Published online Sep 16, 2012. doi: 10.4253/wjge.v4.i9.432
Revised: September 3, 2011
Accepted: September 12, 2012
Published online: September 16, 2012
Covered self-expandable metal stents were developed to overcome tumor in-growth through the metal mesh. Stent migration is one of their malfunctions. Recently, the partially covered wallflex stent (PCWS) was developed with flared ends to prevent migration However, difficulty has been reported in its removal. We describe the removal of a PCWS embedded in mucosal hyperplasia at the uncovered proximal flared end, visualized by using SpyGlass cholangioscopy.
- Citation: Kawakubo K, Isayama H, Sasahira N, Kogure H, Miyabayashi K, Hirano K, Tada M, Koike K. Mucosal hyperplasia in an uncovered portion of partially covered metal stent. World J Gastrointest Endosc 2012; 4(9): 432-433
- URL: https://www.wjgnet.com/1948-5190/full/v4/i9/432.htm
- DOI: https://dx.doi.org/10.4253/wjge.v4.i9.432
A covered self-expandable metal stent (SEMS) was developed to overcome tumor-in growth through the metal mesh[1]. Stent migration is one of the malfunctions of covered SEMS[2]. Recently, the partially covered Wallflex stent (PCWS) (Boston Scientific, Natick, MA, United States) was developed with flared ends to prevent migration. However, this design had negative effect on stent removal[3]. We describe a patient in whom there was difficulty in removal of a PCWS embedded in mucosal hyperplasia at the uncovered proximal flared end, successfully visualized by using SpyGlass cholangioscopy (Boston Scientific, Natick, MA, United States).
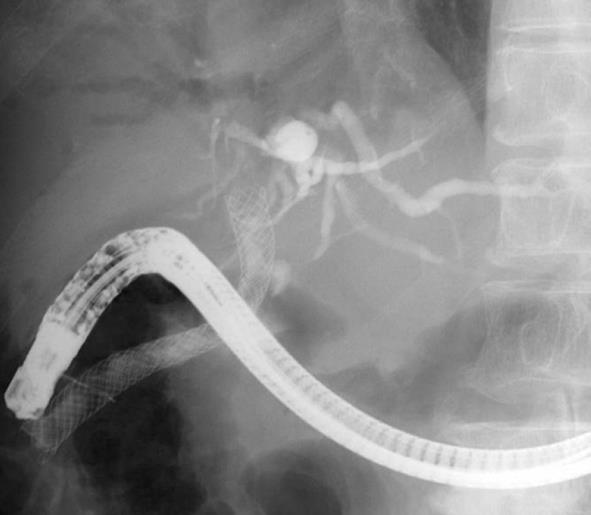
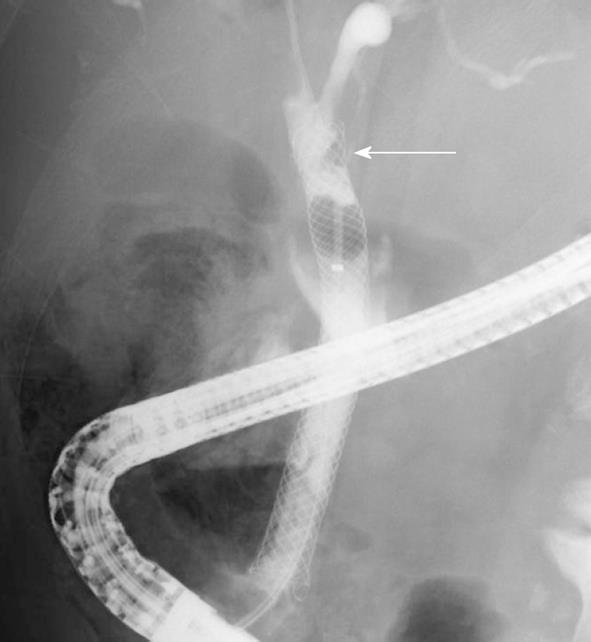
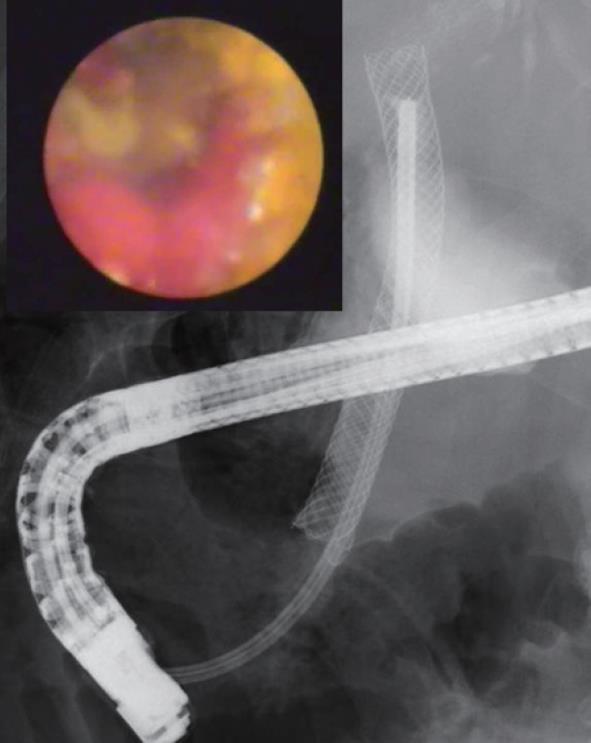
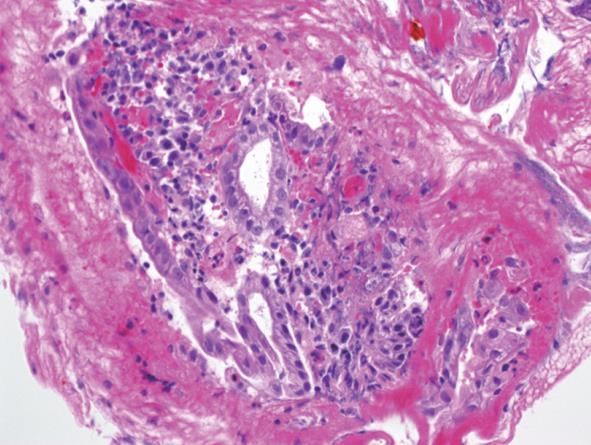
A 70-year-old man presented to our institution with fever and jaundice. Two years earlier, he received a PCWS for malignant biliary obstruction due to pancreatic head cancer and underwent systematic chemotherapy. Endoscopic retrograde cholangiopancreatography revealed a distally migrated PCWS and a biliary sludge inside the PCWS but no tumor in growth. Removal of the PCWS was attempted with a snare, but failed (Figure 1). After mechanical cleaning by a balloon catheter, cholangiography showed a filling defect at the proximal end of the PCWS (Figure 2). The SpyGlass direct visualization system revealed reddened mucosal hyperplasia in almost two thirds of the uncovered portion of the PCWS (Figure 3). The uncovered portion of the PCWS was totally embedded in the mucosal hyperplasia. Mucosal hyperplasia was not present at the covered portion of PCWS. We also performed biopsy of the mucosal hyperplasia under direct cholangioscopic visualization by using Spybite forceps (Boston Scientific, Natick, MA, United States) and confirmed the presence of inflammatory bile duct mucosa without malignancy (Figure 4). The cholangitis subsided with mechanical cleaning of biliary sludge inside the PCWS, and the patient was discharged on the second day after the procedure without further intervention.
In previous reports, covered a number of SEMS were safely and easily removed endoscopically using a snare or rat-tooth forceps[4,5]. A PCWS has uncovered flared ends to prevent migration, which ironically may cause tissue inflammation and mucosal hyperplasia at the proximal flared ends. In patients, the uncovered portion of the PCWS may become totally embedded into this mucosal hyperplasia, leading to difficulty in stent removal. A PCWS cannot always be removed endoscopically due to mucosal hyperplasia at the proximal flared end. In this case, the invagination method may be useful for the removal of an embedded PCWS[3], wherby the proximal end of PCWS is grasped, pulled off the bile duct and gradually invaginated by using a forceps.
| 1. | Isayama H, Komatsu Y, Tsujino T, Sasahira N, Hirano K, Toda N, Nakai Y, Yamamoto N, Tada M, Yoshida H. A prospective randomised study of "covered" versus "uncovered" diamond stents for the management of distal malignant biliary obstruction. Gut. 2004;53:729-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 460] [Cited by in RCA: 467] [Article Influence: 21.2] [Reference Citation Analysis (1)] |
| 2. | Wamsteker EJ, Elta GH. Migration of covered biliary self-expanding metallic stents in two patients with malignant biliary obstruction. Gastrointest Endosc. 2003;58:792-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Nakai Y, Isayama H, Kawakubo K, Kogure H, Sasaki T, Togawa O, Sasahira N, Hirano K, Tsujino T, Tada M. Endoscopic removal of a biliary covered metallic stent with the invagination method. Endoscopy. 2011;43 Suppl 2 UCTN:E30-E31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Shin HP, Kim MH, Jung SW, Kim JC, Choi EK, Han J, Lee SS, Seo DW, Lee SK. Endoscopic removal of biliary self-expandable metallic stents: a prospective study. Endoscopy. 2006;38:1250-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Kahaleh M, Tokar J, Conaway MR, Brock A, Le T, Adams RB, Yeaton P. Efficacy and complications of covered Wallstents in malignant distal biliary obstruction. Gastrointest Endosc. 2005;61:528-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 129] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
Peer reviewers: Mohammad Al-Haddad, Assistant Professor of Clinical Medicine, Director, MD, Endoscopic Ultrasound Fellowship Program, Indiana University School of Medicine, 550 N. University Blvd, Suite 4100, Indianapolis, IN 46202, United States; Vittorio Terruzzi, MD, Department of Gastroenterology, Ospedale Valduce, Via Dante, 11 22100 Como, Italy
S- Editor Song XX L- Editor Hughes D E- Editor Zheng XM