Published online Jun 10, 2016. doi: 10.4253/wjge.v8.i11.433
Peer-review started: November 7, 2015
First decision: December 10, 2015
Revised: February 10, 2016
Accepted: February 23, 2016
Article in press: February 24, 2016
Published online: June 10, 2016
Processing time: 213 Days and 13.8 Hours
AIM: To compare low volume polyethylene glycol with ascorbic acid, sodium picosulfate-magnesium citrate and clear liquid diet alone as bowel preparation prior to small bowel capsule endoscopy (CE).
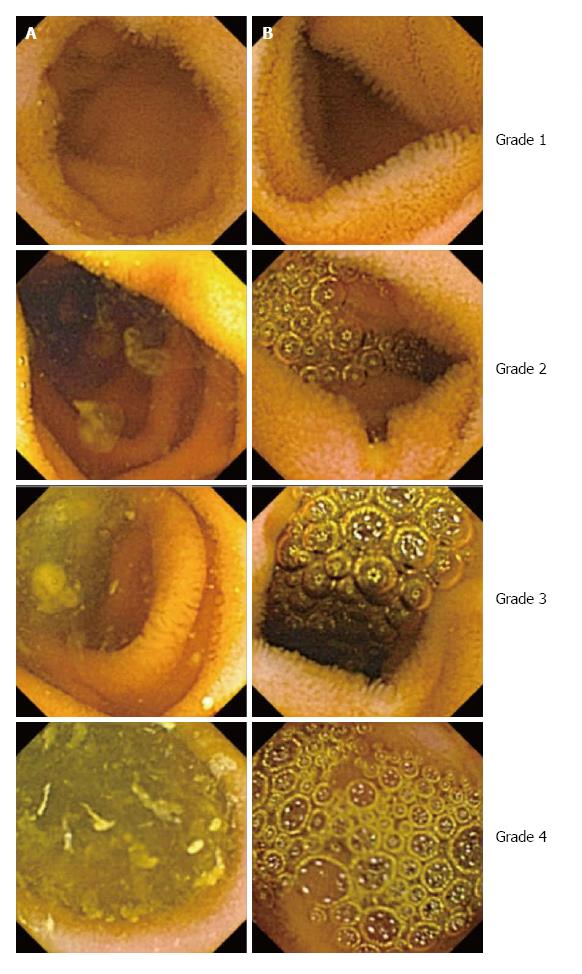
METHODS: We retrospectively collected all CE studies done from December 2011 to July 2013 at a single institution. CE studies were reviewed only if low volume polyethylene glycol with ascorbic acid, sodium picosulfate-magnesium citrate or clear liquid diet alone used as the bowel preparation. The studies were then reviewed by the CE readers who were blinded to the preparation type. Cleanliness and bubble burden were graded independently within the proximal, middle and distal small bowel using a four-point scale according to the percentage of small bowel mucosa free of debris/bubbles: grade 1 = over 90%, grade 2 = between 90%-75%, grade 3 = between 50%-75%, grade 4 = less than 50%. Data are expressed as mean ± SEM. ANOVA and Fishers exact test were used where appropriate. P values < 0.05 were considered statistically significant.
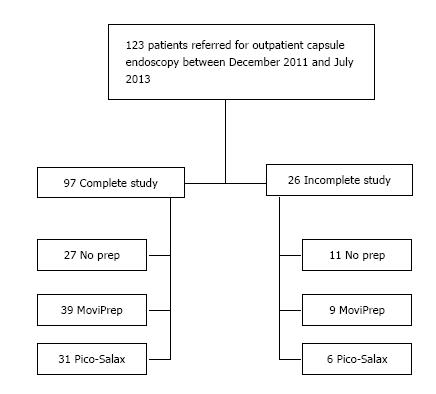
RESULTS: A of total of 123 CE studies were reviewed. Twenty-six studies were excluded from analysis because of incomplete small bowel examination. In the remaining studies, 39 patients took low volume polyethylene glycol with ascorbic acid, 31 took sodium picosulfate-magnesium citrate and 27 took a clear liquid diet alone after lunch on the day before CE, followed by overnight fasting in all groups. There was no significant difference in small bowel cleanliness (1.98 ± 0.09 vs 1.84 ± 0.08 vs 1.76 ± 0.08) or small bowel transit time (213 ± 13 vs 248 ± 14 ± 225 ± 19 min) for clear liquid diet alone, MoviPrep and Pico-Salax respectively. The bubble burden in the mid small bowel was significantly higher in the MoviPrep group (1.6 ± 0.1 vs 1.9 ± 0.1 vs 1.6 ± 0.1, P < 0.05). However this did not result in a significant difference in diagnosis of pathology.
CONCLUSION: There was no significant difference in small bowel cleanliness or diagnostic yield of small bowel CE between the three preparations regimens used in this study.
Core tip: Adequate small bowel preparation is essential for diagnosing small bowel pathology on video capsule endoscopy, but the optimal small bowel preparation method remains unclear. Due the small volume and safety, low volume polyethylene glycol (PEG) based regimens become attractive. However no previous studies have compared low volume PEG with ascorbic acid to sodium picosulfate-magnesium citrate or clear liquid diet alone. In this retrospective study we performed a direct comparison between these three regimens. The bubble burden was significantly higher in the low PEG group but no differences in small bowel cleanliness or diagnostic yield were found between the three regimens.
- Citation: Rayner-Hartley E, Alsahafi M, Cramer P, Chatur N, Donnellan F. Low volume polyethylene glycol with ascorbic acid, sodium picosulfate-magnesium citrate, and clear liquid diet alone prior to small bowel capsule endoscopy. World J Gastrointest Endosc 2016; 8(11): 433-438
- URL: https://www.wjgnet.com/1948-5190/full/v8/i11/433.htm
- DOI: https://dx.doi.org/10.4253/wjge.v8.i11.433
Capsule endoscopy (CE) has revolutionized the management of small bowel diseases including obscure GI bleeding, Crohn’s disease, polyposis syndromes and advanced celiac disease[1-4]. The diagnostic yield (DY) is affected by a number of factors including intraluminal material, bubbles, and both gastric and small bowel transit times[5].
Adequate small bowel preparation is important to increase the DY. Multiple studies have been done comparing various bowel preparation regimens, including just an overnight fast. Despite numerous studies, controversy exists regarding the optimal bowel preparation prior to CE[6-22]. Previous studies have examined the use of laxatives, prokinetics as well as surfactant agents. The bowel preparation regimen may also have an impact on the gastric and small bowel transit times. Recent consensus guidelines recommend polyethylene glycol (PEG) based laxatives as first line agents[23].
The primary aim of this study was to evaluate the DY, small bowel cleanliness, bubble burden and both gastric and small bowel transit times following three different preparation regimens. To our knowledge, no previous studies compared a low volume PEG based agent to a sodium picosulfate - magnesium citrate based agent and clear liquid diet alone.
The charts for all patients referred for outpatient CE between December 2011 and July 2013 were reviewed. Patients were included only if they were given one of the following three bowel preparation regimens: Low volume PEG based agent (MoviPrep, Norgine), sodium picosulfate and magnesium citrate based agent (Pico-Salax, Ferring) and a clear liquid diet alone. In this study, the patients in the groups of MoviPrep and Pico-Salax were instructed to take the first sachet at 14h00 and the second at 17h00. All patients ingested the capsule at approximately 8 am of the study day. All CE examinations were performed using the Olympus Endocapsule.
Two experienced reviewers who were blinded to preparation method (FD and NC) reviewed all CE studies for diagnostic evaluation, and both gastric and small bowel transit time. Clinical disagreement was solved by joint review and discussion. One CE reader who was blinded to preparation (ERH) reviewed all CE studies for mucosal visibility grading related to cleanliness and bubble burden. Once the CE studies have been reviewed, patients were assigned into one of the three different groups based on the bowel preparation regimen given according to chart review.
Only CE studies with complete small bowel examinations, determined by identification of the cecum were included for analysis. The primary outcome measures included the DY, intraluminal small bowel cleanliness and bubble burden. Small bowel cleanliness and bubble burden were graded independently within the proximal, mid and distal small bowel using a four-point scale according to the percentage of small bowel mucosa free of debris/bubbles: Grade 1 = over 90%, grade 2 = between 90%-75%, grade 3 = between 50%-75%, grade 4 = less than 50% (Figure 1). This grading system was developed by the authors based on the commonly used grading criteria as there is no validated scoring system available. The anatomic divisions were determined by dividing the small bowel into three segments based on the small bowel transit time.
According to CE protocol in our center, patients are instructed to follow a clear liquid diet after lunch the day prior to CE, followed by an overnight fast as of 21h00. They are permitted to resume a clear fluid diet 2 h after recording begin and a light meal 4 h later. Patients return 8 h after ingestion of the capsule to disconnect the recorder. An abdominal X-ray is obtained at one week following ingestion to determine if the capsule is retained if it did not reach the cecum or the patient did not report its passage.
Data are expressed as mean ± SEM. ANOVA and Fishers exact test were used where appropriate. P value < 0.05 were considered statistically significant. Statistical analysis was performed by Fergal Donnellan (University of British Columbia).
One hundred and twenty-three patients were included, 48 patients took MoviPrep, 37 took Pico-Salax and 38 took a clear liquid diet alone. Table 1 depicts the patients’ characteristics. There was no statistically significant different between the three groups in regard to gender, age or complete small bowel examination. Ninty-seven (78.9%) patients had a complete small bowel examination and thus included in the final analysis. This included 39 (81%) patients in the MoviPrep group, 31 (84%) patients in the Pico-Salax group and 27 (71%) patients in the clear liquid group (Figure 2).
| Variable | No prep n = 38 | MoviPrep n = 48 | Pico-Salax n = 37 |
| Male | 11 (28.9) | 22 (45.8) | 18 (48.6) |
| Mean age (yr) | 52.7 | 54.1 | 53.2 |
| Indication | |||
| Obscure bleeding | 17 (44.7) | 27 (56.3) | 19 (51.4) |
| Abnormal imaging | 3 (7.9) | 4 (8.3) | 5 (15.3) |
| Suspected IBD | 11 (28.9) | 11 (22.9) | 10 (27) |
| Other | 7 (18.4) | 6 (12.5) | 3 (8.1) |
| Completion rate | 27 (71) | 39 (81.3) | 31 (83.8) |
Table 2 depicts the results for small bowel cleanliness, bubble burden and both gastric and small bowel transit times. There was a significant increase in the bubble burden in the mid small bowel in the MoviPrep group (P < 0.05). Otherwise there was no difference between the three groups in terms of cleanliness or bubble burden. Similarly there was no difference in the small bowel transit time. The gastric transit time, however, was significantly longer in the Pico-Salax group only (P < 0.05).
| Result | No prep n = 27 | MoviPrep n = 39 | Pico-Salax n = 31 | P value |
| Cleanliness | ||||
| Proximal | 1.4 ± 0.1 | 1.7 ± 0.1 | 1.6 ± 0.1 | 0.1 |
| Mid | 1.8 ± 0.2 | 1.8 ± 0.2 | 2.0 ± 0.2 | 0.7 |
| Distal | 2.1 ± 0.2 | 2.4 ± 0.2 | 2.3 ± 0.2 | 0.6 |
| Bubble burden | ||||
| Proximal | 1.5 ± 0.1 | 1.8 ± 0.1 | 1.7 ± 0.1 | 0.1 |
| Mid | 1.6 ± 0.1 | 1.9 ± 0.1 | 1.6 ± 0.1 | < 0.05 |
| Distal | 1.6 ± 0.1 | 1.8 ± 0.2 | 1.5 ± 0.1 | 0.09 |
| Gastric transit time (min) | 26 ± 5 | 25 ± 6 | 47 ± 9 | < 0.05 |
| Small bowel transit time (min) | 213 ± 13 | 248 ± 14 | 225 ± 19 | 0.3 |
Table 3 depicts the results for DY and abnormal findings. Overall there was no difference in detection of pathology between the three groups (P = 0.6). However, there was a trend towards increased detection of vascular lesions in the MoviPrep group and ulceration in the clear liquid diet group, however these findings were not statistically significant (P = 0.06 and 0.07 respectively).
| Finding | No prepn = 27 | MoviPrepn = 39 | Pico-Salaxn = 31 |
| Abnormal study | 13 (48.1) | 19 (48.7) | 13 (41.9) |
| Gastric | 2 (7.4) | 1 (2.6) | 0 (0.0) |
| Small bowel | |||
| Vascular | 1 (3.7) | 10 (25.6) | 5 (16.1) |
| Ulcer/erosion | 7 (25.9) | 3 (7.7) | 3 (9.7) |
| Polyp/mass | 0 (0.0) | 1 (2.6) | 3 (9.7) |
| Blood | 0 (0.0) | 1 (2.6) | 1 (3.2) |
| Abnormal mucosa | 2 (7.4) | 3 (7.7) | 1 (3.2) |
| other | 1 (3.7) | 0 (0.0) | 0 (0.0) |
Since its introduction in 2000, CE is now recognized as a widely applicable, non-invasive tool with a high DY[24]. Unlike conventional endoscopy, which has the advantage of washing and suctioning to improve mucosal visibility, CE relies on the state of the small bowel at time of exam. No universally accepted bowel preparation regimen exists amongst clinicians[6-22].
The most studied agents in small bowel CE preparation are PEG, sodium phosphate and sodium picosulphate. Recent meta-analyses found that the DY and small bowel visualization quality were superior with PEG or sodium phosphate in comparison to clear fluid diet[5,6]. None of these studies included sodium picosulphate. Lower volume PEG (2L) has been shown as effective as 4L, which is preferable for patient tolerance[7,8]. Magnesium citrate is another agent that is less well studied. One retrospective analysis showed significant improvement in clarification of intestinal juices with magnesium citrate as compared to simethicone[10]. Subsequent studies however, have not reported significant differences in cleansing efficacy[9-11].
In our study, we did not find a significant difference in cleanliness, bubble burden or transit time in the three groups studied. Only the bubble burden in the mid small bowel in the MoviPrep group and the gastric transit time in the Pico-Salax group were significantly different. When considering that no difference in pathology detection was noted between the groups, our results concur with previously published studies that CE DY may be preserved with the simplicity of a clear liquid diet. The small bowel is primarily a site of nutrient absorption and not stool formation. Thus, unlike colonoscopy preparation, it is logical that a preparation method without purgative agents could be adequate. We did note a non-significant trend towards increased detection of vascular lesions only in the MoviPrep group and ulceration in the clear liquid diet alone group. It is difficult to conclude that this is due to the regimen, but more likely due to small sample size.
Recent consensus guidelines along with European Society of Gastrointestinal Endoscopy recommendations support the use of PEG based purgative agents prior to CE[23,25,26]. Our findings suggest that a clear liquid diet the day prior to CE followed by an overnight fast is as effective for detection of pathology on CE. We included preparation agents that have not been previously directly compared.
Our study has several limitations. This was a retrospective study with a relatively small sample size. However we reviewed all the CE examinations blindly for the purpose of this study. The compliance with bowel preparation used could not be verified given the retrospective design. The anatomical sections of the small bowel were arbitrarily determined by dividing the total small bowel transit time into three periods, while the CE speed might be variable.
In conclusion, our study demonstrates no clinically significant difference in small bowel cleanliness or DY between three preparations regimens used in this study. Only the bubble burden in the mid small bowel in the MoviPrep group and the gastric transit time in the Pico-Salax group were significantly different. Our study suggests that it is reasonable to consider eliminating the use of bowel preparation prior to outpatient CE.
Capsule endoscopy (CE) has revolutionized the management of small bowel diseases including obscure GI bleeding, Crohn’s disease, polyposis syndromes and advanced celiac disease. Adequate small bowel preparation is required to increase the diagnostic yield (DY). The DY is affected by a number of factors including intraluminal material, bubbles, and both gastric and small bowel transit times. Multiple studies have been done comparing various bowel preparation regimens, including just an overnight fast. Previous studies have also examined the use of laxatives, prokinetics as well as surfactant agents. Despite numerous studies, controversy exists regarding the optimal bowel preparation prior to CE.
To the authors’ knowledge, no previous studies compared a low volume polyethylene glycol (PEG) based agent to a sodium picosulfate and magnesium citrate based agent and clear liquid diet alone.
In this study, the authors compared low volume PEG with ascorbic acid (MoviPrep), sodium picosulfate-magnesium citrate (Pico-Salax) and clear liquid diet alone as bowel preparation prior to small bowel CE. Only the bubble burden in the mid small bowel in the MoviPrep group and the gastric transit time in the Pico-Salax group were significantly different. However the authors did not find a significant difference in the small bowel cleanliness or the DY.
When considering that no difference in the DY was noted between the three groups, the results concur with previously published studies that CE DY may be preserved with the simplicity of a clear liquid diet alone.
Small bowel CE: A pill sized video camera ingested by the patient which allows examination of small bowel.
This is a retrospective study which compared low volume polyethylene glycol with ascorbic acid, sodium picosulfate-magnesium citrate and clear liquid diet alone as bowel preparation prior to small bowel CE.
| 1. | Fisher L, Lee Krinsky M, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T, Cash BD, Decker GA, Fanelli RD, Friis C. The role of endoscopy in the management of obscure GI bleeding. Gastrointest Endosc. 2010;72:471-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 167] [Article Influence: 10.4] [Reference Citation Analysis (1)] |
| 2. | Dionisio PM, Gurudu SR, Leighton JA, Leontiadis GI, Fleischer DE, Hara AK, Heigh RI, Shiff AD, Sharma VK. Capsule endoscopy has a significantly higher diagnostic yield in patients with suspected and established small-bowel Crohn’s disease: a meta-analysis. Am J Gastroenterol. 2010;105:1240-1248; quiz 1249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 287] [Article Influence: 17.9] [Reference Citation Analysis (36)] |
| 3. | Mata A, Llach J, Castells A, Rovira JM, Pellisé M, Ginès A, Fernández-Esparrach G, Andreu M, Bordas JM, Piqué JM. A prospective trial comparing wireless capsule endoscopy and barium contrast series for small-bowel surveillance in hereditary GI polyposis syndromes. Gastrointest Endosc. 2005;61:721-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 99] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 4. | Culliford A, Daly J, Diamond B, Rubin M, Green PH. The value of wireless capsule endoscopy in patients with complicated celiac disease. Gastrointest Endosc. 2005;62:55-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 132] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 5. | Rokkas T, Papaxoinis K, Triantafyllou K, Pistiolas D, Ladas SD. Does purgative preparation influence the diagnostic yield of small bowel video capsule endoscopy?: A meta-analysis. Am J Gastroenterol. 2009;104:219-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 130] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 6. | Belsey J, Crosta C, Epstein O, Fischbach W, Layer P, Parente F, Halphen M. Meta-analysis: efficacy of small bowel preparation for small bowel video capsule endoscopy. Curr Med Res Opin. 2012;28:1883-1890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | Park SC, Keum B, Seo YS, Kim YS, Jeen YT, Chun HJ, Um SH, Kim CD, Ryu HS. Effect of bowel preparation with polyethylene glycol on quality of capsule endoscopy. Dig Dis Sci. 2011;56:1769-1775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Hartmann D, Keuchel M, Philipper M, Gralnek IM, Jakobs R, Hagenmüller F, Neuhaus H, Riemann JF. A pilot study evaluating a new low-volume colon cleansing procedure for capsule colonoscopy. Endoscopy. 2012;44:482-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | Ninomiya K, Yao K, Matsui T, Sato Y, Kishi M, Karashima Y, Ishihara H, Hirai F. Effectiveness of magnesium citrate as preparation for capsule endoscopy: a randomized, prospective, open-label, inter-group trial. Digestion. 2012;86:27-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Esaki M, Matsumoto T, Kudo T, Yanaru-Fujisawa R, Nakamura S, Iida M. Bowel preparations for capsule endoscopy: a comparison between simethicone and magnesium citrate. Gastrointest Endosc. 2009;69:94-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 34] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Postgate A, Tekkis P, Patterson N, Fitzpatrick A, Bassett P, Fraser C. Are bowel purgatives and prokinetics useful for small-bowel capsule endoscopy? A prospective randomized controlled study. Gastrointest Endosc. 2009;69:1120-1128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 64] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 12. | Wei W, Ge ZZ, Lu H, Gao YJ, Hu YB, Xiao SD. Effect of mosapride on gastrointestinal transit time and diagnostic yield of capsule endoscopy. J Gastroenterol Hepatol. 2007;22:1605-1608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 51] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 13. | Ida Y, Hosoe N, Imaeda H, Bessho R, Ichikawa R, Naganuma M, Kanai T, Hibi T, Ogata H. Effects of the oral administration of mosapride citrate on capsule endoscopy completion rate. Gut Liver. 2012;6:339-343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Leung WK, Chan FK, Fung SS, Wong MY, Sung JJ. Effect of oral erythromycin on gastric and small bowel transit time of capsule endoscopy. World J Gastroenterol. 2005;11:4865-4868. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 56] [Cited by in RCA: 64] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Caddy GR, Moran L, Chong AK, Miller AM, Taylor AC, Desmond PV. The effect of erythromycin on video capsule endoscopy intestinal-transit time. Gastrointest Endosc. 2006;63:262-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 65] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Niv E, Bonger I, Barkay O, Halpern Z, Mahajna E, Depsames R, Kopelman Y, Fireman Z. Effect of erythromycin on image quality and transit time of capsule endoscopy: a two-center study. World J Gastroenterol. 2008;14:2561-2565. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 32] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Selby W. Complete small-bowel transit in patients undergoing capsule endoscopy: determining factors and improvement with metoclopramide. Gastrointest Endosc. 2005;61:80-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 101] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 18. | Koulaouzidis A, Giannakou A, Yung DE, Dabos KJ, Plevris JN. Do prokinetics influence the completion rate in small-bowel capsule endoscopy? A systematic review and meta-analysis. Curr Med Res Opin. 2013;29:1171-1185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 19. | Shiotani A, Opekun AR, Graham DY. Visualization of the small intestine using capsule endoscopy in healthy subjects. Dig Dis Sci. 2007;52:1019-1025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Wei W, Ge ZZ, Lu H, Gao YJ, Hu YB, Xiao SD. Purgative bowel cleansing combined with simethicone improves capsule endoscopy imaging. Am J Gastroenterol. 2008;103:77-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 73] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 21. | Spada C, Riccioni ME, Familiari P, Spera G, Pirozzi GA, Marchese M, Bizzotto A, Ingrosso M, Costamagna G. Polyethylene glycol plus simethicone in small-bowel preparation for capsule endoscopy. Dig Liver Dis. 2010;42:365-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Wu L, Cao Y, Liao C, Huang J, Gao F. Systematic review and meta-analysis of randomized controlled trials of Simethicone for gastrointestinal endoscopic visibility. Scand J Gastroenterol. 2011;46:227-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 98] [Article Influence: 6.5] [Reference Citation Analysis (4)] |
| 23. | Mathus-Vliegen E, Pellisé M, Heresbach D, Fischbach W, Dixon T, Belsey J, Parente F, Rio-Tinto R, Brown A, Toth E. Consensus guidelines for the use of bowel preparation prior to colonic diagnostic procedures: colonoscopy and small bowel video capsule endoscopy. Curr Med Res Opin. 2013;29:931-945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 24. | Iddan G, Meron G, Glukhovsky A, Swain P. Wireless capsule endoscopy. Nature. 2000;405:417. [PubMed] |
| 25. | Song HJ, Moon JS, Do JH, Cha IH, Yang CH, Choi MG, Jeen YT, Kim HJ. Guidelines for Bowel Preparation before Video Capsule Endoscopy. Clin Endosc. 2013;46:147-154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 42] [Article Influence: 3.2] [Reference Citation Analysis (1)] |
| 26. | Ladas SD, Triantafyllou K, Spada C, Riccioni ME, Rey JF, Niv Y, Delvaux M, de Franchis R, Costamagna G. European Society of Gastrointestinal Endoscopy (ESGE): recommendations (2009) on clinical use of video capsule endoscopy to investigate small-bowel, esophageal and colonic diseases. Endoscopy. 2010;42:220-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 173] [Article Influence: 10.8] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Chen JQ, Mentes O S- Editor: Qi Y L- Editor: A E- Editor: Lu YJ