INTRODUCTION
The major endoscopic devices utilized to provide hemostasis and to close mucosal or luminal gastrointestinal (GI) defects are hemoclips and loops[1-3]. However, hemoclips may not allow for closure of large defects and they do not exert enough tensile force to keep fibrotic defects larger than 5 mm approximated[3]. In addition, partial and full-thickness defects resulting from perforations, fistulas and leaks may have irregular, thick and friable edges limiting the deployment of hemoclips and/or loops[4]. Recently, a new endoscopic closure device called the over-the-scope-clip (OTSC)-system (Ovesco Endoscopy, Tübingen, Germany) or “bear claw” became available[5,6]. The OTSC-system is an endoscopic clipping device made of Nitinol, which allows for treatment of peptic ulcer bleeding and the closure of perforations, anastomotic leaks and fistulas[7-9]. The majority of information on the OTSC device stems from animal studies but data on the usefulness of the OTSC device in humans is increasingly recognized[7-12]. The aim of this case report is to describe the effective endoscopic closure of a large gastrocolic fistula in an extremely malnourished patient with complex post-surgical upper GI anatomy.
CASE REPORT
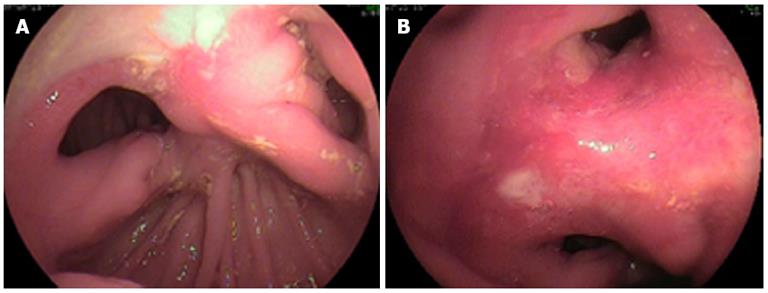
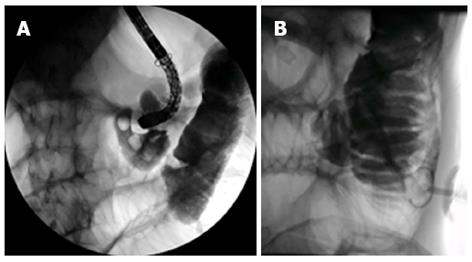
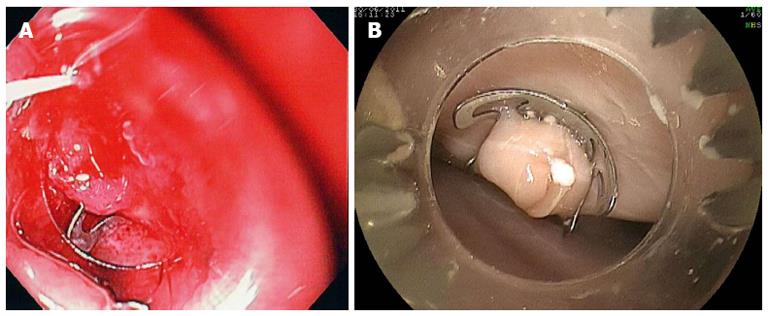
A 47-year-old man with history of chronic pancreatitis, alcoholism and Billroth II gastrojejunostomy for perforated peptic ulcer presented with chronic diarrhea and severe weight loss of 32-kg over a 1 year-period. The diarrhea was watery and occurred up to 12 times per day, being worse after eating. His physical examination was remarkable for cachexia, his weight was 40 kg, his height was 170 cm (body mass index = 12.8). The laboratory data were remarkable for hypoalbuminemia (1.8 g/dL) and decreased hemoglobin (11 g/dL). An esophagogastroduodenoscopy (EGD) showed a clean based ulceration at the anastomosis and patent lumen to both the afferent and efferent limbs (Figure 1A). At the upper part of the anastomosis there was an additional orifice, which represented the fistula (Figure 1B). Insertion of the scope through this orifice lead to the colon. The patient was placed on bowel rest, NPO, total parenteral nutrition. Due to the patient’s poor medical status no surgical intervention could be attempted to close the defect. The patient underwent a full GI evaluation (pananedoscopy) to exclude a malignancy or inflammatory bowel diseases leading to fistula formation. An upper GI series using barium clearly demonstrated a communication between the stomach and the colon. A colonoscopy revealed a normal colon mucosa, but no clear fistula opening could be detected. Repeat EGD disclosed the three openings at the gastrojejunal (Billroth II) anastomosis. Both the afferent and efferent limbs were patent and had normal mucosa. The gastrocolic fistula measured about 10-12 mm in diameter (Figure 1B). The EGD was exchanged for a double balloon enteroscope. The overtube was positioned inside the stomach and the enteroscope was advanced through the fistula into the colon (Figure 2). Both the rectum and the cecum were reached. After re-examining the colon and ruling out malignancy and inflammation, the scope was brought back to the gastrojejunal anastomosis and both limbs were investigated using the double-balloon enteroscopy technique. The small bowel mucosa was normal, without evidence of obstruction, fistulization or inflammation. A direct percutaneous enteroscopic feeding jejunostomy was then placed using the double-balloon enteroscopy (DBE)-technique[13]. Multiple biopsies of the gastrocolic fistula were negative for malignancy. Serum gastrin level was also within reference range.
Figure 1 Billroth II anatomy.
A clean-based ulcer is present at the anastomosis (A), the lumen to both the afferent and efferent limbs is patent (A); the gastrocolic fistula opening was located at the upper end of the anastomosis (B).
Figure 2 Insertion of the scope through this orifice lead to the colon (A), after placing the jejunostomy, water soluble contrast was injected confirming its perfect intra-jejunal position (B).
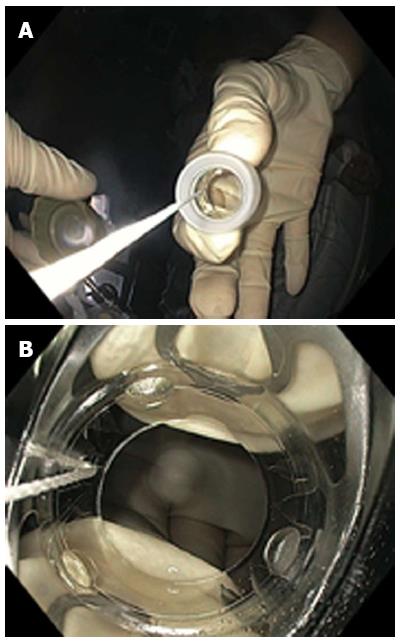
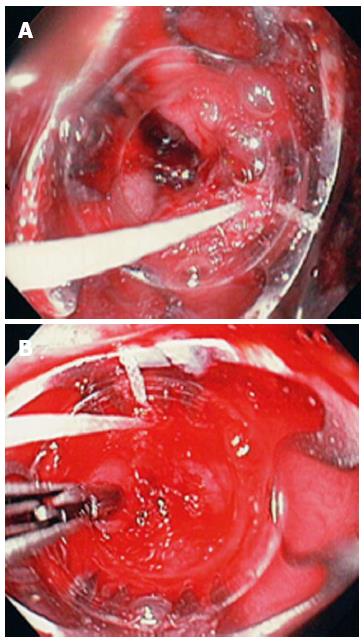
Closure of the gastrocolic fistula
Before closing the fistula the entrance into the orifice was marked with India ink (SPOT INK, ultrasound Enodscopy, United States) (Figure 3). This intervention was performed in order to mark the area of interest, as the fistulous tract was somewhat friable and the occurrence of edema and oozing could potentially obscure visualization of the area once the OTSC-system was loaded on the tip of the endosocpe. The gastrojejunostomy with the presence of two small bowel limbs made the endosocpic operation more challenging, as there is a previous report of complete small bowel obstruction resulting form the misapplication of this closure device[10]. The atraumatic 11 mm diameter OTSC-system (“bear claw”) was applied (Figure 4). The OTSC cap was approximated into the fistula and suctioned was applied (Figure 5). To achieve definite closure, the edges of the fistula were approximated with a twin grasper (OTSC Twin Grasper; Ovesco Endoscopy AG, Tubingen, Germany) (Figure 5). In addition, an ongoing effort was made to aspirate (i.e., “suck”) tissue into the distal transparent cap. Once enough tissue was trapped, the OTSC was released (Figures 6 and 7). The patient was continued on high dose proton pump inhibitors (esomeprazole 40 mg po bid), kept NPO and 24 h later the feedings were started through the DPEJ. On the third post-operative day an upper GI study using barium was performed, documenting complete closure of the gastrocolic fistula (Figure 8). Closure was also confirmed by performing an EGD with direct visual inspection and Indigo carmine dye instillation during a simultaneously performed colonoscopy. No dye escaped into the colon from the stomach during the procedure. On day four after endoscopic closure the patient was started on a liquid diet, which was then slowly advanced to soft. Due to his poor nutritional status it was elected to keep the jejunostomy tube feedings until he has regained more weight and his condition has markedly improved. The patient was discharged home in stable condition 7 d after initial presentation and remains well one month after the procedure.
Figure 3 Before closing the fistula the entrance into the orifice was marked with India ink.
Figure 4 T the over-the-scope-clip -system come loaded onto a transparent cap which is attached to the tip of the scope.
Figure 5 The over-the-scope-clip-system was approximated to the fistula (A) and the proximal edge of the fistula was pulled inside the transparent cap of the over-the-scope-clip-system using the Twin Grasper (B).
Figure 6 Once enough tissue was present inside the cap the over-the-scope-clip device was released.
(A) Example of deployed over-the-scope-clip -system in experimental perforation in an ex-vivo pig stomach (B).
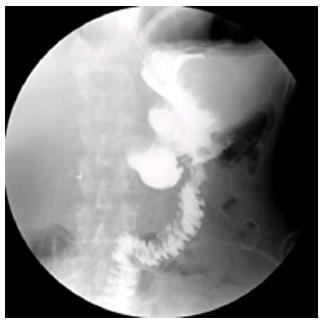
Figure 7 Radiologic view of the over-the-scope-clip -system (‘‘bear trap”).
Figure 8 Barium study documents complete closure of the fistula.
The contrast flows into the jejunal limbs.
DISCUSSION
To the best of our knowledge this is the first case of successful endoscopic closure of a gastrocolic fistula in a patient with complex post-surgical upper GI anatomy. The additional challenge in this patient was his poor clinical status and hence inability to benefit from a surgical intervention. The case stands out for several reasons. First we show that this tissue-suturing device is also useful to accomplish endoscopic closure of a complex fistula, located in an awkward anatomic position. We also provide useful tips and information on the utilization of this device, which is becoming more widely available. The OTSC-system is a quite innovative endoscopic suturing device made of superelastic biocompatible Nitinol, which allows for the entrapment of larger amount of tissue, allowing closure of fistula holes, and, as shown in these cases, hemostasis[7-12]. The ability to grasp and pull and/or “suck” a relative large volume of tissue into the distal transparent cap allows for potential closure of defects ranging from 10 to 20 mm in size, a situation which is usually not possible using traditional clipping devices[7-12]. Second, we also demonstrate how panendoscopic evaluation using EGD, colonoscopy and DBE was fundamental to thoroughly examine the GI tract for malignancy and inflammatory conditions. Whereas a capsule endoscopy may have also been helpful to evaluate the small bowel, its utility in patients with deranged upper GI anatomy is questionable as there is no guarantee that both limbs are examined. In addition, DBE allowed us to inspect the colon through the fistula located in the transverse colon and perform a right and left colon inspection, including the ileocecal valve. Furthermore, DBE permitted for a direct placement of a jejunal feeding tube, which was essential to aid in the enteral feeding of this severely malnourished patient. Third, this case adds to the growing evidence that the OTSC-system is a useful device to treat clinically significant endoluminal GI defects. These GI scenarios include leaks, GI bleeding, stent anchoring, fistula closure and resection of submucosal lesions[7-12].
The potential imitations of the OTSC-system should be acknowledged. Its application in tubular or torqued parts of the luminal GI tract may be difficult or impossible. In areas of curves or partially closed lumen, adequate apposition of the OTSC system against the defect may be impossible. If the defect is located in a tubular structure such as the esophagus adequate apposition of the device in a tangential manner to the defect may be more difficult. Thus, the closing forces of the OTSC-system may grasp and engulf the wrong part of the defect or normal tissue, as the vectorial forces are deranged due the angulated position of the device against the defect. Indeed, a crucial element to technical success of OTSC system placement is to accurately position the lesion within the transparent OTSC cap[10]. The misapplication of a clip to one side of such a lesion may interfere with the successful deployment of a second clip over the defect. Nonetheless, multiple OTSC applications in a single session may still be useful and allow approximation of tissue to facilitate subsequent closure[10]. Nevertheless, and as shown in our case and experience, if the defect is visible and reachable a successful application can always be successfully accomplished[11,12]. Using marking with chromoendoscopy may improve visualization and recognition of the defect while the OTSC-system is being applied. Because the device is new it is not known how long it remains attached after deployment. A potential complication of the OTSC system is that once it is deployed it cannot be removed. We have recently demonstrated two techniques to remove the “bear claw” using the wire technique[14] or resecting the OTSC system using endoscopic mucosal resection techniques[15]. In addition, the OTSC system can be removed using Nd-YAG Laser or argon plasma coagulation[10,16].
In summary, we have presented a case of successful endoscopic closure of a gastrocolic fistula in a severely malnourished patient with complex post-surgical upper GI anatomy. Panendoscopy using EGD, colonoscopy and DBE allowed for detailed examination of the GI tract and direct DPEJ placement before endoscopic closure with the OTSC. We strongly believe that this device is a major breakthrough for the management of various types of discontinuity defects or fistulas of the GI tract. Thus, the OTSC system should be incorporated into the therapeutic armamentarium of the advanced endoscopist. In addition, we show the usefulness of placing a direct jejunostomy using the DBE technique during the same procedure. The concept of providing direct jejunal feedings while allowing for upper gastrointestinal bowel rest to promote the healing of the minimally invasive endoscopic operation is novel. Thus, our case is unique and exemplifies the utility of minimally invasive endoscopic endoluminal surgery.