mechanical method for hemostasis could be preferred. For this modality new clip models were presented in recent years.
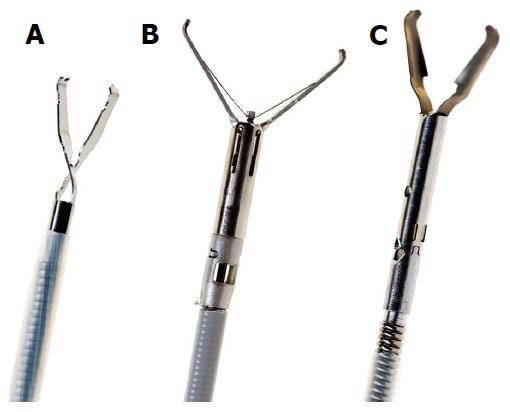
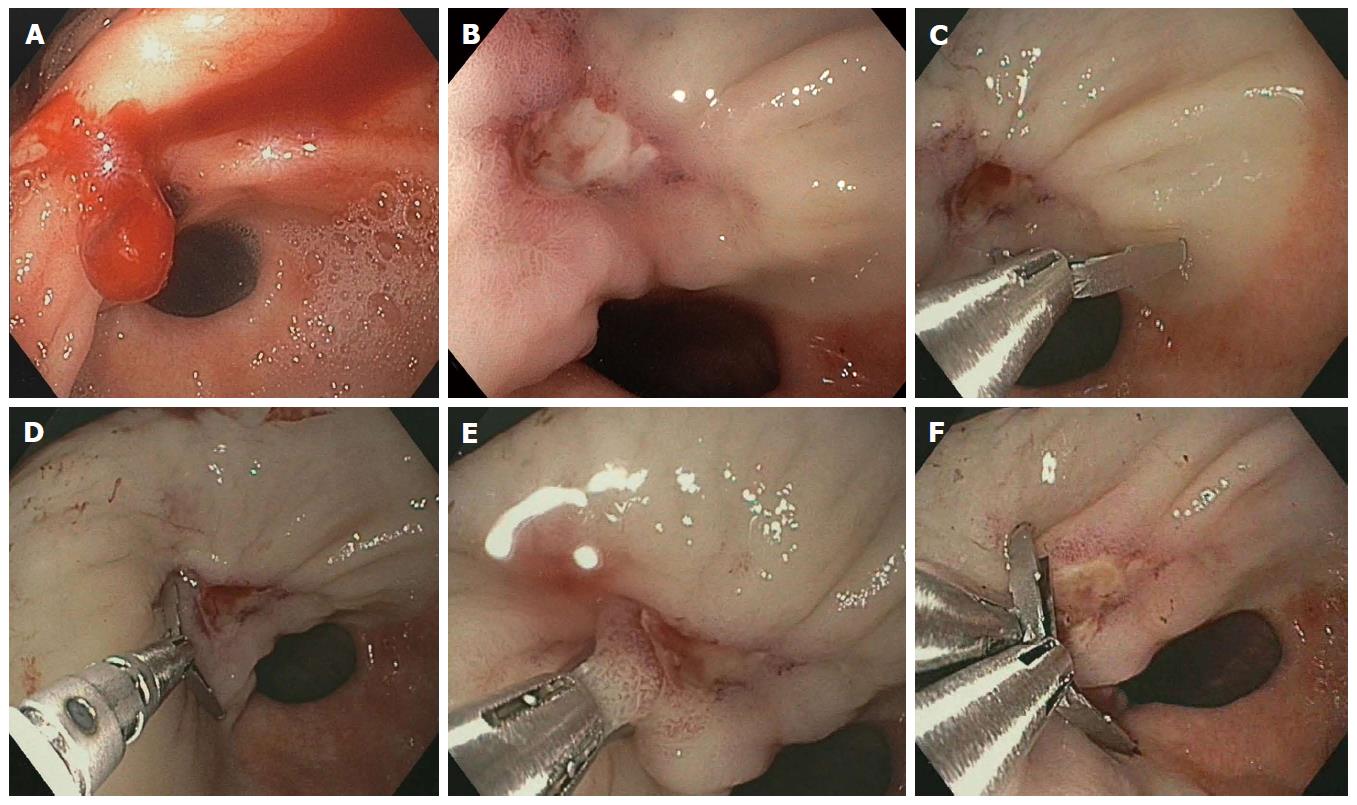
There are two groups of clips: Clips applied through the working channel of an endoscope [Through-the-Scope (TTS)] and clips pre-loaded with a transparent detachable cap at the distal end of the endoscope (over the scope OTSC) (Figure 2).
The TTS clips are available from different manufacturers and with different opening lengths (Table 2, Figures 3 and 4). A clip with three branches (TriClip, Cook Medical, Ireland) is now no longer available. Prospective studies with the TriClip compared to the Quick Clip (Olympus, Hamburg, Germany) showed a slightly worse outcome for the TriClip. Another study showed more recurrent bleeding with the TriClip (15% vs 29%). The primary hemostasis rate was also significantly lower with the TriClip (94% vs 76%, P = 0.01)[15].
| Clip | Manufacturer | Opening with | Special |
| Clipmaster 3 | Medwork, Höchstadt/Aisch, Germany | 12 mm | 3 clips in a row - no change of the applicator required |
| Quick clip 2 | Olympus, Hamburg, Germany | 9 mm | Multiple use applicator |
| Quick clip 2 long | Olympus, Hamburg, Germany | 11 mm | Multiple use applicator |
| Resolution clip | Boston Scientific, Ratingen, Germany | 11 mm | Reopenable after placement |
| Instinct clip | Cook Medical, Limerick, Ireland | 16 mm | Reopenable after placement |
Meanwhile the company has improved the clip model and offers a clip with two branches. It is called “instinct clip”, opens at a very wide angle, can be rotated and reopened. However it is a single use clip, requiring a complete application set for each application. So far there are no published clinical trials. However, an ex vivo study showed a good application even in full inversion of the endoscope and a durable tissue closure (Figure 5)[16].
The mechanical hemostasis is the only endoscopic procedure that offers a safe and permanent closure of larger vessels[17]. However, the exact placement on the bleeding source and the durability of the clip until hemostasis has occurred are important.
Hepworth et al[18] compared the methods of endoscopic injection, heater probe thermal treatment, and clip application in an animal model on arterial vessels of different diameter. The injection could not achieve permanent hemostasis in any vessel diameter (1-3 mm). But even with the state of the art hemostasis clips, the authors were only able to achieve permanent hemostasis in 10%-15% of the cases. The attempt to achieve a higher hemostasis rate with an endoscopic suture or an endoloop achieved more durable vascular occlusion. Another ex vivo study was performed on the “Erlangen Active Simulator for Interventional Endoscopy” and measured the closing pressure after endoscopic application of different clip models. The maximum closure pressure of 200 mmHg was achieved in 59% with the OTSC system. The resolution clip (Boston Scientific, Ratingen, Germany) accomplished this in 10%, quick clip (Olympus, Hamburg, Germany) 3% and in TriClip (Cook, Limerick, Irland) in 10%. With injection alone, the maximum occlusion pressure has been reached in 5% of the tests. The authors conclude from their experimental results that arterial vessels greater than 2 mm can only be closed with the OTSC System[19].
Another benefit of the OTSC System could be a circular grasp of the bleeding source and the surrounding tissue containing the supplying blood vessels. Kirschniak et al[20] reported the first clinical experience with the OTSC clip for hemostasis.
The clip was used for primary or postoperative bleeding in the gastrointestinal tract. In all seven patients in whom the clip was used for endoscopic hemostasis, the primary hemostasis was successful and there was no recurrent bleeding. Another series of 30 cases in which the conventional methods of endoscopic hemostasis had failed, use of the OTSC system achieved a success rate of 97% of primary hemostasis[21]. In two cases there was recurrent bleeding, which could be treated with repeated endoscopic treatment. In a recent case series, a technical success rate of 100% for hemostasis with the OTSC clip is reported. In two cases a rebleeding occurred, in one of which the source of bleeding was a multiply pretreated tumor[22].
In recent years, new techniques for endoscopic hemostasis were introduced and known methods further improved.
With Hemospray and EndoClot two new compounds for topical treatment are available. Initial studies in this area have shown a good hemostatic effect, especially in active large scale oozing bleeding, e.g., tumor bleedings. For further evaluation larger prospective studies comparing the substanced with other methods of endoscopic hemostasis are needed.
For localized active arterial bleeding, primary injection therapy in the area of bleeding as well as in the four adjacent quadrants offers a good method to reduce bleeding activity. The injection is technically quite easy to learn and practicable. After bleeding activity is reduced the bleeding source can be localized more easily for clip application. Today many different TTS clips are available. The ability to close and reopen a clip can aid towards good positioning at the bleeding site. Even more important is the rotatability of a clip before application. Often multiple TTS clips are required for secure closure of a bleeding vessel. One model has the ability to use three clips in series without changing the applicator.
Severe arterial bleeding from vessels larger than 2 mm is often unmanageable with these conventional methods. Here the OTSC system is a newly available method. Its mechanism is similar to the ligation of esophageal varices and involves aspiration of tissue into a transparent cap before closure of the clip. Thus a greater vascular occlusion pressure can be achieved and larger vessels can be treated endoscopically. Patients with severe arterial bleeding from the upper gastrointestinal tract have a very high rate of recurrence after initial endoscopic treatment. These patients should always be managed in an interdisciplinary team of interventional radiologist and surgeons.
| 1. | Barkun AN, Bardou M, Kuipers EJ, Sung J, Hunt RH, Martel M, Sinclair P. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010;152:101-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 840] [Cited by in RCA: 716] [Article Influence: 44.8] [Reference Citation Analysis (1)] |
| 2. | Vergara M, Calvet X, Gisbert JP. Epinephrine injection versus epinephrine injection and a second endoscopic method in high risk bleeding ulcers. Cochrane Database Syst Rev. 2007;CD005584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Ogasawara N, Mizuno M, Masui R, Kondo Y, Yamaguchi Y, Yanamoto K, Noda H, Okaniwa N, Sasaki M, Kasugai K. Predictive factors for intractability to endoscopic hemostasis in the treatment of bleeding gastroduodenal peptic ulcers in Japanese patients. Clin Endosc. 2014;47:162-173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Sung JJ, Tsoi KK, Ma TK, Yung MY, Lau JY, Chiu PW. Causes of mortality in patients with peptic ulcer bleeding: a prospective cohort study of 10,428 cases. Am J Gastroenterol. 2010;105:84-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 213] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 5. | Barkun AN, Moosavi S, Martel M. Topical hemostatic agents: a systematic review with particular emphasis on endoscopic application in GI bleeding. Gastrointest Endosc. 2013;77:692-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 92] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 6. | Goker H, Haznedaroglu IC, Ercetin S, Kirazli S, Akman U, Ozturk Y, Firat HC. Haemostatic actions of the folkloric medicinal plant extract Ankaferd Blood Stopper. J Int Med Res. 2008;36:163-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 167] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 7. | Wong Kee Song LM, Banerjee S, Barth BA, Bhat Y, Desilets D, Gottlieb KT, Maple JT, Pfau PR, Pleskow DK, Siddiqui UD. Emerging technologies for endoscopic hemostasis. Gastrointest Endosc. 2012;75:933-937. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Giday SA, Kim Y, Krishnamurty DM, Ducharme R, Liang DB, Shin EJ, Dray X, Hutcheon D, Moskowitz K, Donatelli G. Long-term randomized controlled trial of a novel nanopowder hemostatic agent (TC-325) for control of severe arterial upper gastrointestinal bleeding in a porcine model. Endoscopy. 2011;43:296-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Sung JJ, Luo D, Wu JC, Ching JY, Chan FK, Lau JY, Mack S, Ducharme R, Okolo P, Canto M. Early clinical experience of the safety and effectiveness of Hemospray in achieving hemostasis in patients with acute peptic ulcer bleeding. Endoscopy. 2011;43:291-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 165] [Article Influence: 11.0] [Reference Citation Analysis (1)] |
| 10. | Smith LA, Stanley AJ, Bergman JJ, Kiesslich R, Hoffman A, Tjwa ET, Kuipers EJ, von Holstein CS, Oberg S, Brullet E. Hemospray application in nonvariceal upper gastrointestinal bleeding: results of the Survey to Evaluate the Application of Hemospray in the Luminal Tract. J Clin Gastroenterol. 2013;48:e89-e92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 89] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 11. | Chen YI, Barkun AN, Soulellis C, Mayrand S, Ghali P. Use of the endoscopically applied hemostatic powder TC-325 in cancer-related upper GI hemorrhage: preliminary experience (with video). Gastrointest Endosc. 2012;75:1278-1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Binkau J, Nötzel E, Hartmann D. TC-325-Applikation (Hemospray®-Device) zur endoskopischen Blutstillung bei Tumorblutungen - zwei Kasuistiken. Endo heute. 2013;26:259-262. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Müller-Gerbes D, Beeck A, Dormann A. Hämostase mit Pulver - Erfahrungen mit EndoClotTM bei schwierigen oberen GI-Blutungen. Endo heute. 2013;26:254-258. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Holster IL, Kuipers EJ, Tjwa ET. Hemospray in the treatment of upper gastrointestinal hemorrhage in patients on antithrombotic therapy. Endoscopy. 2013;45:63-66. [PubMed] |
| 15. | Lin HJ, Lo WC, Cheng YC, Perng CL. Endoscopic hemoclip versus triclip placement in patients with high-risk peptic ulcer bleeding. Am J Gastroenterol. 2007;102:539-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Daram SR, Tang SJ, Wu R, To SD. Benchtop testing and comparisons among three types of through-the-scope endoscopic clipping devices. Surg Endosc. 2013;27:1521-1529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (36)] |
| 17. | Jensen DM, Machicado GA. Hemoclipping of chronic canine ulcers: a randomized, prospective study of initial deployment success, clip retention rates, and ulcer healing. Gastrointest Endosc. 2009;70:969-975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Hepworth CC, Kadirkamanathan SS, Gong F, Swain CP. A randomised controlled comparison of injection, thermal, and mechanical endoscopic methods of haemostasis on mesenteric vessels. Gut. 1998;42:462-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 19. | Naegel A, Bolz J, Zopf Y, Matthes K, Mueller B, Kraus F, Neurath MF, Maiss J. Hemodynamic efficacy of the over-the-scope clip in an established porcine cadaveric model for spurting bleeding. Gastrointest Endosc. 2012;75:152-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 20. | Kirschniak A, Subotova N, Zieker D, Königsrainer A, Kratt T. The Over-The-Scope Clip (OTSC) for the treatment of gastrointestinal bleeding, perforations, and fistulas. Surg Endosc. 2011;25:2901-2905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 180] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 21. | Manta R, Galloro G, Mangiavillano B, Conigliaro R, Pasquale L, Arezzo A, Masci E, Bassotti G, Frazzoni M. Over-the-scope clip (OTSC) represents an effective endoscopic treatment for acute GI bleeding after failure of conventional techniques. Surg Endosc. 2013;27:3162-3164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 86] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 22. | Chan SM, Chiu PW, Teoh AY, Lau JY. Use of the Over-The-Scope Clip for treatment of refractory upper gastrointestinal bleeding: a case series. Endoscopy. 2014;46:428-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 74] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Yan SL S- Editor: Ji FF L- Editor: A E- Editor: Li D