Published online Jul 10, 2015. doi: 10.4253/wjge.v7.i8.824
Peer-review started: September 1, 2014
First decision: December 17, 2014
Revised: January 12, 2015
Accepted: May 5, 2015
Article in press: May 8, 2015
Published online: July 10, 2015
Processing time: 316 Days and 10.9 Hours
AIM: To examine the discrepancy, if any, between the endoscopist’s estimate and pathologist’s measurement of colonic polyp size.
METHODS: We retrospectively studied 88 patients who underwent colonoscopy with a clear unequivocal documentation of polyp size by both endoscopist and pathologist. Endoscopist measurements were based on the visual estimate of polyp size seen on high definition screens. The measurement was done by our pathologists after formalin fixation. We compared the endoscopist estimate of the polyp size to the pathologist measurement in order to explore the discordance between the two readings. Data regarding demographics and method of polypectomy (snare polypectomy vs excisional biopsy) was collected, as well. Statistical analysis software (SAS) was used to analyze the data.
RESULTS: Our cohort included 88 patients from which 111 polyps were removed. Fifty-two (46.8%) of the 111 polyps were excised using biopsy forceps and fifty-nine (53.2%) were removed by snare. In the biopsy forceps group, the mean polyp size documented by the pathologist was 0.38 ± 0.19 cm and the mean polyp size documented by the endoscopist was 0.54 ± 0.16 cm. The mean difference was 0.16 cm (P < 0.001). In the snare group, the mean polyp size documented by the pathologist was 0.54 ± 0.24 cm and the mean polyp size documented by the endoscopist 0.97 ± 0.34 cm. The mean difference was 0.43 cm (P < 0.001). Combining both groups, the mean size documented by pathologist was 0.46 ± 0.23 cm compared to 0.76 ± 0.35 cm documented by the endoscopist. The mean difference was 0.3 cm (95%CI: 0.23-0.36).
CONCLUSION: Post polypectomy measurement by the pathologist are generally smaller than the endoscopist’s estimate.
Core tip: Our results suggest wide variance in polyp size documentation. Neither endoscopist estimate nor pathologist measurement accurately reflects colonic polyp size. Inaccurate determination of polyp size can negatively impact advanced adenoma detection. Using a screen cursor like that used in ultrasound and computed tomography scanners may serve as a standardized, accurate technique to solve this issue.
- Citation: Izzy M, Virk MA, Saund A, Tejada J, Kargoli F, Anand S. Accuracy of endoscopists’ estimate of polyp size: A continuous dilemma. World J Gastrointest Endosc 2015; 7(8): 824-829
- URL: https://www.wjgnet.com/1948-5190/full/v7/i8/824.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i8.824
The incidence of colorectal cancer continues to rise to make it the fourth most common cancer in men and third most common cancer in women[1]. The concept of adenoma-carcinoma sequence has been already established by several studies[2-4]. The various characteristics that need to be considered upon evaluating the malignant potential of an adenomatous polyp are size, villous components and dysplasia[2,5]. These factors significantly impact the decision regarding follow up surveillance studies. While an experienced pathologist can precisely recognize the villous component or dysplastic changes in the polyp, achieving an accurate estimate of the polyp actual size remains challenging for the endoscopist as well as the pathologist.
With the growing importance of early detection of premalignant colonic polyps, accurate determination of polyp size becomes critical to recognize patients with potential to develop colon cancer. National and international guidelines consider polyp size as a key factor in determining follow up intervals with 10 mm cutoff as an important threshold for closer monitoring and surveillance[6,7]. Polyps less than 5 mm rarely show pre malignant histological features while a size over 10 mm has a 33% potential of pre malignant characteristics[8-10]. Polyp size is visually estimated during endoscopy. This is an approximate determination with variability between observers. Pathological measurements are made after excision using the untreated sample or after treatment with formaldehyde[11]. There is a possibility of incomplete estimation because some polyps are submitted piecemeal or fragmented. In addition, visual estimation is 2 dimensional while pathologic measurement is 3 dimensional[12]. Accurate estimation of polyp size also appears to be critical based on its location. Gupta et al[13] have reported advanced adenomas are more likely with a smaller size estimate on the right side of the colon. In this study, we aim to investigate the inconsistency, if any, between the endoscopist’s estimate and pathologist’s measurement of polyp size hoping to find a way to standardize the polyp size measurement.
Eighty-eight subjects who underwent endoscopic polypectomy over a two-year period were studied retrospectively. Data was collected on 111 excised polyps. Visual estimation by the endoscopist was rounded to the nearest millimeter. Pathological estimation after fixation with formaldehyde was obtained from biopsy pathology reports. Data regarding the method of polypectomy being biopsy forceps vs snare was collected from each procedure report and analyzed accordingly. Demographic data was collected, as well. We only included patients with clear numerical documentation of the polyp size by the pathologist and the endoscopist and clear documentation of method of polypectomy in the endoscopy report. Subjects with incomplete data or missing parameters were not included. Only cases that were cared for by the teaching consult service were included. From the entire cohort, a random selection of 88 cases that fulfill these criteria was made by our GI pathologist. In order to get a wide representation of all endoscopists and fellows rotating through our service, an average of 3-4 cases from each month over the course of 2 years was maintained.
Visual estimates were obtained using Olympus Evis Exera 111 (CF-HQ190L/I and PCF-HQ190L/I) colonovideoscopes with dual focus optical system and Narrow Band Imaging. Visual estimation was done by the endoscopists for snared polyps and in reference to open forceps for excisional biopsies. The method of polypectomy was determined based on the size of the polyp and type of its attachment, i.e., sessile or pedunculated. All study colonoscopies were performed by our 9 gastroenterology fellows under the supervision of 4 experienced faculty members. The documented size was agreed upon by the performing fellow and supervising faculty.
The pathologist was blinded to the visual estimate. The macroscopic measurement was done at the cut-up bench.
Retrospective analysis was performed comparing endoscopist visual estimate of polyp size and pathologist measurement. Continuous and categorical data were presented using means (± SD) and frequencies, respectively. Student t test was used to measure the difference of the means between different polypectomy techniques (snare vs excisional biopsy). Paired t test was used to estimate the difference of the means between the endoscopist and pathologist size determinations. Linear regression model was used to determine the predictors of the difference of the means between the two determinations (endoscopist vs pathologist). All statistical analysis was done using statistical analysis software (9.2, South Carolina).
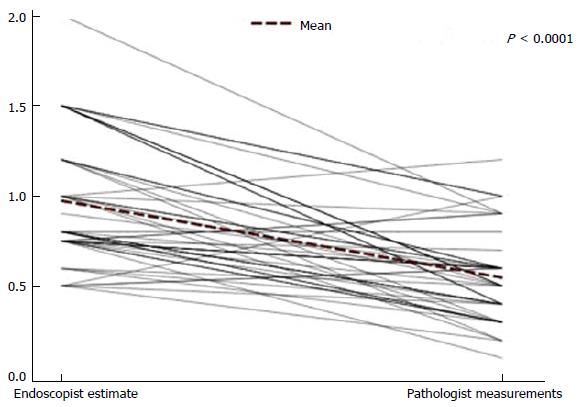
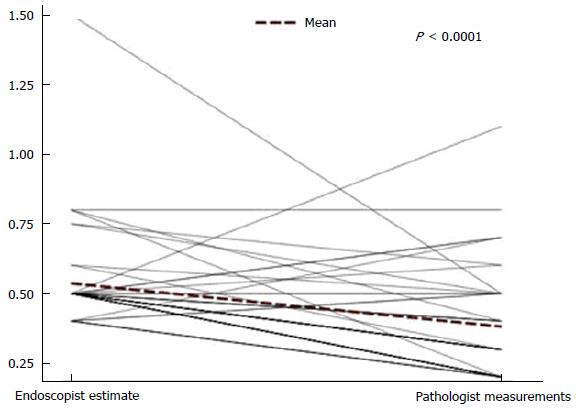
In our cohort, 37% were men and 63% were women with 75% African American, 21% Hispanic, 3% Caucasian and 1% Asian American. Fifty-two (46.8%) of the polyps were excised using biopsy forceps and 59 (53.2%) of the polyps were removed by snare polypectomy. In the biopsy excision group the mean visual size reported by the endoscopist was 0.54 ± 0.16 cm vs a mean polyp size of 0.38 ± 0.19 reported during pathological exam. The mean difference was 0.16 (95%CI: 0.09-0.215) (Figure 1). The location of the polyp did not have any impact on the reported measurements. In the snare polypectomy group the mean visual size reported by the endoscopist was 0.97 ± 0.34 cm vs a mean polyp size of 0.54 ± 0.24 reported during pathologist exam. The mean difference was 0.43 cm (95%CI: 0.33-0.52) (Figure 2). Visual overestimation in the biopsy excision group was 39% in comparison 77% in the snare polypectomy group (Table 1).
| Method of excision | Number of polyps | Mean endoscopist’s estimate | Mean pathologist’s measurement | Mean difference | Overestimate | P value |
| Biopsy excision | 52 | 0.54 (± 0.16) cm | 0.38 (± 0.19) cm | 0.16 cm | 39% | < 0.001 |
| Snare polypectomy | 59 | 0.97 (± 0.34) cm | 0.54 (± 0.24) cm | 0.43 cm | 77% | < 0.001 |
| Total | 111 | 0.76 (± 0.35) cm | 0.46 (± 0.23) cm | 0.3 cm | 65% | < 0.001 |
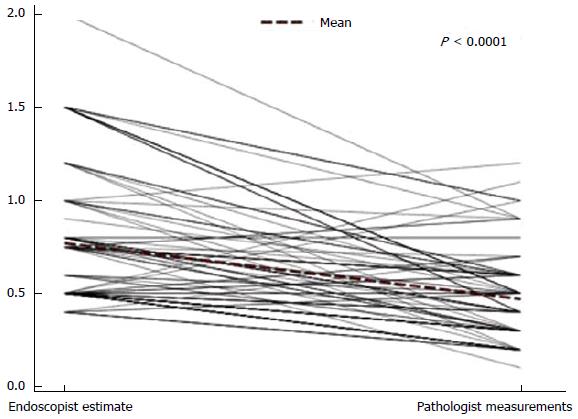
Combining both groups, the mean visual size was 0.76 ± 0.35 cm compared to 0.46 ± 0.23 cm by the pathologist. The mean difference was 0.3 cm (95%CI: 0.23-0.36). Visual estimates during endoscopy were within 1 mm of the pathologist measurement in 28 polyps (25%) and were within 2 mm in 52 polyps (46%) (Figure 3).
To date, our study is the largest in the field with special emphasis on the method of polypectomy as a factor affecting the endoscopist visual estimate. It also clearly shows that endoscopists tend to overestimate the polyp size; a fact that was previously considered a controversial concept. This study showed that endoscopists tend to overestimate the polyp size by 65% in comparison to the measurements reported by pathologists. This difference between polyp size measurement that was noted between the endoscopists and pathologists may be attributed to the physical damage of the specimen. The polyp may be damaged in situ during excision or the endoscopist may not remove the polyp in its entirety. This will result in a specimen being sent to the pathologist that is actually smaller than it was in situ. Another factor that could be considered is the formalin fixation effect on size shrinkage. However, previous studies have shown that there was no significant difference between post excision polyp size and post fixation measurement, which strongly argues against formalin impact on polyp size[14,15]. Piecemeal submission of polyp tissue for pathological exam can be a factor that results in discrepancies in size too. Furthermore, a study by Schoen et al[14] determined that the type of polyp had an impact on the estimated size. In their measurement of 61 polyps, of which, 44 were pedunculated, the size was overestimated by the endoscopist 55% of the time. The stalk on pedunculated polyps may cause the polyp to sit on an angle which makes it more difficult for the endoscopist to accurately estimate its size. In our study, no such observation was noted.
In the current study, only 46% of the endoscopists estimations were within 2 mm of the pathologic measurements. There appears to be a wide variance in the remaining 54% of the measurements. Several published studies support our conclusion that endoscopists overestimate polyp size. A study of 61 polyps concluded that endoscopists overestimated polyp size by greater than 3 mm in 20% of the cases[14]. Morales et al[15] determined that in a sample of 31 polyps the endoscopists’ estimates were on average 1.6 mm greater than the postpolypectomy measurement. Other studies contradict our findings by asserting that endoscopists underestimate polyp size. A study of 107 polyps conducted by Turner et al[16] concluded that on average both colonoscopists and pathologists significantly underestimate polyp size in comparison to the prefixation measurement. Another recent study on 35 polyps also concluded that colonoscopists underestimate polyp size in 74% of the cases[11]. However, this study of 35 polyps presents a potential bias due to its small sample size.
It is noteworthy that, in our study, endoscopists showed greater overestimation of size in the polyps that were removed by snare biopsy vs removal using biopsy forceps (77% vs 39%). This can suggest that larger polyps are likely to be overestimated than smaller ones.
One possible limitation of this study is the retrospective model rather than a prospective one. This makes the study rely on the merit of record keeping by the endoscopists and pathologists. Moreover, we also looked only at post fixation size and did not have adequate data on prefixation measurements. However, the latter factor is unlikely to impact our findings in view of previously published studies about the effect of formalin fixation.
In conclusion, this study determined that endoscopists tend to overestimate the size of colonic polyps. This was more pronounced in case of snared polyps in comparison to polyps excised by forceps. Considering the major importance of accurate polyp size estimation on detecting advanced adenoma, visual estimates provided in a non-standardized manner can result in significant inter-observer (endoscopist) variations. Pathology reports for the size are not reliable either considering that most polyps get some degree of physical damage upon removal, which directly affects the size. Use of measurement cursors is a standard practice during imaging studies such as sonography. We suggest that the addition of a measurement cursor to video endoscopes can standardize the visual estimates and provide accurate information to determine appropriate surveillance intervals allowing for better management and ultimately a decreased mortality rate from colon cancer.
Colonic polyp size is critical in determining the significance of the polyp and thus the colonoscopy surveillance interval. The inaccuracy in determining the size can have remarkable consequences represented by repeating colonoscopy earlier than needed in case of overestimating the actual polyp size or delaying a necessary procedure which might result in development of colorectal cancer in case of underestimating the polyp size.
There have been only few small studies that attempted to address the issue of estimating polyp size by the endoscopists. Those studies have shown inconsistent results in terms of endoscopists’ tendency to overestimate vs underestimate polyp size.
This study is, to date, the largest of its kind and it clearly shows that endoscopists tend to generally overestimate polyp size with wide variance in the overestimate. On the other hand, the pathologist’s measurement cannot be considered reliable given the possibility of physical damage or shrinkage of the polyp.
This study highlights the desperate need for an accurate standardized method of measuring colonic polyp size. To solve this issue, the authors suggest using cursors for colonoscopy screens like those used in ultrasound and computed tomography scanners.
This is a well-written manuscript. The retrospective nature of the study may actually be a plus as it gives a true representation of the endoscopists estimation of size as they would normally do in their routine practice.
| 1. | Center MM, Jemal A, Ward E. International trends in colorectal cancer incidence rates. Cancer Epidemiol Biomarkers Prev. 2009;18:1688-1694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 532] [Cited by in RCA: 568] [Article Influence: 33.4] [Reference Citation Analysis (0)] |
| 2. | Muto T, Bussey HJ, Morson BC. The evolution of cancer of the colon and rectum. Cancer. 1975;36:2251-2270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1522] [Cited by in RCA: 1389] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 3. | Winawer SJ, Zauber AG, Ho MN, O’Brien MJ, Gottlieb LS, Sternberg SS, Waye JD, Schapiro M, Bond JH, Panish JF. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329:1977-1981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3107] [Cited by in RCA: 3174] [Article Influence: 96.2] [Reference Citation Analysis (1)] |
| 4. | Citarda F, Tomaselli G, Capocaccia R, Barcherini S, Crespi M. Efficacy in standard clinical practice of colonoscopic polypectomy in reducing colorectal cancer incidence. Gut. 2001;48:812-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 511] [Cited by in RCA: 500] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 5. | Davila RE, Rajan E, Baron TH, Adler DG, Egan JV, Faigel DO, Gan SI, Hirota WK, Leighton JA, Lichtenstein D. ASGE guideline: colorectal cancer screening and surveillance. Gastrointest Endosc. 2006;63:546-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 225] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 6. | Atkin WS, Saunders BP. Surveillance guidelines after removal of colorectal adenomatous polyps. Gut. 2002;51 Suppl 5:V6-V9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 207] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 7. | Lieberman D, Moravec M, Holub J, Michaels L, Eisen G. Polyp size and advanced histology in patients undergoing colonoscopy screening: implications for CT colonography. Gastroenterology. 2008;135:1100-1105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 355] [Cited by in RCA: 334] [Article Influence: 18.6] [Reference Citation Analysis (1)] |
| 8. | Pickhardt PJ. The natural history of colorectal polyps and masses: rediscovered truths from the barium enema era. AJR Am J Roentgenol. 2007;188:619-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Welin S, Youker J, Spratt JS. The rates and patterns of growth of 375 tumors of the large intestine and rectum observed serially by double contrast enema study (malmoe technique). Am J Roentgenol Radium Ther Nucl Med. 1963;90:673-687. [PubMed] |
| 10. | Chen SC, Rex DK. Endoscopist can be more powerful than age and male gender in predicting adenoma detection at colonoscopy. Am J Gastroenterol. 2007;102:856-861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 310] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 11. | Chadebecq F, Tilmant C, Bartoli A. Measuring the size of neoplasia in colonoscopy using Depth-From-Defocus. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:1478-1481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Endoscopic Classification Review Group. Update on the paris classification of superficial neoplastic lesions in the digestive tract. Endoscopy. 2005;37:570-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 559] [Cited by in RCA: 675] [Article Influence: 32.1] [Reference Citation Analysis (2)] |
| 13. | Gupta S, Balasubramanian BA, Fu T, Genta RM, Rockey DC, Lash R. Polyps with advanced neoplasia are smaller in the right than in the left colon: implications for colorectal cancer screening. Clin Gastroenterol Hepatol. 2012;10:1395-1401.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Schoen RE, Gerber LD, Margulies C. The pathologic measurement of polyp size is preferable to the endoscopic estimate. Gastrointest Endosc. 1997;46:492-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 146] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 15. | Morales TG, Sampliner RE, Garewal HS, Fennerty MB, Aickin M. The difference in colon polyp size before and after removal. Gastrointest Endosc. 1996;43:25-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 81] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Turner JK, Wright M, Morgan M, Williams GT, Dolwani S. A prospective study of the accuracy and concordance between in-situ and postfixation measurements of colorectal polyp size and their potential impact upon surveillance. Eur J Gastroenterol Hepatol. 2013;25:562-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Bettington M, Septer S S- Editor: Gong XM L- Editor: A E- Editor: Wu HL