Published online Apr 16, 2013. doi: 10.4253/wjge.v5.i4.186
Revised: December 22, 2012
Accepted: January 5, 2013
Published online: April 16, 2013
Processing time: 264 Days and 18 Hours
Foreign objects ingestion occur commonly in pediatric patients. The majority of ingested foreign bodies pass spontaneously the gastrointestinal tract and surgery is rarely required for extraction. Endoscopic removal of foreign bodies larger than 10 cm has not yet been described. We present the case of a 16 years old bulimic girl that swallowed a 12 cm long teaspoon in order to provoke vomiting. The teaspoon perforated the duodenum. However, it was removed during gastroscopy and the site of perforation was closed endoscopically. This particular case shows the importance of endoscopy for retrieval of large foreign bodies, and the possibility to endoscopically close a perforated duodenal wall.
- Citation: Boškoski I, Tringali A, Landi R, Familiari P, Contini ACI, Pintus C, Costamagna G. Endoscopic retrieval of a duodenal perforating teaspoon. World J Gastrointest Endosc 2013; 5(4): 186-188
- URL: https://www.wjgnet.com/1948-5190/full/v5/i4/186.htm
- DOI: https://dx.doi.org/10.4253/wjge.v5.i4.186
Foreign objects ingestion occur commonly in pediatric patients, psychiatric patients, and those suffering from bulimia or anorexia. Mostly 90% of the foreign bodies pass spontaneously the gastrointestinal tract, 10%-20% require endoscopic removal, and less than 1% require surgery[1].
Ingestion of long, sharp and rigid foreign bodies is associated with an increased risk of impaction, perforation and bleeding. Foreign bodies may also impact or perforate the bowel wall. Symptoms are variable and mostly related to the site of impaction or perforation of the bowel wall. Foreign bodies can also be found incidentally on X-rays done for other reasons.
Anatomical sites where foreign bodies impact most commonly are pylorus, duodenal C-loop and ileo-cecal valve. Foreign bodies longer than 10 cm mostly impact in the duodenal C-loop because this part is fixed in the retroperitoneum[2]. Endoscopic removal of these objects should be attempted in a way to avoid perforation and if this fails, surgery should be considered.
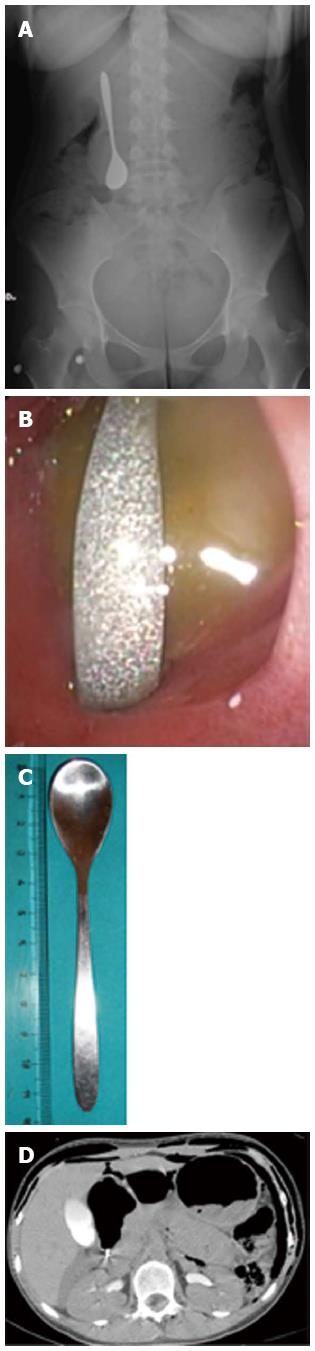
A 16-year-old bulimic girl swallowed a teaspoon in a way to induce vomiting. She informed the parents only 24 h later, when she had abdominal pain. On plain abdominal X-ray the teaspoon was in the right upper abdominal quadrant without evidence of intra-abdominal air (Figure 1A). On urgent upper endoscopy, there was a large amount of food in the stomach and in the duodenal bulb despite prolonged fasting. The tip of the teaspoon handle was found impacted into the duodenal mucosa at the level of the superior duodenal genu with suspected duodenal perforation (Figure 1B). With delicate maneuvers using a rat-tooth forceps the impacted teaspoon handle was removed from the duodenal wall, brought into the stomach and then extracted. The spoon was 12 cm long, 2 cm large at the cup and 0.5 cm at the handle, which was sharp (Figure 1C). Control endoscopy was performed immediately after extraction of the teaspoon, and this confirmed perforation of the duodenal wall. The mucosal flaps on the site of perforation were closed by placing 5 clips (EZ clips long, Olympus, Tokyo, Japan), and by injection of 3 mL of fibrin glue (Beriplast, Nycomed, Germany) over the clips in a way to consolidate the closure. Air injection during endoscopy induced the onset of subcutaneous emphysema, which was diagnosed on palpation. On urgent computed tomography (CT) scan there was diffuse bilateral retro-pneumoperitoneum extending to the right inguinal region, with a small amount of fluid into the retro-duodenal region near the right kidney (Figure 1D).
White blood cells count was 12.240 (normal value 4.100-9.800), without fever. On physical examination there was abdominal tenderness without signs of peritonitis. The patient started iv therapy with broad spectrum antibiotics and proton pump inhibitors. Clinical course was uneventful during the following days, and white blood cells count normalized without occurrence of fever. Four days later upper gastrointestinal enema with water soluble contrast confirmed the absence of leaks at the site of perforation. On control CT scan after 7 d diffuse retro-peritoneum was still present without evidence of fluid collections and upper endoscopy confirmed complete closure of the perforation. One week later the patient started oral nutrition and was discharged in good clinical conditions.
Swallowing of large objects (> 10 cm) may occur, but these usually do not pass spontaneously through the gastrointestinal tract, and often require urgent surgery due to perforation[2]. In the setting of intentional foreign body ingestion, the rate of endoscopic intervention may be much higher (63%-76%) and the need for surgical intervention ranges from 12% to 16%[3,4]. This however depends on the size of the foreign body (usually < 10 cm). Mortality rate in these patients is extremely low[5]. The technique of fibrin glue injection has already been described[6]. Our patient developed diffuse subcutaneous emphysema during endoscopy. The use of carbon dioxide instead of air should be preferred in these circumstances because of much more rapid reabsorption. Timing of endoscopy in these patients is very important, in order to reduce the risk of bacterial contamination in case of perforation[5].
This particular case shows the importance of endoscopy for retrieval of large foreign bodies, and the possibility to endoscopically close a perforated duodenal wall. The endoscopic approach was essential in this case and avoided surgery to this young patient.
| 1. | Arana A, Hauser B, Hachimi-Idrissi S, Vandenplas Y. Management of ingested foreign bodies in childhood and review of the literature. Eur J Pediatr. 2001;160:468-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 196] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 2. | Karcz WK, Kulemann B, Seifert GJ, Schrag HJ, Küsters S, Marjanovic G, Grüneberger JM, Braun A. Video. Laparoscopic extirpation of a fork from the duodenum. Surg Endosc. 2011;25:2363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Palta R, Sahota A, Bemarki A, Salama P, Simpson N, Laine L. Foreign-body ingestion: characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest Endosc. 2009;69:426-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 161] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 4. | Simic MA, Budakov BM. Fatal upper esophageal hemorrhage caused by a previously ingested chicken bone: case report. Am J Forensic Med Pathol. 1998;19:166-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Ikenberry SO, Jue TL, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T, Decker GA, Fanelli RD, Fisher LR, Fukami N. Management of ingested foreign bodies and food impactions. Gastrointest Endosc. 2011;73:1085-1091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 468] [Cited by in RCA: 540] [Article Influence: 36.0] [Reference Citation Analysis (1)] |
| 6. | Mutignani M, Iacopini F, Dokas S, Larghi A, Familiari P, Tringali A, Costamagna G. Successful endoscopic closure of a lateral duodenal perforation at ERCP with fibrin glue. Gastrointest Endosc. 2006;63:725-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
P- Reviewer Ciaccio EJ S- Editor Song XX L- Editor A E- Editor Zhang DN