Published online Aug 10, 2015. doi: 10.4253/wjge.v7.i10.995
Peer-review started: March 12, 2015
First decision: March 20, 2015
Revised: April 22, 2015
Accepted: July 7, 2015
Article in press: July 8, 2015
Published online: August 10, 2015
Processing time: 159 Days and 2.9 Hours
AIM: To assess the endoscopic characteristics of gastric polyps and their association with Helicobacter pylori (H. pylori) status in a predominantly Hispanic population.
METHODS: We conducted a retrospective study of all esophagogastroduodenoscopies performed at our institution. Demographic, endoscopic and histopathological data were reviewed. Categorization of patients into Hispanic and Non-Hispanic was based on self-identification. Patients without resection/biopsy were not included in the analysis. Identification of polyps type was based on histological examination. One way analysis of variance was used to compare continuous variables among different polyp types and Fisher’s exact test was used compare categorical variables among polyp types. Unadjusted and adjusted comparisons of demographic and clinical characteristics were performed according to the H. pylori status and polyp type using logistic regressions.
RESULTS: Of 7090 patients who had upper endoscopy, 335 patients had gastric polyps (4.7%). Resection or biopsy of gastric polyps was performed in 296 patients (88.4%) with a total of 442 polyps removed or biopsied. Of 296 patients, 87 (29%) had hyperplastic polyps, 82 (28%) had fundic gland polyps and 5 (1.7%) had adenomatous polyps. Hyperplastic polyps were significantly associated with positive H. pylori status compared with fundic gland polyps (OR = 4.621; 95%CI: 1.92-11.13, P = 0.001). Hyperplastic polyps were also found to be significantly associated with portal hypertensive gastropathy compared with fundic gland polyps (OR = 6.903; 95%CI: 1.41-33.93, P = 0.0174). Out of 296 patients, 30 (10.1%) had a follow-up endoscopy with a mean duration of 26 ± 16.3 mo. Interval development of cancer was not noted in any of the patients during follow up period.
CONCLUSION: Gastric hyperplastic polyps were significantly associated with positive H. pylori status and portal hypertensive gastropathy as compared with fundic gland polyps.
Core tip: In a predominantly Hispanic population, the most common gastric polyps were hyperplastic and fundic gland polyps (more than half of gastric polyps). Gastric hyperplastic polyps were significantly associated with positive Helicobacter pylori status and portal hypertensive gastropathy as compared with fundic gland polyps. Hyperplastic polyps and fundic gland polyps were more prevalent in chronic gastritis, while adenomatous polyps were associated with intestinal metaplasia.
- Citation: Elhanafi S, Saadi M, Lou W, Mallawaarachchi I, Dwivedi A, Zuckerman M, Othman MO. Gastric polyps: Association with Helicobacter pylori status and the pathology of the surrounding mucosa, a cross sectional study. World J Gastrointest Endosc 2015; 7(10): 995-1002
- URL: https://www.wjgnet.com/1948-5190/full/v7/i10/995.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i10.995
Gastric polyps can be defined as abnormal luminal growths projecting above the plane of the mucosal surface. The incidence of gastric polyps has been estimated to be between 2% and 6%. The incidence of gastric polyps is gradually increasing due to expanded indications and widespread use of endoscopic examinations[1-4]. Gastric polyps are usually asymptomatic and discovered incidentally during endoscopic examination, but on rare occasions they can present with nonspecific symptoms such as abdominal pain, gastrointestinal bleeding, anemia, or symptoms of gastric outlet obstruction[5-8]. Determination of gastric polyp type is important as the risk for malignant transformation depends on the histopathological nature of the polyp[9-12]. The frequency of different types of gastric polyps varies widely depending on the population studied. It has been reported that hyperplastic polyps are relatively more frequent than fundic gland polyps in regions where Helicobacter pylori (H. pylori) infection is common[1,13]. A higher prevalence of H. pylori infection has been documented in Hispanics living in United States regions bordering Mexico compared with non-border areas[14,15]. There is a paucity of published data from the United States regarding the nature and various characteristics of gastric polyps, especially in Hispanics and other immigrant groups. The aim of this study is to assess the prevalence of gastric polyps and their endoscopic and histological characteristics in a predominantly Hispanic population on the United States-Mexico border.
After receiving approval from Texas Tech University Institutional Review Board, we retrospectively reviewed all esophagogastroduodenoscopies (EGDs) performed at the University Medical Center, El Paso, TX for all indications. The review period of the study was from November 1, 2007 to July 30, 2013. The electronic database system (ProVation®, Minneapolis, MN) was used to identify the patient’s demographic data, the indication for the procedure and gastric polyp characteristics. Categorization of patients into Hispanic and Non-Hispanic was based on self-identification. Patients without resection/biopsy were not included in the analysis. Identification of polyps type was based on histological examination.
Quantitative variables were described using the mean ± SD, whereas categorical variables were described using the frequency and proportion. One way analysis of variance was used to compare continuous variables among different polyp types and Fisher’s exact test was used compare categorical variables among polyp types. Unadjusted and adjusted comparisons of demographic and clinical characteristics were performed according to the H. pylori status and polyp type using logistic regressions. The logistic regression analysis for H. pylori status was conducted after removing H. pylori not tested patients. The logistic regression was used to find out factors associated with hyperplastic polyp type as compared with fundic polyp type after removing patients with adenoma, mixed polyps, and others. The results of logistic regression analysis were reported using odds ratio (OR), 95%CI and P values. Stepwise selection method using probability to enter = 0.10 and probability to stay = 0.05 was used to obtain the final model. All the statistical analyses were carried out using statistical analysis software (SAS) 9.3. Results were considered significant at the 5% level of significance. The statistical methods of this study were reviewed by Dr. Alok Dwivedi from the department of Biostatistics at Texas Tech University HSC at El Paso.
A total of 7090 patients underwent 9450 EGD procedures. Of these, 335 patients had gastric polyps (4.7%). Resection or biopsy of 442 gastric polyps was done in 296 patients (88.4%). 39 patients did not undergo resection or biopsy of their gastric polyps because of the high risk of bleeding or obvious endoscopic diagnosis of fundic gland polyps (FGPs). The mean age of the patients was 58 years (SD: ± 12 years). The majority of the patients were females (74%) and most were Hispanics (85%). Portal hypertensive gastropathy was seen in 20 patients (7%).
Polyps’ histology: Of 296 patients, 87 (29%) patients had hyperplastic polyps and 82 (28%) patients had fundic gland polyps. There were 5 (1.7%) patients with adenomatous polyps while 13 (4.4%) patients had mixed types of polyps. Histology results of the remaining polyps revealed chronic gastritis in 41 patients (14%), intestinal metaplasia in 12 patients (4.1%), faveolar hyperplasia in 10 patients (3.4%), carcinoid tumor in 4 patients (1.4%) and granulation tissue polyps in 4 patients (1.4%). Adenocarcinoma, gastric xanthelasma, hamartomatous polyps, lymphoid follicles and submucosal brunner glands were each found in 2 patients (0.68%). There was one patient with lipoma. The histology of resected or biopsied polyp was normal in 27 patients (9.1%).
Pathology of the surrounding mucosa: Out of 296 patients, 266 (89.8%) patients had biopsies of the surrounding mucosa (Table 1).
| Polyp’s type | Total patients (n = 296) | Percentage |
| Hyperplastic polyp | 87 | 29.39 |
| Fundic gland polyp | 82 | 27.7 |
| Chronic gastritis | 41 | 13.85 |
| Mixed | 13 | 4.39 |
| Intestinal metaplasia | 12 | 4.05 |
| Foveolar hyperplasia | 10 | 3.38 |
| Adenoma | 5 | 1.69 |
| Carcinoid tumor | 4 | 1.35 |
| Granulation tissue polyp | 4 | 1.35 |
| Adenocarcinoma | 2 | 0.68 |
| Gastric xanthelasma | 2 | 0.68 |
| Hamartomatous polyp | 2 | 0.68 |
| Lymphoid follicles | 2 | 0.68 |
| Submucosal Brunner glands | 2 | 0.68 |
| Lipoma | 1 | 0.34 |
| Normal | 27 | 9.12 |
Of these, 190 (64%) patients had chronic gastritis while 25 (8%) patients had intestinal metaplasia. Thirty (10%) patients were not biopsied. In regards to H. pylori status, H. pylori were positive in 71 (24%) patients, and negative in 211 (71%) patients, while 14 patients were not tested.
Clinical characteristics of gastric polyps: Table 2 shows the distribution of patient and clinical characteristics according to five categories (Adenoma, Hyperplastic, Fundic gland, Mixed and other) of polyps. The gender and ethnicity distributions were not found to be significantly different among different polyp types. The distribution of age, pathology of surrounding gastric mucosa, and H. pylori status were found to be associated with different polyp types. Adenomatous polyps were more common in advanced age (P < 0.0013). Fundic, hyperplastic and mixed polyps were more frequent in chronic gastritis while adenomatous polyps were more common (60%) in intestinal metaplasia (P < 0.001). Thirty-one percent of the patients with hyperplastic polyps tested positive for H. pylori status while 9.8% of the patients with fundic gland polyps tested positive for H. pylori. Portal hypertensive gastropathy was seen in 11.5% of patients with hyperplastic polyps compared to 2.4% of patients with fundic gland polyps.
| Cofactor | Adenoman = 5 | Fundicn = 82 | Hyperplasticn = 87 | Mixedn = 13 | Othern = 109 | P value |
| Age (yr), mean ± SD | 75.4 (3.3) | 54.7 (13.0) | 58.4 (10.8) | 62.2 (14.0) | 57.7 (11.9) | 0.0013 |
| Gender | 0.2086 | |||||
| Female | 5 (100.0) | 67 (81.71) | 64 (73.56) | 9 (69.23) | 75 (68.81) | |
| Male | 0 (0.00) | 15 (18.29) | 23 (26.44) | 4 (30.77) | 34 (31.19) | |
| Ethnicity | 0.7427 | |||||
| Hispanic | 5 (100.0) | 66 (80.49) | 77 (88.51) | 11 (84.62) | 93 (85.32) | |
| Non-Hispanic White | 0 (0.00) | 5 (6.10) | 4 (4.60) | 0 (0.00) | 8 (7.34) | |
| Other | 0 (0.00) | 11 (13.41) | 6 (6.90) | 2 (15.38) | 8 (7.34) | |
| Pathology of surrounding gastric | < 0.00011 | |||||
| Chronic gastritis | 0 (0.00) | 51 (62.20) | 52 (59.77) | 9 (69.23) | 78 (41.05) | |
| Intestinal metaplasia | 3 (60.00) | 1 (1.22) | 6 (6.90) | 1 (7.69) | 14 (56.00) | |
| Other | 0 (0.00) | 22 (26.83) | 15 (17.24) | 2 (15.38) | 5 (16.67) | |
| Not biopsied | 2 (40.00) | 8 (9.76) | 14 (16.09) | 1 (7.69) | 12 (23.53) | |
| Helicobacter pylori status | 0.00061 | |||||
| Negative | 4 (80.00) | 70 (85.37) | 52 (59.77) | 11 (84.62) | 74 (35.07) | |
| Positive | 0 (0.00) | 8 (9.76) | 27 (31.03) | 2 (15.38) | 34 (47.89) | |
| Not tested | 1 (20.00) | 4 (4.88) | 8 (9.20) | 0 (0.00) | 1 (7.14) | |
| Portal hypertensive gastropathy | 0.1821 | |||||
| No | 5 (100.0) | 80 (97.56) | 77 (88.51) | 12 (92.31) | 102 (93.58) | |
| Yes | 0 (0.00) | 2 (2.44) | 10 (11.49) | 1 (7.69) | 7 (6.42) | |
Associations of H. pylori status and gastric pathology: The prevalence of hyperplastic polyps was 34% in the H. pylori positive group while the prevalence of fundic polyps was 10% in the H. pylori positive group. Table 3 shows the unadjusted and adjusted associations of cofactors with H. pylori status. Only the polyp type and the pathology of surrounding gastric mucosa were associated with H. pylori in unadjusted and adjusted models. Hyperplastic polyps have a 4.6 times higher odds of having a positive H. pylori status compared to fundic gland polyps (OR = 4.621; 95%CI: 1.92-11.13, P = 0.001).
| Cofactor | Unadjusted OR(95%CI), P value | Adjusted OR(95%CI), P value |
| Age (yr) | 1.011 (0.988-1.034), 0.3686 | |
| Polyp type | ||
| Fundic (referent) | 1 | 1 |
| Hyperplastic | 4.621 (1.918-11.133), 0.0006 | 4.621 (1.861-11.479), 0.0010 |
| Other | 3.469 (1.509-7.976), 0.0034 | 2.952 (1.250-6.972), 0.0136 |
| Gender | ||
| Female (referent) | 1 | |
| Male | 0.891 (0.460-1.726), 0.7321 | |
| Ethnicity | ||
| Hispanic (referent) | 1 | |
| Non-hispanic White | 0.205 (0.026-1.605), 0.1311 | |
| Other | 0.409 (0.117-1.435), 0.1629 | |
| Pathology of surrounding gastric | ||
| Chronic gastritis (referent) | 1 | 1 |
| Intestinal metaplasia | 0.996 (0.407-2.437), 0.9931 | 0.827 (0.331-2.065), 0.6848 |
| Other | 0.088 (0.021-0.375), 0.0010 | 0.090 (0.021-0.390), 0.0013 |
| Portal hypertension | ||
| No (referent) | 1 | |
| Yes | 0.569 (0.159-2.044), 0.3877 | |
Cofactors association of hyperlastic and fundic gland polyps: Table 4 shows the unadjusted and adjusted associations of cofactors with hyperplastic polyps as compared with fundic polyps. In the unadjusted analysis, age, H. pylori status and portal hypertension were found to be associated with hyperplastic polyps. Per unit increase in age increased the odds of hyperplastic polyp type by 3% as compared with fundic gland polyp. After adjusting for all other factors, H. pylori status and portal hypertensive gastropathy were the only remained significant factors in the final adjusted model. Positive H. pylori status has 5.3 times higher odds to have hyperplastic polyps compared with negative H. pylori status (OR = 5.285; 95%CI: 2.17-12.89, P = 0.0003) after adjusting for portal hypertensive gastropathy. Patients with portal hypertensive gastropathy are 6.4 times more likely to have hyperplastic polyps after adjusting for H. pylori status (OR = 6.903; 95%CI: 1.40-33.93, P = 0.0174).
| Cofactor | Unadjusted OR(95%CI), P value | Adjusted OR(95%CI), P value |
| Age (yr) | 1.031 (1.001-1.062), 0.0419 | |
| H. pylori status | ||
| Negative (referent) | 1 | 1 |
| Positive | 4.622 (1.918-11.137), 0.0006 | 5.285 (2.166-12.892), 0.0003 |
| Gender | ||
| Female (referent) | 1 | |
| Male | 1.804 (0.756-4.303), 0.1837 | |
| Ethnicity | ||
| Hispanic (referent) | 1 | |
| Non-Hispanic White | 0.469 (0.083-2.655), 0.3922 | |
| Other | 0. 536 (0.150-1.923), 0.3390 | |
| Pathology of surrounding gastric | ||
| Chronic gastritis (referent) | 1 | |
| Intestinal metaplasia | 5.997 (0.697-51.614), 0.1029 | |
| Other | 0.714 (0.331-1.542), 0.3917 | |
| Portal hypertension | ||
| No (referent) | 1 | 1 |
| Yes | 5.080 (1.057-24.414), 0.0424 | 6.903, 0.0174 |
Out of 296 patients, 30 (10.1%) had a follow-up endoscopy with a mean duration of 26 ± 16.3 mo. Out of these 30 patients, 11 (36.6%) had hyperplastic polyps, 5 had chronic gastritis polyp, 4 had fundic gland polyp, two had intestinal metaplasia, two had carcinoid tumor, two had faveloar hyperplasia, one had adenomatous polyp and 3 patients were classified as other (gastric adenocarcinoma, brunner gland hyperplasia and normal pathology). Polyp’s recurrence was noted in five out of eleven hyperplastic polyps and one out of four fundic gland polyps surveyed.
All Five adenomatous polyps were polypectomized during the initial endoscopy session. Four out of the five patients with adenomatous polyps were lost to follow-up in our system. Recurrence of the adenomatous polyp was noted in the one patient who had surveillance endoscopy.
Interval development of cancer was not noted in any of the patients during follow up period.
In this study, we found the prevalence of gastric polyps to be 4.7% in a predominantly Hispanic population, which is similar to the reported spectrum in previous series[1,13,16,17]. However, there is wide variation in the reported frequencies of different histological subtypes. Fundic gland polyps and hyperplastic polyps are the most prevalent types of gastric polyps in the current literature[1,2,16]. This was found in our study as well. We found 29% prevalence of hyperplastic polyps and 28% prevalence of fundic polyps. In addition, our data confirmed the positive association between H. pylori infection and hyperplastic polyps compared to fundic gland polyps.
There are several subtypes of gastric polyps which can be classified based on their endoscopic appearance or histopathological features. One of the most popular classifications is dividing the gastric polyps into two categories; epithelial and subepithelial. Epithelial polyps include fundic gland polyps, hyperplastic polyps, adenomatous polyps, polyps associated with familial adenomatous polyposis (FAP) and Peutz-Jeghers syndrome. Subepithelial polyps include gastrointestinal stromal tumors (GISTs]), inflammatory fibroid polyps, pancreatic heterotopia, leiomyomas, neuroendocrine tumors and granular cell tumors[17].
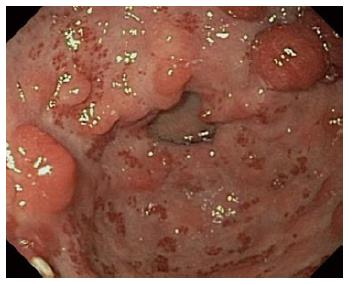
In our study, hyperplastic polyps were the most frequent subtype of polyps. We found a strong association between hyperplastic polyps, chronic gastritis and H. pylori infection which confirms what was reported in other studies[18,19]. A higher prevalence of H. pylori infection has been documented in Hispanics living in United States-Mexico border regions compared with non-border areas, which may explain the relatively high prevalence of hyperplastic polyps in our study population[14,15,20,21]. The risk of dysplasia and neoplastic progression of hyperplastic polyps is controversial with wide discrepancy between the reported rates (1.9% to 19%)[19,22-24]. However, this type of polyp has been reported to have an increased risk of neoplasia in the surrounding abnormal mucosa and is associated with higher incidence of synchronous gastric cancer[3,25]. In our series, 11 out of 87 patients who were found to have hyperplastic polyps, had follow-up endoscopy with a mean duration of 30 ± 18 mo. Five (45%) of these 11 patients were found to have residual polyps in follow up endoscopy and none (0%) of them developed dysplasia or cancer. Given this higher risk of developing adenocarcinoma in the surrounding mucosa of hyperplastic polyp, the guidelines recommend obtaining multiple biopsies of the intervening mucosa[26]. Polyp resection has been recommended for any hyperplastic polyp greater than 0.5 cm in size. Repeat surveillance endoscopy is recommended at 1 year after endoscopic resection[22,27,28]. Regression of hyperplastic polyps has been reported in many studies after effective treatment of H. pylori infection, it is thus essential to treat the patients with active H. pylori infection before entertaining any further management[18,19,29,30] (Figure 1).
FGPs were found to be the second most frequent type of polyp in our study population. The highest prevalence of fundic gland polyps was reported by Carmack et al[1] in a nationwide United States population from 2007-2008 in which FGP constituted 77% of the study cohort. FGP can be found sporadically or in patients with FAP syndrome[31,32]. Sporadic FGP has been reported in many studies to have a positive association with prolonged use of proton pump inhibitors (PPI)[33-36]. However, in other series this correlation was not confirmed[37,38]. Jalving et al[36] reported up to 4-times increased risk of fundic gland polyps with long-term proton pump inhibitor, and Ally et al[33] reported that the duration of PPI therapy greater than 4 years is an independent predictor for FGP development regardless of the used dosage. Due to the retrospective nature of our study, we were unable to obtain accurate data regarding PPI use among the study population. FGPs have been reported to have a negative association with the presence of H. pylori infection[39]. This was found in our study as well. The risk of dysplasia in sporadic FGPs is rare, while it occurs in 25%-41% of FAP-associated polyps[31,40]. Biopsy of FGPs is recommended to exclude dysplasia or adenocarcinoma. Polyp resection is recommended for FGPs more than 1 cm in size to eliminate sampling error by missing any neoplastic foci within the polyp[26,41]. Further workup is recommended to exclude FAP in patients who are less than 40 years of age with numerous FGPs, or if the initial polyp biopsy showed dysplasia[26].
Raised Intraepithelial Neoplasia is the recent nomenclature for gastric adenomas as they are at increased risk for malignant transformation[3,42,43]. Three (60%) of the gastric adenomas in our study were associated with underlying atrophic gastritis and intestinal metaplasia which confirms what was reported in other studies[42,44]. The malignant potential of adenomatous polyps correlates with the polyp size and the age of the patient[3,24,45-47]. Polyps more than 2 cm in size had been reported to have higher risk of development of adenocarcinoma[3,45]. The guidelines recommend complete endoscopic removal of gastric adenomas or referral for surgical resection if lesions are not amenable to endoscopic resection or if they contain invasive carcinoma[26,27]. In addition, careful examination of the rest of the gastric mucosa and obtaining multiple biopsies is recommended to rule out any synchronous neoplastic process. In 2006, the American Society of Gastrointestinal Endoscopy guideline recommended endoscopic surveillance at 1 year for adenomatous polyps. The 2010 British Society of Gastroenterology guidelines recommended to repeat the endoscopic examination at 6 mo for incompletely resected adenomatous polyps or those with high grade dysplasia[26,27].
In our series, 20 (6.76%) patients were found to have portal hypertensive gastropathy. Half of these patients were found to have hyperplastic polyps. However, it has been reported that hyperplastic polyps in portal hypertensive patients are pathologically distinct from the typical hyperplastic polyps seen in nonportal hypertensive patients with uncertain malignant potential[48-52]. Management of portal hypertensive polyps is difficult as patients are at increased risk of post-polypectomy bleeding due to associated thrombocytopenia and coagulopathy. Conservative management and follow up endoscopy has been suggested as a safer strategy than multiple polypectomies[49,52].
There are some limitations to our study. One of the main drawbacks in our study is the lack of information on PPI use for the study cohort. As a result, we were unable to study the correlation between the various types of gastric polyps and PPI use. Second, this study was designed as a retrospective study with its obvious drawbacks. Although this study was performed in a unique practice setting on the United States-Mexico international border and the database used is significantly large, our results may not be applicable to all settings as our study is single-center study. However, one of the significant strengths of this study is the fact that the majority of the study population is Hispanic (85%) which may give more insight about the characteristics and the histopathologic features of gastric polyps in Hispanics.
In conclusion, the prevalence of gastric polyps in a predominantly Hispanic population is similar to what has been reported in the literature for other populations. Hyperplastic polyps were significantly associated with positive H. pylori status and portal hypersensitive gastropathy. Hyperplastic polyps and FGPs were more prevalent in chronic gastritis, while adenomatous polyps were associated with intestinal metaplasia.
Gastric polyps are usually asymptomatic and incidentally discovered during endoscopic examination. Determination of gastric polyp type is important as the risk for malignant transformation depends on the histopathological type.
The relationship between Helicobacter pylori (H. pylori) and the different types of gastric polyps is not well studied.
This is one of a few studies focused on the prevalence and distribution of gastric polyps in Hispanic populations. Hyperplastic and fundic gland polyps accounted for more than half of the resected polyps in this study. Gastric hyperplastic polyps were significantly associated with positive H. pylori status and portal hypertensive gastropathy as compared with fundic gland polyps. Hyperplastic polyps and fundic gland polyps were more prevalent in chronic gastritis, while adenomatous polyps were associated with intestinal metaplasia.
When Hyperplastic polyp is suspected, biopsy of the surrounding mucosa should be done to rule out H. pylori infection. In case of an adenomatous polyp, biopsy of the surrounding mucosa should be done to rule out intestinal metaplasia.
FGPs: Fundic Galnd Polyps; EGDs: Esophagogastroduodenoscopies.
The manuscript is concise, fluent and well-written. Strengths are the number of cases and the ethnicity orientation of the study group. The main drawback is that there is no new knowledge added, apart from ethnicity-targeted results. However, this is still of notice.
| 1. | Carmack SW, Genta RM, Schuler CM, Saboorian MH. The current spectrum of gastric polyps: a 1-year national study of over 120,000 patients. Am J Gastroenterol. 2009;104:1524-1532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 202] [Article Influence: 11.9] [Reference Citation Analysis (1)] |
| 2. | García-Alonso FJ, Martín-Mateos RM, González Martín JA, Foruny JR, Vázquez-Sequeiros E, Boixeda de Miquel D. Gastric polyps: analysis of endoscopic and histological features in our center. Rev Esp Enferm Dig. 2011;103:416-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 3. | Laxén F, Sipponen P, Ihamäki T, Hakkiluoto A, Dortscheva Z. Gastric polyps; their morphological and endoscopical characteristics and relation to gastric carcinoma. Acta Pathol Microbiol Immunol Scand A. 1982;90:221-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Carmack SW, Genta RM, Graham DY, Lauwers GY. Management of gastric polyps: a pathology-based guide for gastroenterologists. Nat Rev Gastroenterol Hepatol. 2009;6:331-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 99] [Article Influence: 5.8] [Reference Citation Analysis (1)] |
| 5. | Oberhuber G, Stolte M. Gastric polyps: an update of their pathology and biological significance. Virchows Arch. 2000;437:581-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 68] [Article Influence: 2.6] [Reference Citation Analysis (1)] |
| 6. | Secemsky BJ, Robinson KR, Krishnan K, Matkowskyj KA, Jung BH. Gastric hyperplastic polyps causing upper gastrointestinal hemorrhage in a young adult. World J Clin Cases. 2013;1:25-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (4)] |
| 7. | Aydin I, Ozer E, Rakici H, Sehitoglu I, Yucel AF, Pergel A, Sahin DA. Antral hyperplastic polyp: A rare cause of gastric outlet obstruction. Int J Surg Case Rep. 2014;5:287-289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Nayudu SK, Niazi M, Balar B, Kumbum K. A rare complication of hyperplastic gastric polyp. Case Rep Gastrointest Med. 2013;2013:631975. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (6)] |
| 9. | Tomasulo J. Gastric polyps. Histologic types and their relationship to gastric carcinoma. Cancer. 1971;27:1346-1355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Eichhorn K, Kratzsch KH, Stibenz J, Waller H, Winkelvoss H. Relations between stomach polyps and stomach cancer--results of follow-up after endoscopic polypectomy. Z Gesamte Inn Med. 1986;41:433-435. [PubMed] |
| 11. | Nechipaĭ AM, Poddubnyĭ BK, Kuvshinov IuP, Efimov ON, Rottenberg VI. The probability of malignant degeneration of stomach polyps. Vopr Onkol. 1989;35:1044-1049. [PubMed] |
| 12. | Orlowska J, Jarosz D, Pachlewski J, Butruk E. Malignant transformation of benign epithelial gastric polyps. Am J Gastroenterol. 1995;90:2152-2159. [PubMed] |
| 13. | Archimandritis A, Spiliadis C, Tzivras M, Vamvakousis B, Davaris P, Manika Z, Scandalis N. Gastric epithelial polyps: a retrospective endoscopic study of 12974 symptomatic patients. Ital J Gastroenterol. 1996;28:387-390. [PubMed] |
| 14. | Cardenas VM, Mena KD, Ortiz M, Karri S, Variyam E, Behravesh CB, Snowden KF, Flisser A, Bristol JR, Mayberry LF. Hyperendemic H. pylori and tapeworm infections in a U.S.-Mexico border population. Public Health Rep. 2010;125:441-447. [PubMed] |
| 15. | Mapel D, Roberts M, Overhiser A, Mason A. The epidemiology, diagnosis, and cost of dyspepsia and Helicobacter pylori gastritis: a case-control analysis in the Southwestern United States. Helicobacter. 2013;18:54-65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Csontos AA, Fekete B, Lőrinczy K, Terjék O, Berczi L, Juhász M, Miheller P, Tulassay Z. Prevalence of gastric polypoid lesions at an endoscopic facility. Orv Hetil. 2013;154:770-774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Cao H, Wang B, Zhang Z, Zhang H, Qu R. Distribution trends of gastric polyps: an endoscopy database analysis of 24 121 northern Chinese patients. J Gastroenterol Hepatol. 2012;27:1175-1180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (2)] |
| 18. | Ljubicić N, Banić M, Kujundzić M, Antić Z, Vrkljan M, Kovacević I, Hrabar D, Doko M, Zovak M, Mihatov S. The effect of eradicating Helicobacter pylori infection on the course of adenomatous and hyperplastic gastric polyps. Eur J Gastroenterol Hepatol. 1999;11:727-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 37] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 19. | Dirschmid K, Platz-Baudin C, Stolte M. Why is the hyperplastic polyp a marker for the precancerous condition of the gastric mucosa? Virchows Arch. 2006;448:80-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 63] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Goodman KJ, Correa P. The transmission of Helicobacter pylori. A critical review of the evidence. Int J Epidemiol. 1995;24:875-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 156] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 21. | Graham D. Public health issues relating to Helicobacter pylori infection and global eradication. Gastritis Philadelphia: Lippincott Williams and Wilkins 1999; 241-246. |
| 22. | Daibo M, Itabashi M, Hirota T. Malignant transformation of gastric hyperplastic polyps. Am J Gastroenterol. 1987;82:1016-1025. [PubMed] |
| 23. | Hizawa K, Fuchigami T, Iida M, Aoyagi K, Iwashita A, Daimaru Y, Fujishima M. Possible neoplastic transformation within gastric hyperplastic polyp. Application of endoscopic polypectomy. Surg Endosc. 1995;9:714-718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Cristallini EG, Ascani S, Bolis GB. Association between histologic type of polyp and carcinoma in the stomach. Gastrointest Endosc. 1992;38:481-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Hattori T. Morphological range of hyperplastic polyps and carcinomas arising in hyperplastic polyps of the stomach. J Clin Pathol. 1985;38:622-630. [PubMed] |
| 26. | Goddard AF, Badreldin R, Pritchard DM, Walker MM, Warren B. The management of gastric polyps. Gut. 2010;59:1270-1276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 148] [Article Influence: 9.3] [Reference Citation Analysis (1)] |
| 27. | Hirota WK, Zuckerman MJ, Adler DG, Davila RE, Egan J, Leighton JA, Qureshi WA, Rajan E, Fanelli R, Wheeler-Harbaugh J. ASGE guideline: the role of endoscopy in the surveillance of premalignant conditions of the upper GI tract. Gastrointest Endosc. 2006;63:570-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 369] [Cited by in RCA: 318] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 28. | Ginsberg GG, Al-Kawas FH, Fleischer DE, Reilly HF, Benjamin SB. Gastric polyps: relationship of size and histology to cancer risk. Am J Gastroenterol. 1996;91:714-717. [PubMed] |
| 29. | Ohkusa T, Takashimizu I, Fujiki K, Suzuki S, Shimoi K, Horiuchi T, Sakurazawa T, Ariake K, Ishii K, Kumagai J. Disappearance of hyperplastic polyps in the stomach after eradication of Helicobacter pylori. A randomized, clinical trial. Ann Intern Med. 1998;129:712-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 87] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 30. | Tokunaga K, Tanaka A, Takahashi S. [Gastric hyperplastic polyps and H. pylori infection, their relationship and effects of eradication therapy]. Nihon Rinsho. 2013;71:1449-1452. [PubMed] |
| 31. | Burt RW. Gastric fundic gland polyps. Gastroenterology. 2003;125:1462-1469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 78] [Article Influence: 3.4] [Reference Citation Analysis (1)] |
| 32. | Attard TM, Cuffari C, Tajouri T, Stoner JA, Eisenberg MT, Yardley JH, Abraham SC, Perry D, Vanderhoof J, Lynch H. Multicenter experience with upper gastrointestinal polyps in pediatric patients with familial adenomatous polyposis. Am J Gastroenterol. 2004;99:681-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 64] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 33. | Ally MR, Veerappan GR, Maydonovitch CL, Duncan TJ, Perry JL, Osgard EM, Wong RK. Chronic proton pump inhibitor therapy associated with increased development of fundic gland polyps. Dig Dis Sci. 2009;54:2617-2622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 34. | Hegedus I, Csizmadia C, Lomb Z, Cseke L, Enkh-Amar Y, Pajor L, Bogner B. [Massive fundic gland polyposis caused by chronic proton pump inhibitor therapy]. Orv Hetil. 2012;153:351-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 35. | Zelter A, Fernández JL, Bilder C, Rodríguez P, Wonaga A, Dorado F, Galich M, Viola LA. Fundic gland polyps and association with proton pump inhibitor intake: a prospective study in 1,780 endoscopies. Dig Dis Sci. 2011;56:1743-1748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 36. | Jalving M, Koornstra JJ, Wesseling J, Boezen HM, DE Jong S, Kleibeuker JH. Increased risk of fundic gland polyps during long-term proton pump inhibitor therapy. Aliment Pharmacol Ther. 2006;24:1341-1348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 167] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 37. | Vieth M, Stolte M. Fundic gland polyps are not induced by proton pump inhibitor therapy. Am J Clin Pathol. 2001;116:716-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 68] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 38. | Declich P, Ambrosiani L, Bellone S, Tavani E, Prada A, Bortoli A, Gozzini C. Fundic gland polyps under omeprazole treatment. Am J Clin Pathol. 1999;112:576-577. [PubMed] |
| 39. | Watanabe N, Seno H, Nakajima T, Yazumi S, Miyamoto S, Matsumoto S, Itoh T, Kawanami C, Okazaki K, Chiba T. Regression of fundic gland polyps following acquisition of Helicobacter pylori. Gut. 2002;51:742-745. [PubMed] |
| 40. | Bianchi LK, Burke CA, Bennett AE, Lopez R, Hasson H, Church JM. Fundic gland polyp dysplasia is common in familial adenomatous polyposis. Clin Gastroenterol Hepatol. 2008;6:180-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 145] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 41. | Chandrasekhara V, Ginsberg GG. Endoscopic management of gastrointestinal stromal tumors. Curr Gastroenterol Rep. 2011;13:532-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 42. | Kamiya T, Morishita T, Asakura H, Miura S, Munakata Y, Tsuchiya M. Long-term follow-up study on gastric adenoma and its relation to gastric protruded carcinoma. Cancer. 1982;50:2496-2503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 43. | Nakamura K, Sakaguchi H, Enjoji M. Depressed adenoma of the stomach. Cancer. 1988;62:2197-2202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 44. | Ito H, Hata J, Yokozaki H, Nakatani H, Oda N, Tahara E. Tubular adenoma of the human stomach. An immunohistochemical analysis of gut hormones, serotonin, carcinoembryonic antigen, secretory component, and lysozyme. Cancer. 1986;58:2264-2272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 45. | Abraham SC, Park SJ, Lee JH, Mugartegui L, Wu TT. Genetic alterations in gastric adenomas of intestinal and foveolar phenotypes. Mod Pathol. 2003;16:786-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 80] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 46. | Park do Y, Lauwers GY. Gastric polyps: classification and management. Arch Pathol Lab Med. 2008;132:633-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 47. | Nakamura T, Nakano G. Histopathological classification and malignant change in gastric polyps. J Clin Pathol. 1985;38:754-764. [PubMed] |
| 48. | Amarapurkar AD, Amarapurkar D, Choksi M, Bhatt N, Amarapurkar P. Portal hypertensive polyps: distinct entity. Indian J Gastroenterol. 2013;32:195-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 49. | Lam MC, Tha S, Owen D, Haque M, Chatur N, Gray JR, Yoshida EM. Gastric polyps in patients with portal hypertension. Eur J Gastroenterol Hepatol. 2011;23:1245-1249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 50. | Pai CG. Portal hypertensive polyp--what is in a name? Indian J Gastroenterol. 2013;32:163-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 51. | Lee TH, Jang JY, Jeong SW, Jin SY. Gastric polyposis associated with portal hypertension. Korean J Intern Med. 2013;28:261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 52. | Boyd JT, Lee L. Portal hypertension-associated gastric polyps. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Giannopoulos GA, Sieg A S- Editor: Tian YL L- Editor: A E- Editor: Wu HL