Published online Jul 25, 2015. doi: 10.4253/wjge.v7.i9.889
Peer-review started: November 23, 2014
First decision: December 12, 2014
Revised: May 2, 2015
Accepted: June 18, 2015
Article in press: June 19, 2015
Published online: July 25, 2015
Processing time: 255 Days and 22.1 Hours
AIM: To evaluate the efficacy and safety of single-step endoscopic placement of self-expandable metallic stents (SEMS) for treatment of obstructive jaundice.
METHODS: A retrospective study was performed among 90 patients who underwent transpapillary biliary metallic stent placement for malignant biliary obstruction (MBO) between April 2005 and October 2012. The diagnosis of primary disease and MBO was based on abdominal ultrasound, computed tomography, magnetic resonance imaging, endoscopic ultrasound, endoscopic retrograde cholangiopancreatography with brush cytology, biopsy, and/or a combination of these modalities. The type of SEMS (covered or non-covered, 8 mm or 10 mm in diameter) was determined by the endoscopist. Ninety patients were divided into two groups: group 1 (49 patients) who underwent a single-step SEMS placement and group 2 (41 patients) who underwent a two-step SEMS placement. The technical success rate, complication rate, stent patency, and patient survival rate were compared between the groups. In addition, to identify the clinical prognostic factors associated with patient survival, the following variables were evaluated in Cox-regression analysis: gender, age, etiology of MBO (pancreatic cancer or non-pancreatic cancer), clinical stage (IVb; with distant metastases or IVa >; without distant metastases), chemotherapy (with or without), patency of the stent, and the use of single-step or two-step SEMS.
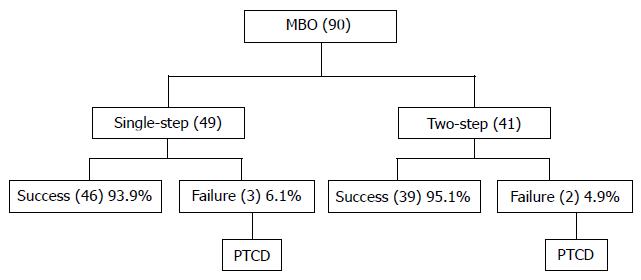
RESULTS: Immediate technical success was achieved in 93.9% (46/49) in group 1 and in 95.1% (39/41) in group 2, with no significant difference (P = 1.0). Similarly, there was no difference in the complication rates between the groups (group 1, 4.1% and group 2, 4.9%; P = 0.62). Stent failure was observed in 10 cases in group 1 (20.4%) and in 16 cases in group 2 (39.0%). The patency of stent and patient survival revealed no difference between the two groups with Kaplan-Meier analysis, with a mean patency of 111 ± 17 d in group 1 and 137 ± 19 d in group 2 (P = 0.91), and a mean survival of 178 ± 35 d in group 1 and 222 ± 23 d in group 2 (P = 0.57). On the contrary, the number of days of hospitalization associated with first-time SEMS placement in group 1 was shorter when compared with that number in group 2 (28 vs 39 d; P < 0.05). Multivariate analysis revealed that a clinical stage of IVa > (P = 0.0055), chemotherapy (P = 0.0048), and no patency of the stent (P = 0.011) were independent prognostic factors associated with patient survival.
CONCLUSION: Our results showed that single-step endoscopic metal stent placement was safe and effective for treating obstructive jaundice secondary to various inoperable malignancies.
Core tip: Single-step placement of expandable metallic stents for treating malignant biliary obstruction is useful for shortening hospitalization. To maximize symptomatic relief and cost benefits, stent placement should not be delayed after deciding on metal stent palliation.
- Citation: Yamamoto R, Takahashi M, Osafune Y, Chinen K, Kato S, Nagoshi S, Yakabi K. Comparison of endoscopic stenting for malignant biliary obstruction: A single-center study. World J Gastrointest Endosc 2015; 7(9): 889-894
- URL: https://www.wjgnet.com/1948-5190/full/v7/i9/889.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i9.889
Because of improvements in operative procedures and diagnostic techniques, both the incidence of biliary pancreatic malignancies and resection rates have increased. Nevertheless, partly due to the high incidence obstructive jaundice in affected patients, some cases remain inoperable with a poor prognosis. Presently, the preferred treatment for jaundice due to malignant biliary pancreatic obstruction is biliary stent placement. Such stenting was initially performed using polyethylene plastic stents; however, expanding metal stents have been available for several years[1,2]. These expandable metallic stents have several advantages over plastic stents: (1) they can be introduced by a smaller delivery catheter; (2) they have a large inner diameter; and (3) they can remain fixed in position after release[3-6]. In this study, we assessed the safety and efficacy of single-step endoscopic placement for self-expandable metallic stents (SEMS) for treating obstructive jaundice secondary to various inoperable malignancies.
This study included 90 patients who underwent transpapillary biliary metallic stent placement for malignant biliary obstruction (MBO) between April 2005 and October 2012 at the Saitama Medical Center of Saitama Medical University. For these 90 patients (72 men and 18 women), the diagnoses of primary disease and MBO were based on abdominal ultrasound, computed tomography, magnetic resonance imaging, endoscopic ultrasound, endoscopic retrograde cholangiopancreatography with brush cytology, biopsy, and/or a combination of these modalities. Before cholangiography, all patients were diagnosed with obstructive jaundice caused by an unresectable malignancy because of either very advanced carcinoma or old age. The type of SEMS (covered or noncovered, 8 mm or 10 mm in diameter) was determined by the endoscopist. Ninety patients were divided into two groups: group 1 (49 patients) who underwent a single-step SEMS placement and group 2 (41 patients) who underwent a two-step SEMS placement, depending on the severity of cholangitis. The flowchart for the single-step and two-step SEMS placements for distal MBO is shown in Figure 1.
The technical success rate, complication rate, length of hospital stay, stent patency, and patient survival rate were compared between the groups. Techinical success was defined as successful endoscopic deployment of the stent at the appropriate position resulting in a smooth drainage of the stented bile ducts. Complication rate was defined as the pancreatitis, bleeding and cholangitis arising from stent placement for malignant bile duct obstruction. And, length of hospital stay was defined as the period between hospital admission and discharge. In addition, to identify the clinical prognostic factors associated with patient survival, the following variables were evaluated with a Cox-regression analysis: gender, age, etiology of MBO (pancreatic cancer or nonpancreatic cancer), clinical stage (IVb with distant metastasis or IVa > without distant metastasis), chemotherapy (with or without), patency of the stent, and the use of single-step SEMS or two-step SEMS. This study was performed according to the principles of the Declaration of Helsinki, and informed consent was obtained from the patients and/or their families.
We reviewed medical records and radiological images of all patients undergoing stent placement. We then assessed the following variables using univariate analyses (χ2 test or Fisher’s exact test) to identify patient survival: sex, age, etiology of MBO (pancreatic cancer or nonpancreatic cancer), clinical stage (IVb with distant metastasis or > IVa without distant metastasis), chemotherapy (with or without), stent patency, and the use of single-step SEMS or two-step SEMS. We estimated survival times with the Kaplan–Meier method and compared them using the log-rank test. We also calculated odds ratios with 95%CIs for all variables. These statistical tests were two-sided, and statistical significance was set at P value < 0.05 for all analyses. The statistical evaluation was performed using SPSS (IBM, JAPAN) 21.0 for Windows.
The clinical characteristics of the study participants are summarized in Table 1. The single-step group (group 1) included only 49 men (percentage of men = 100%) with a mean age of 70.1 years. The two-step group (group 2) included 23 men (56.1%, P < 0.01) and 18 women (43.9%) with a mean age of 74.3 years. The incidence of pancreatic cancer was higher in group 1 than in group 2 (59.2% vs 31.7%, P = 0.016) (Table 1). The information concerning stricture location and endoscopic sphincterotomy (EST) performance before stenting is shown in Table 1. The number of ESTs performed before stenting was statistically significantly higher in group 1 than in group 2 (2.0% vs 22%, P < 0.01). The patient characteristics in the two groups categorized by treatment are summarized in Table 1. Although hilar obstruction was significantly less frequent in group 1 than in group 2 (22.4% vs 46.3%, P = 0.03), there was no difference in bilateral drainage rate between the two groups (group 1, 4.1% and group 2, 12.2%; P = 0.24). Immediate technical success was achieved in 93.9% (46/49) patients in group 1 and 95.1% (39/41) patients in group 2; there was no significant difference (P = 1.0). Serum total bilirubin levels were within normal limits within two weeks after placement of the stent in all patients who underwent successful procedures. Likewise, there was no difference in the occurrence of complication between the groups (group 1, 4.1% and group 2, 4.9%; P = 0.62).
| Variable | Single-step (n = 49) | Two-step (n = 41) | P |
| Mean age (yr) | 70.1 ± 12.6 | 74.3 ± 9.9 | NS |
| Gender (n) | |||
| Male | 49 | 23 | < 0.01 |
| Female | 0 | 18 | |
| Etiology of MBO: | |||
| pancratic cancer (%) | 59.2 | 31.7 | 0.016 |
| MPD tumor involvement present (%) | 36.7 | 24.4 | NS |
| Spincterotomy (%) | 2.0 | 22.0 | 0.003 |
| Hilar biliary obstruction (%) | 22.4 | 46.3 | 0.03 |
| Clinical stage | |||
| IVa > (%) | 40.8 | 61 | NS |
| IVb (%) | 59.2 | 39 | NS |
| Bilateral drainage (%) | 4.1 | 12.2 | NS |
| Technical success rate (%) | 93.9 | 95.1 | NS |
| Complication rate (%) | 4.1 | 4.8 | NS |
| Chemotherapy (%) | 55.1 | 51.2 | NS |
| Length of hospital stay (d) | 28.1 ± 28.6 | 39.6 ± 25.7 | < 0.05 |
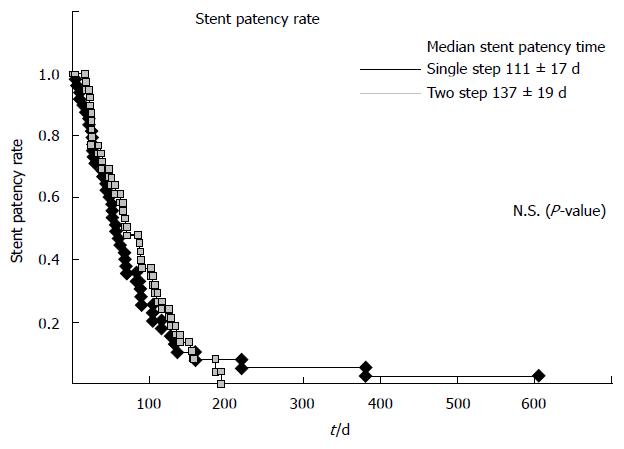
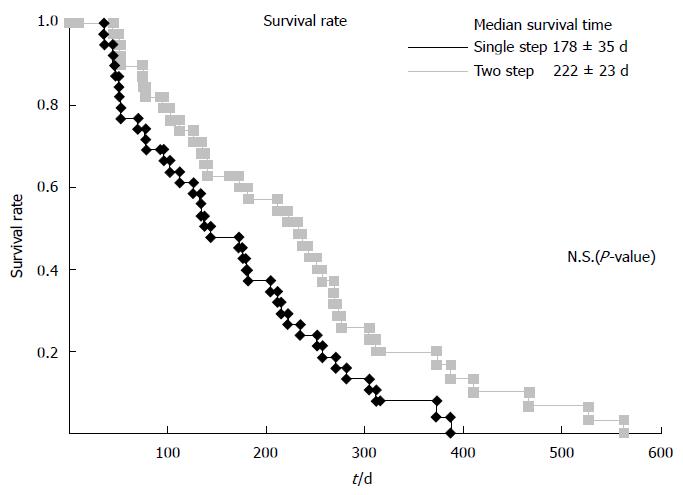
We observed stent failure in 10 cases in group 1 (20.4%) and 16 cases in group 2 (39.0%). The stent was patent in all 26 cases. There was no difference in the stent patency or patient survival between both groups using the Kaplan–Meier analysis, with a mean patency of 111 ± 17 d in group 1 and 137 ± 19 d in group 2 (P = 0.91, Figure 2), and a mean survival of 178 ± 35 d in group 1 and 222 ± 23 d in group 2 (P = 0.57, Figure 3). In contrast, the number of hospitalization days associated with first-time SEMS placement in group 1 was shorter than in group 2 (28 vs 39 d; P < 0.05). Multivariate analysis found that a clinical stage of IVa > (P = 0.0055), chemotherapy (P = 0.0048), and no patency of the stent (P = 0.011) were independently associated prognostic factors for patient survival (Table 2).
| Variables | OR | 95%CI | P |
| Step (single vs two) | 0.81 | 0.49-1.36 | 0.42 |
| Gender (male vs female) | 1.05 | 0.66-1.67 | 0.83 |
| Age (69 ≥vs 70 < ) | 1.02 | 0.59-1.76 | 0.96 |
| Pancratic cancer (yes vs no) | 1.01 | 0.21-1.61 | 0.98 |
| Clinical stage (IVa ≥vs IVb) | 2.03 | 1.23-3.34 | 0.006 |
| Chemotherapy (with vs without) | 2.18 | 1.27-3.76 | 0.005 |
| Patency of the stent (no vs yes) | 2.21 | 1.20-4.07 | 0.011 |
Patients with malignant bile duct obstruction have poor long-term survival and are not candidates for surgical resection. The goals of palliation using a biliary stent placement are symptomatic relief of obstructive jaundice, prevention of cholangitis, and prolongation of survival. Stenting has also been found to improve quality of life of these patients. To maximize the symptomatic relief and cost benefits, the stent should be placed as soon as the decision for metal stent palliation has been made. However, a recent study[7,8] that compared the single-step and two-step procedures found that procedure-related complication rate improved with single-step procedures with no increase in early complications. However, Hamada et al[8] reported that single-step SEMS placement for distal MBO was associated with a shorter time to dysfunction and a higher rate of stent migration than two-step SEMS placement. In addition, single-step procedure caused minimal patient discomfort, and avoided both the second intervention and drainage catheter dislocation risk before the deployment of the stent. The single-step placement procedure has two goals: (1) reducing the number of interventions and hence the procedural expenses; and (2) eliminating the need for bile-collecting bags or bottles, thus resulting in an improvement in quality of life as well as reduction in hospitalizations.
In this study, we evaluated the efficacy and safety of the single-step endoscopic placement of SEMS for treating obstructive jaundice that can be caused by various inoperable malignancies. There was no difference in stent patency and patient survival between the two groups in the Kaplan–Meier analysis. In contrast, the number of hospitalization days associated with first-time SEMS placement in group 1 was lower than in group 2 (28 vs 39 d, P < 0.05). The multivariate analysis revealed that a clinical stage of IVa > (P = 0.0055), chemotherapy (P = 0.0048), and no patency of the stent (P = 0.011) were independently associated prognostic factors of patient survival. Patients with inoperable malignant strictures generally receive only palliative radiotherapy or chemotherapy and have a limited life expectancy. One possible reason for poor outcomes may be the delay between the diagnostic cholangiography and the placement of the metallic stent[9]. McDougall et al[9] determined that 25 (78%) patients had a plastic stent placed before placement of the metallic stent, leading to a mean delay of 123 d, and that 7 (22%) patients had > 1 metallic stent placed. This clearly suggests that if a metallic stent is placed earlier in the course of the disease, the stent patency can be prolonged.
The strategies for self-expandable metal stent placement can depend on the primary cancer types because of the differences in their biological behavior. However, the survival times were not significantly different between patients with pancreatic cancer and those with other primary cancers in our study population. Therefore, this factor may not have any effects on the results of the analyses.
The limitations of our study were as follows. Firstly, our study population was not large enough for a meaningful analysis regarding the efficacy of single-step endoscopic metal stent placement. Secondly, because this was not a prospective study, selection biases regarding the type of SEMS and the procedure adopted for cannulation of the ampulla were present. We propose the implementation of initial stenting for partial drainage of malignant hilar bile duct strictures, rendering contralateral drainage as a last resort for cases with severe cholangitis or insufficient reduction of jaundice.
To conclude, single-step placement of expandable metallic stents for MBO cases that are inoperable is a useful method to shorten hospitalization. Once the decision about metal stent palliation has been made, the stent should be placed as soon as possible to maximize symptomatic relief and cost benefits.
In conclusion, our results showed that single-step endoscopic metal stent placement was safe and effective for treating obstructive jaundice secondary to various inoperable malignancies.
We gratefully acknowledge the assistance of Dr. Ko Nishikawa, Ageo Central General Hospital.
Although self-expandable metal stent (SEMS) placement has been widely performed for treating malignant biliary obstruction (MBO), few studies have compared single-step SEMS (direct placement without a prior plastic stent) and two-step SEMS (stent placement at second session following temporary plastic stent placement).
The objective of this study was the evaluation of the safety and efficacy of single-step endoscopic placement of SEMS for treating obstructive jaundice caused by various inoperable malignancies.
This was a retrospective single-center study of 90 consecutive patients who had undergone endoscopic retrograde cholangiopancreatography-guided transpapillary biliary metallic stent placement for MBO during a 7.5-year-period. The patients of this study were divided into two groups: a single-step SEMS placement group (n = 49) and a two-step SEMS placement group (n = 41). MBO etiologies were similar between both groups, with pancreatic cancer accounting for 46.7% cases. No significant differences in the patency rate of stents and patient survival were observed between the single-and two-step groups. In contrast, the number of hospitalization days associated with first-time SEMS placement in the single-step group was lower compared with that in the other group (28 vs 39 d). Multivariate analysis identified that IVa > clinical stage (P = 0.0055), chemotherapy (P = 0.0048), and no patency of the stent (P = 0.011) were independently associated prognostic factors for patient survival.
These findings will be particularly interesting to the readership of World Journal of Gastrointestinal Endoscopy as they demonstrate that single-step endoscopic metal stent placement is effective and safe for treating obstructive jaundice caused by various inoperable malignancies.
This is a manuscript about an interesting issue that has not been published extensively. It is written in fluent, simple English, easy to comprehend.
| 1. | Huibregtse K, Cheng J, Coene PP, Fockens P, Tytgat GN. Endoscopic placement of expandable metal stents for biliary strictures--a preliminary report on experience with 33 patients. Endoscopy. 1989;21:280-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 107] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Neuhaus H, Hagenmüller F, Griebel M, Classen M. Percutaneous cholangioscopic or transpapillary insertion of self-expanding biliary metal stents. Gastrointest Endosc. 1991;37:31-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 56] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Knyrim K, Wagner HJ, Pausch J, Vakil N. A prospective, randomized, controlled trial of metal stents for malignant obstruction of the common bile duct. Endoscopy. 1993;25:207-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 382] [Cited by in RCA: 360] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 4. | Lee MJ, Dawson SL, Mueller PR, Krebs TL, Saini S, Hahn PF. Palliation of malignant bile duct obstruction with metallic biliary endoprostheses: technique, results, and complications. J Vasc Interv Radiol. 1992;3:665-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 42] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Rossi P, Bezzi M, Rossi M, Adam A, Chetty N, Roddie ME, Iacari V, Cwikiel W, Zollikofer CL, Antonucci F. Metallic stents in malignant biliary obstruction: results of a multicenter European study of 240 patients. J Vasc Interv Radiol. 1994;5:279-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 128] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Stoker J, Laméris JS. Complications of percutaneously inserted biliary Wallstents. J Vasc Interv Radiol. 1993;4:767-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 65] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Akamatsu N, Sugawara Y, Shin N, Komagome M, Ishida T, Ozawa F, Odaka A, Hashimoto D. One-step percutaneous transhepatic insertion of a balloon-expanding metallic stent for obstructive jaundice. J Gastroenterol Hepatol. 2011;26:1795-1803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Hamada T, Nakai Y, Isayama H, Togawa O, Kogure H, Kawakubo K, Tsujino T, Sasahira N, Hirano K, Yamamoto N. One- and two-step self-expandable metal stent placement for distal malignant biliary obstruction: a propensity analysis. J Gastroenterol. 2012;47:1248-1256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | McDougall NI, Edmunds SE. An audit of metal stent palliation for malignant biliary obstruction. J Gastroenterol Hepatol. 2001;16:1051-1054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected byan in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Giannopoulos GA, Kayaalp C, Tsuyuguchi T, Ye J S- Editor: Gong XM L- Editor: A E- Editor: Jiao XK