Published online Sep 16, 2012. doi: 10.4253/wjge.v4.i9.398
Revised: July 2, 2012
Accepted: September 12, 2012
Published online: September 16, 2012
AIM: To compare the rates of success and complications of two different methods of access into the common bile duct (CBD).
METHODS: Between October 2007 and November 2008, 173 consecutive patients (71 men, 102 women, mean age 68.6 years) requiring endoscopic retrograde cannulation of the papilla and endoscopic treatment were studied. In the first 88 patients CBD cannulation was performed through supra-papillary fistulotomy (group F); in the following 85 patients standard cannulation was performed through the Oddi sphincter (group S). Indications for the procedure were: choledocholithiasis, biliary obstruction, postoperative leak, sclerosing cholangitis, and Mirizzi’s syndrome.
RESULTS: Deep CBD cannulation was successful in 85/88 patients (96.5%) in group F vs 60/85 patients (70.6%) in group S (P < 0.0001). The remaining 25 group S patients in whom cannulation failed were shifted to fistulotomy. Fistulotomy was successful in 21/25 patients (84%). As for complications, hyperamilasemia occurred in 7 (7.9%) group F patients vs 7 (8.2%) group S patients (P = NS); mild pancreatitis in 1 (1.1%) group F patient vs 5 (5.8%) group S patients (P = NS); bleeding in 3 (3.4%) group F patients vs 3 (3.5%) group S patients (P = NS).
CONCLUSION: Needle-knife fistulotomy should represent either the first approach to therapeutic cannulation or rescue therapy after unsuccessful standard cannulation.
- Citation: Ayoubi M, Sansoè G, Leone N, Castellino F. Comparison between needle-knife fistulotomy and standard cannulation in ERCP. World J Gastrointest Endosc 2012; 4(9): 398-404
- URL: https://www.wjgnet.com/1948-5190/full/v4/i9/398.htm
- DOI: https://dx.doi.org/10.4253/wjge.v4.i9.398
Endoscopic retrograde cannulation of the papilla of Vater (ERCP) has become the procedure of choice for the treatment of pancreatic and biliary obstructive disorders. Transpapillary biliary cannulation is the preferred technique to enter the common bile duct (CBD), but access from the sphincter of Oddi to the biliary tract during ERCP is not always possible using standard cannulation techniques. The success rate for deep cannulation of the biliary tree during ERCP ranges between 80% and 95% in the hands of experienced endoscopists[1,2].
When standard cannulation is not possible, alternative techniques may be used: transpancreatic pre-cut, needle-knife pre-cut, needle-knife fistulotomy, and needle-knife pre-cut over pancreatic stent[3]. The rate of complications with these techniques varies widely, some authors report no increased risk while others find rates significantly increased. This discrepancy probably relates to the endoscopist’s level of expertise and the number of failed attempts at cannulation before attempting pre-cut. In experienced hands and in an appropriate clinical setting, pre-cut sphincterotomy appears to be an acceptable method of access into the bile duct[2,4-6].
The study aims to evaluate post-ERCP success and complication rates in two different patient groups: patients submitted to CBD cannulation directly through suprapapillary fistulotomy and patients submitted to the same manoeuvre after unsuccessful standard cannulation of CBD.
In our digestive endoscopy unit, we have been performing ERCPs for 20 years now, with roughly 420 procedures each year (performed by not more than two endoscopists). Where standard cannulation fails, we have usually tried an alternative technique such as needle-knife pre-cut, transpancreatic pre-cut, needle-knife fistulotomy, etc. However in recent years, we have focused on needle-knife fistulotomy as the alternative technique. Between October 2007 and November 2008, 173 consecutive patients (71 men, 102 women, mean age 68 years, range 32-97 years) required an operative ERCP (performed by one of two endoscopists). All patients provided informed written consent.
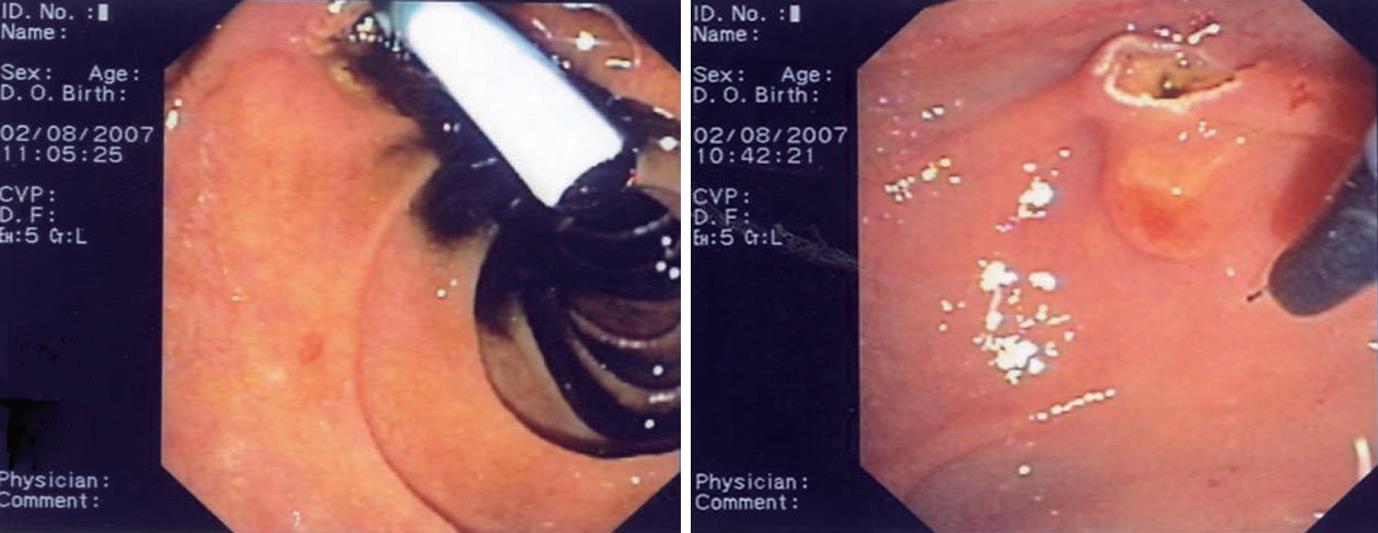
Patients with a previous history of failed ERCP, of acute or chronic pancreatitis, those requiring a pancreatogram, those with severe coagulopathy or previous gastric surgery with Roux-en-Y gastro-jejunostomy were excluded from this retrospective analysis. Patients with previous gastric resection according to the Billroth II technique were included in the study (Figure 1).
Out of the above group of patients, eighty-eight underwent CBD cannulation through supra-papillary fistulotomy with needle knife (group F); the other 85 patients received standard cannulation through the Oddi sphincter with a wire-guided sphincterotome (group S) (Table 1). The initial diagnosis was defined using clinical, laboratory, and radiologic data,; the final diagnosis comprised the categories: choledocholithiasis (113 patients), biliary obstruction (55 pts) postoperative leak (3 pts), sclerosing cholangitis (1 pt), and Mirizzi’s syndrome (1 pt). All the procedures were performed by a single endoscopist (MA) with experience of over 5000 ERCP’s.
| Group F | Group S | P value | |
| No. of patients | 88 | 85 | |
| Sex (male/female) | 48/40 | 47/38 | NS |
| Mean age (yr) | 68 (36–93) | 70 (32–96) | NS1 |
| Diagnosis | |||
| Choledocholithiasis | 58 | 59 | |
| Malignant stenosis | 20 | 17 | |
| Benign stenosis | 6 | 8 | |
| Postoperative leak | 2 | 1 | |
| Scleroses cholangitis | 1 | 0 | |
| Mirizzi’s syndrome | 1 | 0 |
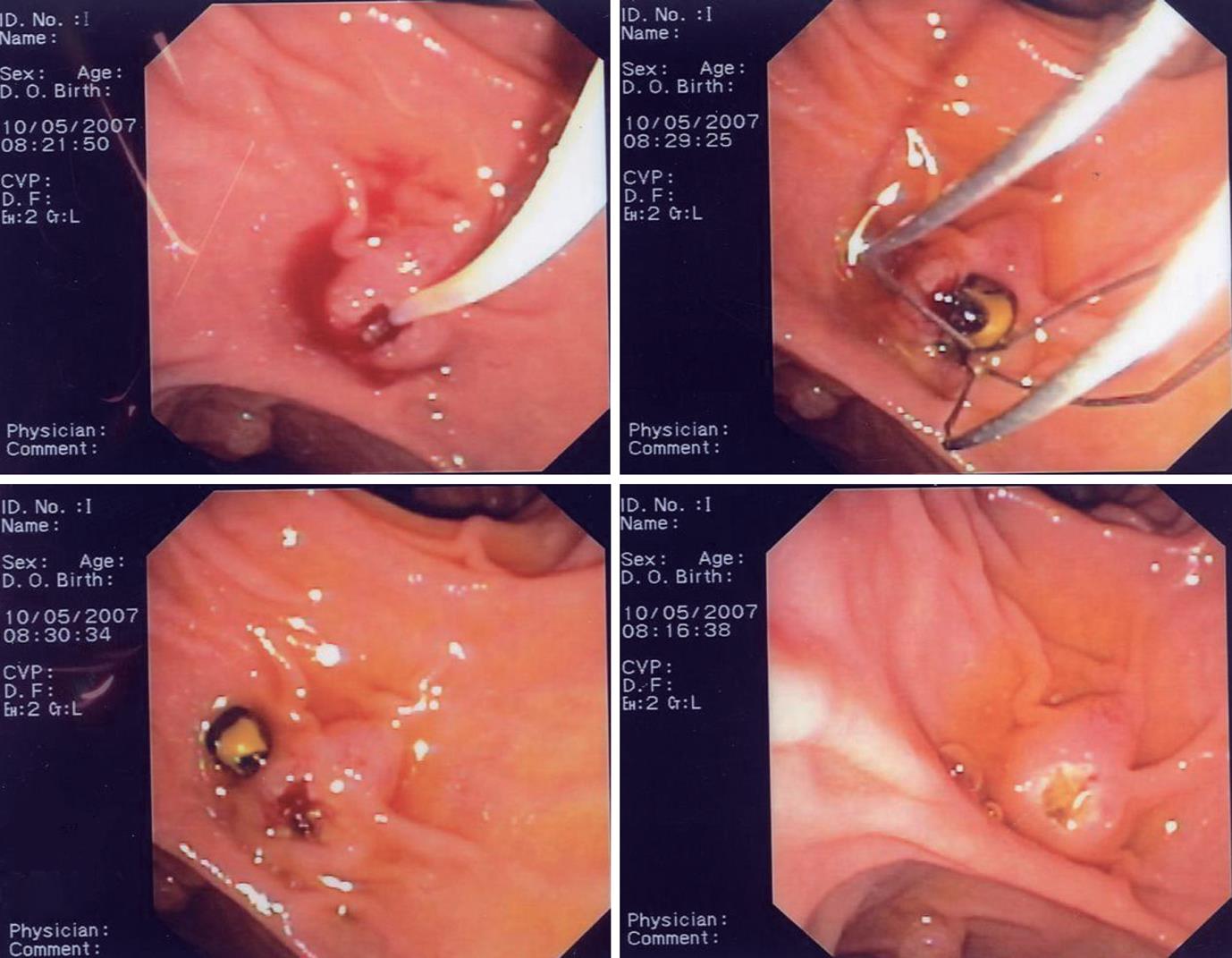
With the supra-papillary needle-knife fistulotomy technique (group F), a small incision was made by means of a 4 mm Huibregtse-Wilson Cook needle-knife or an Olympus modified sphincterotome a few millimeters above the papillary orifice to avoid injuring the pancreatic duct and to minimize the rate of post-ERCP pancreatitis, which is the most serious complication of such procedures.
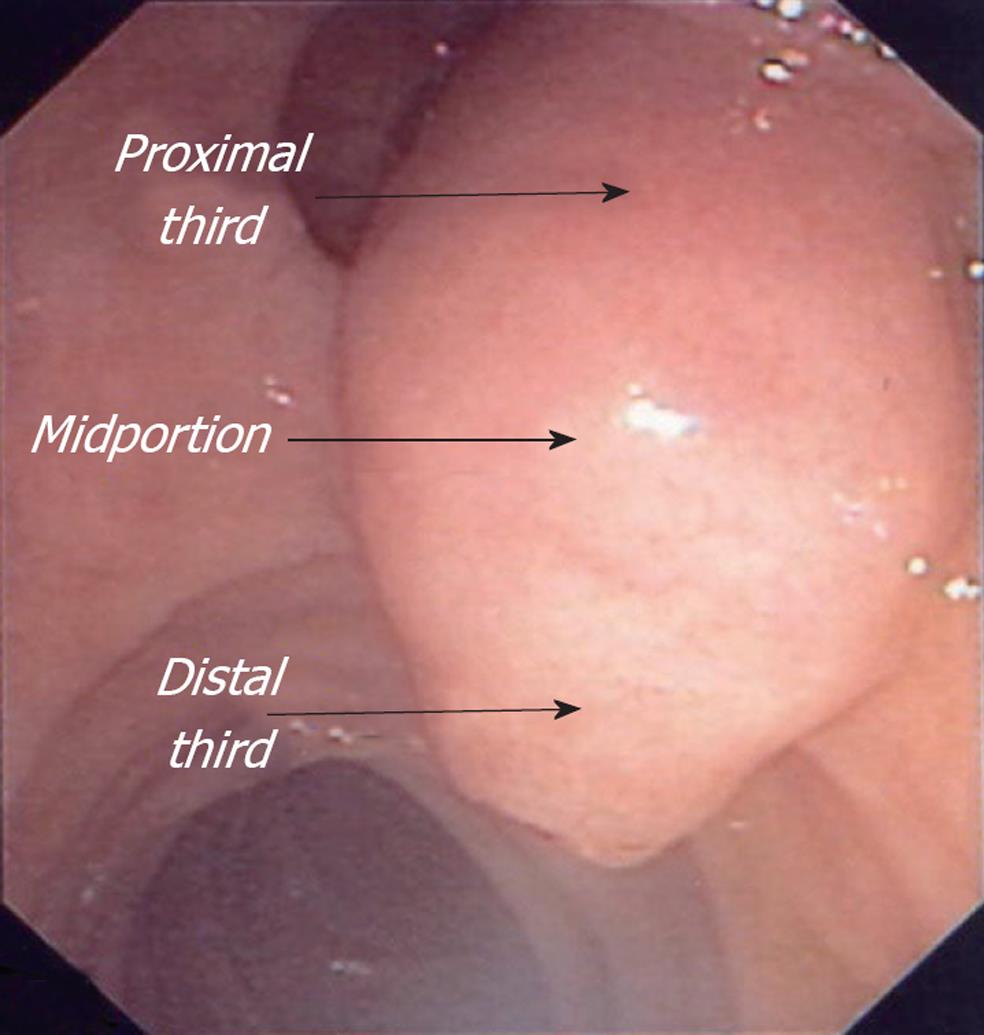
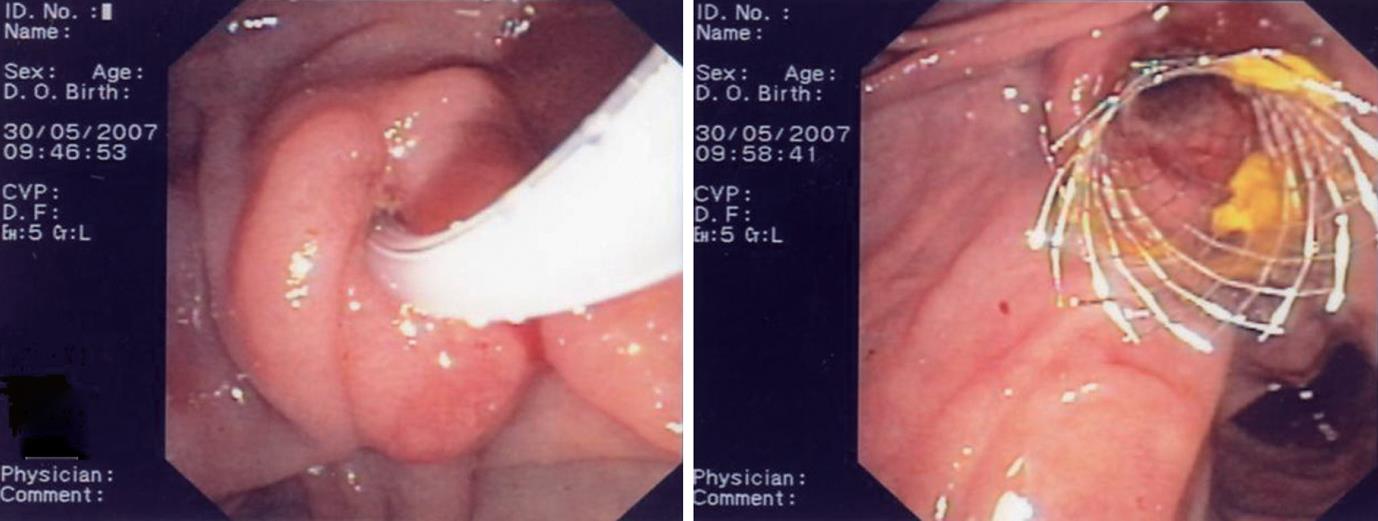
The starting point of the fistulotomy on the papilla (distal third, midportion or proximal third) and the length of the incision varied depending on the disorder being treated (bile duct stones, strictures, etc.) and on the size of the papilla (Figure 2).
For the insertion of a 10 Fr plastic stent just a small incision in the proximal third was required; however, removal of a large stone or the placement of a 10 mm metallic stent, needed the incision of the distal third or midportion (Figures 3 and 4).
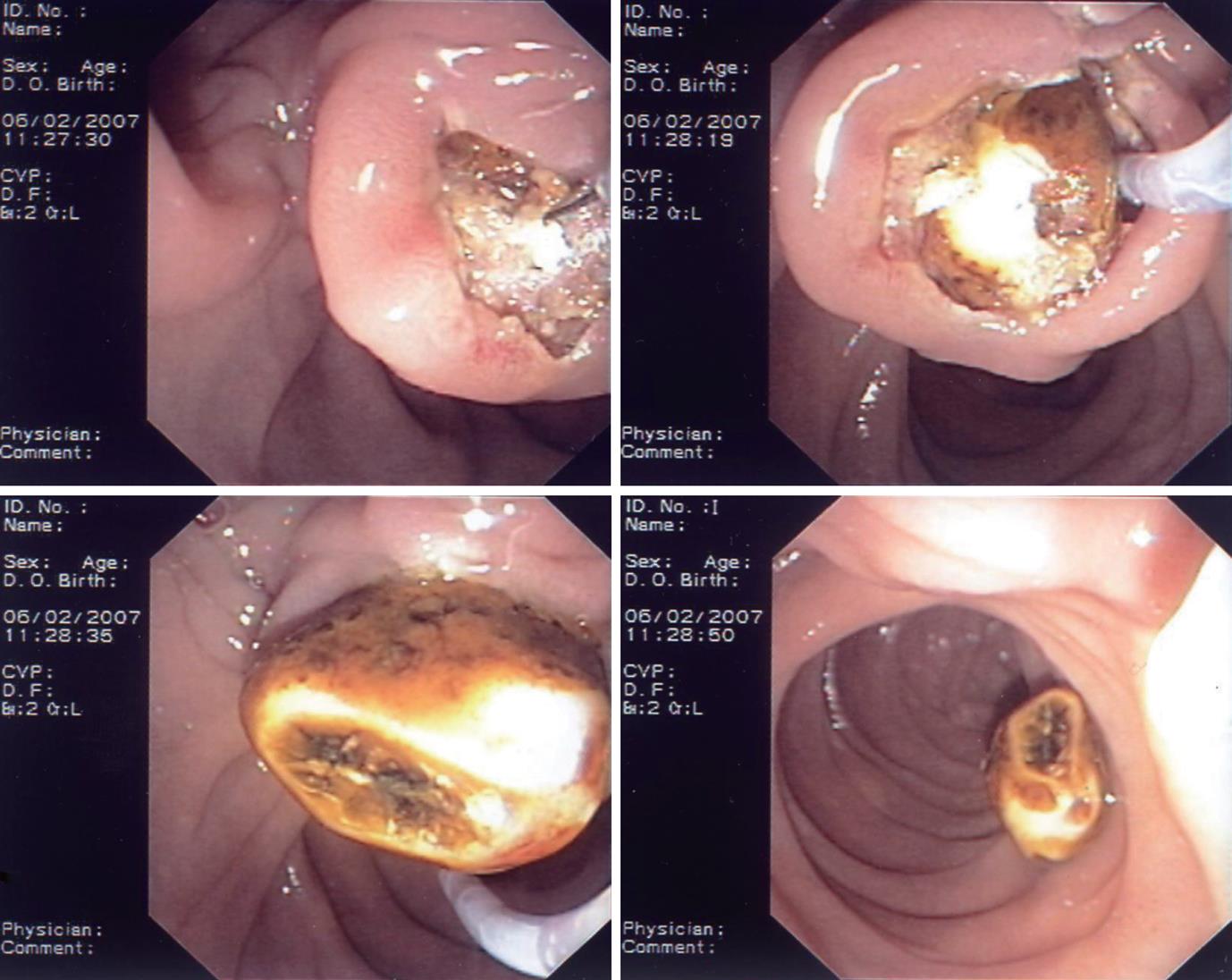
If cannulation of the CBD through this opening was not possible, one or two additional small but deeper incisions were performed. After fistulotomy, the CBD was cannulated through the incision with a wire-guided sphincterotome (Ultratome XL Microvasive with 0.89 mm straight Terumo). After deep cannulation, the correct position of the guidewire in the CBD was checked, dye was injected to obtain a cholangiogram, and finally, a complete papillotomy could be carried out (Figure 5). In these patients (group F) the sphincter of Oddi remained untouched.
In group S, selective cannulation of the CBD was attempted through the Oddi sphincter with a wire-guided sphincterotome (Ultratome XL Microvasive with 0.89 mm straight Terumo) using no more than 4 attempts, each one lasting less than 5 min. If the CBD cannulation was not achieved within 4 attempts, the patients were switched to the fistulotomy approach.
Patients remained hospitalized for at least 48 h after ERCP and their further course was followed by means of telephone interviews for a week to record any post-ERCP complications. Post-ERCP complications were defined according to consensus criteria[7]: (1) hyperamylasemia: any two-fold increase (or more) in serum amylase levels above the upper limit of normal but without abdominal symptoms; (2) mild pancreatitis: clinical symptoms (abdominal pain, nausea, and/or vomiting), serum amylase level increased at least three times the upper limit of normal for 24 h after ERCP, and illness requiring admission or prolongation of a planned admission to the hospital by 2 to 3 d; (3) moderate pancreatitis: as above but with duration of hospitalization between 4 and 10 d; (4) severe pancreatitis: acute pancreatitis needing more than 10 d hospitalization or haemorrhagic pancreatitis, pancreatic phlegmon, pancreatic pseudocyst, or requirement of surgical or radiologic interventional therapy; (5) retroperitoneal perforation: retroperitoneal air or leakage of contrast medium into the retroperitoneum during injection of contrast through a false track created by the sphincterotomy (or pre-cut or fistulotomia, etc.); (6) minor bleeding: bleeding controlled by endoscopic hemostasis, without changes in hemodynamics or fall in hemoglobin levels; and (7) major bleeding: occurrence of hematemesis, melena, decrease in hemoglobin levels to less than 80 g/L, and need for transfusion.
Statistical significance was evaluated according to χ2 test or Student t test for unpaired data, as stated following each table.
Complications (Table 2), as defined above, occurred in 11/88 (12.5%) of the patients in group F and in 15/85 (17.6%) of the patients in group S (P = NS). Hyperamilasemia occurred in 7 patients in each of the two groups, but these 14 patients needed no treatment since serum amylase levels returned to normal within 24 to 36 h after ERCP. Mild pancreatitis occurred in 1 (1.1%) group F patient vs 5 (5.8%) group S patients (P = NS); bleeding occurred in 3 (3.4%) group F patients vs 3 (3.5%) group S patients. Among the 6 cases of bleeding (5 patients with choledocholitiasis and 1 patient with malignant stenosis), 4 were classified as mild and 2 as major (one in each group). In both patients with major bleeding a repeat endoscopy was performed and followed by injection therapy with 1:10 000 epinephrine solution (5-10 mL). One of these patients needed no further treatment while the other (aged 92 years, belonging to group S) received no benefit from endoscopic treatment and underwent surgery. He died 3 d after the operation.
| Adverse effect | Group F 12/88 (13.6) | Group S 15/85 (17.6) | P value |
| Hyperamilasemia | 7 (7.9) | 7 (8.2) | NS |
| Mild pancreatitis | 1 (1.1) | 5 (5.8) | NS |
| Minor bleeding | 2 (2.27) | 2 (2.35) | NS |
| Major bleeding | 1 (1.13) | 1 (1.17) | NS |
| Death | 0 | 1 (1.17) | NS |
Patients in group F were finally diagnosed as being affected by choledocholithiasis (n = 55), malignant bile duct stenosis (n = 20), benign bile duct stenosis (n = 6), postoperative leak (n = 2), sclerosing cholangitis (n = 1), Mirizzi’s syndrome (n = 1). In group S, we documented choledocholithiasis (58 patients), malignant bile duct stenosis (n = 17), benign bile duct stenosis (n = 8), postoperative leak (n = 1). The 24 group S, patients who were shifted to fistulotomy had the following final diagnosis: choledocholithiasis (n = 15), malignant bile duct stenosis (n = 7), benign bile duct stenosis (n = 2).
Deep cannulation was successful at the first attempt in 85/88 pts (96.5%) in group F vs 60/85 pts (70.6%) in group S (P < 0.0001) (Table 3). The remaining 25 group S patients, in whom cannulation failed despite 4 attempts, were shifted to fistulotomy, which was successful in 21/25 pts (84%). The remaining 4 patients underwent a second ERCP 7 d after the first one. During the second ERCP successful cannulation through the incision of fistulotomy was achieved in 3 additional patients. So the overall success rate in the S group was 84/85 pts (98.8%).
| Group F | Group S | P value | |
| During the first ERCP | 85/88 (96.5%) | 60/85 (70.6%) (within 4 attempts of no more than 5 min) | < 0.0001 |
| Patients shifted to fistulotomy 21/24 (84%) | |||
| During the second ERCP after 7 d | 0 | 4 (4.7%) | |
| Overall success rate | 96.5% | 98.8% |
Stone extraction with Dormia basket was achieved in 52 of 55 (94.5%) group F patients and in 56 of 58 (96.5%) group S patients (P = NS). In 4 elderly patients with poor clinical conditions a 10 Fr plastic stent was placed to treat their large and multiple CBD stones. In 1 of 55 (1.8%) patients in the F group stone extraction was performed with a mechanical lithotriptor. Malignant bile duct stenosis was relieved with single 10 Fr plastic stents in 19 out of 20 (95%) patients in group F and in 17 out of 17 patients in the group S (P = NS). In one patient of F group a metallic stent was placed (Figure 6). All patients with a benign bile duct stenosis were treated with two 10 Fr plastic stents.
Endoscopists performing ERCP usually aim for the highest rate of successful CBD cannulation with the lowest rate of complications. Achieving deep cannulation of CBD remains a substantial challenge in ERCP for novices and experts alike. Transpapillary biliary cannulation is the preferred technique; however, 5%-15% of the most experienced endoscopists fail to cannulate the CBD. Pre-cutting (transpancreatic pre-cut, needle-knife pre-cut, needle-knife fistulotomy, and needle-knife pre-cut over pancreatic stent) is the most popular technique when standard cannulation fails. In the search for an alternative technique when standard cannulation fails, fistulotomy above the papillary orifice has been considered in some studies[1-3,8-10].
In our study, we demonstrated that the starting point of the fistulotomy on the papilla (distal third, midportion or proximal third) and the length of the incision varied depending on the disorder being treated (bile duct stones, strictures, etc.) and on the size of the papilla.
For the insertion of a 10 Fr plastic stent just a small incision in the proximal third was required. Conversely, removal of a large stone or placement of a 10 mm metallic stent, required incision of the distal third or midportion. If cannulation of the CBD through this opening was not possible, one or two additional small but deeper incisions were performed.
ERCP can be associated with serious complications including pancreatitis, bleeding, cholangitis, cholecystitis, and perforation. Of these complications, post-ERCP pancreatitis is the most frequent though often mild or moderate, although in about 10% of cases it is severe and potentially fatal.
Since the CBD and the duct of Wirsung share frequently a final common pathway, it is easy to injure the Wirsung duct during cannulation when multiple attempts are needed. Difficulty in CBD cannulation is one of the main factors increasing the risk of post-ERCP pancreatitis[5,11-13]. During ERCP the possible causes of pancreatitis are mechanical injury to the ampulla and pancreatic sphincter from repeated attempts to cannulate the bile duct, hydrostatic and chemical injury from multiple injections of contrast into the pancreatic duct, or thermal injury from endoscopic sphincterotomy[7,14,15]. Moreover, strong evidence indicates that multiple attempts at cannulation increase the risk of post-ERCP pancreatitis and no pharmacological prophylaxis has yet been reported to reduce significantly the incidence of post-ERCP pancreatitis[16,17].
One study[18] reported no cases of pancreatitis when the CBD was cannulated from the suprapapillary portion (i.e., at a defined distance from the Oddi sphincter). A randomized comparative study of “fistulotomy” above the orifice vs conventional needle knifing at the orifice found a significantly lower rate of pancreatits in the fistulotomy subset (0% vs 8%) of 153 patients with suspected choledocholithiasis[19].
In our study, group F showed only one case of mild pancreatitis; in group S there were only mild cases of pancreatitis (5.8% of patients). In group S, CBD cannulation was achieved within 4 attempts in 60/85 pts (70.5%), a figure that is comparable with previously reported data[8,20,21]. In agreement with current literature, in our study fistulotomy after failure of standard cannulation increased the overall success rate[6,17,22-24].
We conclude that in experienced hands, needle-knife fistulotomy is as safe as standard Oddi sphincter cannulation. Since it decreases the frequency of post-ERCP pancreatitis, it may be regarded both as an approach to therapeutic cannulation, and as a rescue procedure after unsuccessful cannulation of the sphincter of Oddi.
When pancreatic and biliary obstructive disorders are to be treated, access from the sphincter of Oddi to the biliary tract during endoscopic retrograde cannulation of the papilla (ERCP) is not always possible using standard cannulation techniques. Alternative techniques may be used. In appropriate clinical settings, precut sphincterotomy appears to be an acceptable method of access into the bile duct. Therefore, the authors evaluated post-ERCP success and complication rates in two different patients’ groups: patients submitted to common bile duct (CBD) cannulation directly through suprapapillary fistulotomy and patients submitted to the same manoeuvre after unsuccessful standard cannulation of CBD.
Transpancreatic pre-cut, needle-knife pre-cut, needle-knife fistulotomy, and needle-knife pre-cut over pancreatic stent are currently used to access CBD when the sphincter of Oddi cannot be cannulated.
The authors demonstrate that needle-knife fistulotomy is as safe as standard Oddi sphincter cannulation.
Since needle-knife fistulotomy also decreases the frequency of post-ERCP pancreatitis, it may be regarded both as an approach to therapeutic cannulation, and as a rescue procedure after unsuccessful cannulation of the sphincter of Oddi.
It is good work to be accepted with minor revision.
| 1. | Wojtun S, Gil J, Gietka W, Gil M. Endoscopic sphincterotomy for choledocholithiasis: a prospective single-center study on the short-term and long-term treatment results in 483 patients. Endoscopy. 1997;29:258-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Binmoeller KF, Seifert H, Gerke H, Seitz U, Portis M, Soehendra N. Papillary roof incision using the Erlangen-type pre-cut papillotome to achieve selective bile duct cannulation. Gastrointest Endosc. 1996;44:689-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 75] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Freeman ML, Guda NM. ERCP cannulation: a review of reported techniques. Gastrointest Endosc. 2005;61:112-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 232] [Article Influence: 11.0] [Reference Citation Analysis (1)] |
| 4. | Huibregtse K, Katon RM, Tytgat GN. Precut papillotomy via fine-needle knife papillotome: a safe and effective technique. Gastrointest Endosc. 1986;32:403-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 127] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1716] [Cited by in RCA: 1703] [Article Influence: 56.8] [Reference Citation Analysis (2)] |
| 6. | Akashi R, Kiyozumi T, Jinnouchi K, Yoshida M, Adachi Y, Sagara K. Pancreatic sphincter precutting to gain selective access to the common bile duct: a series of 172 patients. Endoscopy. 2004;36:405-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 33] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1890] [Cited by in RCA: 2086] [Article Influence: 59.6] [Reference Citation Analysis (2)] |
| 8. | Rabenstein T, Ruppert T, Schneider HT, Hahn EG, Ell C. Benefits and risks of needle-knife papillotomy. Gastrointest Endosc. 1997;46:207-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Baillie J. Needle-knife papillotomy revisited. Gastrointest Endosc. 1997;46:282-284. [PubMed] |
| 10. | Dumonceau JM, Rigaux J, Kahaleh M, Gomez CM, Vandermeeren A, Devière J. Prophylaxis of post-ERCP pancreatitis: a practice survey. Gastrointest Endosc. 2010;71:934-99, 934-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 71] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 11. | Williams EJ, Taylor S, Fairclough P, Hamlyn A, Logan RF, Martin D, Riley SA, Veitch P, Wilkinson ML, Williamson PR. Risk factors for complication following ERCP; results of a large-scale, prospective multicenter study. Endoscopy. 2007;39:793-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 279] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 12. | Bailey AA, Bourke MJ, Williams SJ, Walsh PR, Murray MA, Lee EY, Kwan V, Lynch PM. A prospective randomized trial of cannulation technique in ERCP: effects on technical success and post-ERCP pancreatitis. Endoscopy. 2008;40:296-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 166] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 13. | Dumonceau JM, Andriulli A, Deviere J, Mariani A, Rigaux J, Baron TH, Testoni PA. European Society of Gastrointestinal Endoscopy (ESGE) Guideline: prophylaxis of post-ERCP pancreatitis. Endoscopy. 2010;42:503-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 184] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 14. | Freeman ML, DiSario JA, Nelson DB, Fennerty MB, Lee JG, Bjorkman DJ, Overby CS, Aas J, Ryan ME, Bochna GS. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001;54:425-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 801] [Cited by in RCA: 852] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 15. | Varadarajulu S, Kilgore ML, Wilcox CM, Eloubeidi MA. Relationship among hospital ERCP volume, length of stay, and technical outcomes. Gastrointest Endosc. 2006;64:338-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 120] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 16. | Freeman ML, Guda NM. Prevention of post-ERCP pancreatitis: a comprehensive review. Gastrointest Endosc. 2004;59:845-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 321] [Cited by in RCA: 318] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 17. | Testoni PA. Facts and fiction in the pharmacologic prevention of post-ERCP pancreatitis: a never-ending story. Gastrointest Endosc. 2006;64:732-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Artifon EL, Sakai P, Ishioka S, Hondo FY, Raju GS. Suprapapillary puncture of the common bile duct for selective biliary access: a novel technique (with videos). Gastrointest Endosc. 2007;65:124-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Mavrogiannis C, Liatsos C, Romanos A, Petoumenos C, Nakos A, Karvountzis G. Needle-knife fistulotomy versus needle-knife precut papillotomy for the treatment of common bile duct stones. Gastrointest Endosc. 1999;50:334-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 110] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 20. | Kasmin FE, Cohen D, Batra S, Cohen SA, Siegel JH. Needle-knife sphincterotomy in a tertiary referral center: efficacy and complications. Gastrointest Endosc. 1996;44:48-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 85] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Bruins Slot W, Schoeman MN, Disario JA, Wolters F, Tytgat GN, Huibregtse K. Needle-knife sphincterotomy as a precut procedure: a retrospective evaluation of efficacy and complications. Endoscopy. 1996;28:334-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 74] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 22. | Freeman ML, Overby C, Qi D. Pancreatic stent insertion: consequences of failure and results of a modified technique to maximize success. Gastrointest Endosc. 2004;59:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 137] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 23. | O'Connor HJ, Bhutta AS, Redmond PL, Carruthers DA. Suprapapillary fistulosphincterotomy at ERCP: a prospective study. Endoscopy. 1997;29:266-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Abu-Hamda EM, Baron TH, Simmons DT, Petersen BT. A retrospective comparison of outcomes using three different precut needle knife techniques for biliary cannulation. J Clin Gastroenterol. 2005;39:717-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 45] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
Peer reviewer: Paola De Angelis, MD, Digestive Surgery and Endoscopy Unit, Pediatric Hospital Bambino Gesù, Piazza S. Onofrio, 400165 Rome, Italy
S- Editor Song XX L- Editor Hughes D E- Editor Zheng XM