Published online Feb 16, 2026. doi: 10.4253/wjge.v18.i2.116518
Revised: December 3, 2025
Accepted: January 6, 2026
Published online: February 16, 2026
Processing time: 82 Days and 14.3 Hours
Endoscopic retrograde cholangiopancreatography remains the primary modality for biliary decompression in extrahepatic biliary obstruction (EHBO). There are scarce data on the rate of fall in bilirubin after endoscopic biliary drainage (EBD) in EHBO.
To evaluate the rate and determinants of serum bilirubin decline after EBD in patients with EHBO and their impact on patient outcomes.
This prospective observational study enrolled adults with EHBO and a serum total bilirubin level greater than 6 mg/dL who underwent endoscopic retrograde cholangiopancreatography from May 2023 to October 2024. Liver function tests were recorded at baseline and on days 1, 2, 7, and 15, and monthly thereafter. The primary outcome was the proportion of patients achieving a ≥ 50% decrease in bilirubin by day 7. Secondary outcomes included time to bilirubin < 3 mg/dL, predictors of biochemical response, need for reintervention, and 3-month mor
Among 101 patients, 60.4% had malignant EHBO. Overall, 80.2% achieved ≥ 50% bilirubin reduction by day 7, and 70.3% achieved bilirubin < 3 mg/dL by day 15. Benign etiology [adjusted odds ratio (aOR): 4.30; P = 0.038] and younger age (aOR: 0.95; P = 0.032) independently predicted an early response (day 7). Baseline bilirubin (aOR: 0.79; P < 0.001) and alkaline phosphatase levels (aOR: 1.002; P = 0.043) predicted bilirubin < 3 mg/dL by day 15. Reintervention was required in 15.8%, and 3-month mortality was 14.8%, predominantly in malignant EHBO. Failure to achieve > 50% reduction in bilirubin by day 7 was an independent predictor of reintervention, while failure to achieve bilirubin < 3 mg/dL by day 15 and acute kidney injury were independent predictors of mortality.
Failure to achieve ≥ 50% fall by day 7 predicts reintervention, while inability to reach bilirubin < 3 mg/dL by day 15 predicts mortality. Bilirubin kinetics following EBD serve as reliable indicators of drainage adequacy and short-term prognosis in EHBO.
Core Tip: Early bilirubin kinetics provide a simple, reliable, and clinically actionable tool after endoscopic biliary drainage for extrahepatic biliary obstruction. A ≥ 50% fall in bilirubin by day 7 indicates adequate drainage and predicts lower need for reintervention, whereas failure should prompt early reassessment for stent dysfunction or incomplete drainage. Achieving a bilirubin < 3 mg/dL by day 15 is a strong indicator of recovery, particularly in malignant obstruction; failure to do so predicts higher short-term mortality. Baseline bilirubin, alkaline phosphatase levels, etiology, and presence of acute kidney injury should guide the intensity of monitoring. Routine incorporation of bilirubin kinetics can improve post-endoscopic retrograde cholangiopancreatography decision-making and outcomes.
- Citation: Naidu KSC, Giri S, Sahu SK, Praharaj DL, Mallick B, Nath P, Das S, Panigrahi SC, Sahu MK, Anand AC, Chawla YK, Acharya SK. Reduction of serum bilirubin levels after endoscopic biliary drainage in patients with extrahepatic biliary obstruction and its significance. World J Gastrointest Endosc 2026; 18(2): 116518
- URL: https://www.wjgnet.com/1948-5190/full/v18/i2/116518.htm
- DOI: https://dx.doi.org/10.4253/wjge.v18.i2.116518
Extrahepatic biliary obstruction (EHBO) represents a common and clinically significant cause of cholestatic jaundice encountered in gastroenterology and hepatobiliary practice. The etiological spectrum of EHBO encompasses benign lesions such as choledocholithiasis, inflammatory or iatrogenic strictures, and malignant causes, including cholangiocarcinoma, pancreatic head carcinoma, and periampullary neoplasms[1-3]. In the Indian subcontinent, gallstone disease remains a predominant contributor, while late-presenting biliary and pancreatic malignancies account for an increasing proportion of cases in high-incidence geographic regions, such as the Gangetic plains and northeastern areas[2,3].
Timely diagnosis and effective biliary decompression are critical to prevent serious complications, including ascending cholangitis, sepsis, and secondary biliary cirrhosis. Endoscopic retrograde cholangiopancreatography (ERCP) is the most used modality for biliary decompression, as it enables both visualization and therapeutic intervention in a single pro
In malignant obstruction, for instance, the decline in bilirubin may be slower or incomplete, especially if biliary drainage is only partial or if hepatic infiltration or cirrhosis coexist[4]. In contrast, benign causes such as stone-related obstruction may exhibit a more rapid and consistent decline in bilirubin levels. Quantifying the rate of bilirubin decline post-ERCP provides valuable insights into procedural efficacy, the need for re-intervention, and the timing of subsequent oncologic or surgical management. This study systematically evaluates the rate and determinants of bilirubin decline following endoscopic biliary drainage (EBD) in EHBO. It examines its clinical relevance as a prognostic and quality-of-care indicator in contemporary endoscopic practice.
This is a prospective observational study conducted at a tertiary care center in Eastern India from May 2023 to October 2024. Consecutive patients having EHBO with jaundice and undergoing ERCP for biliary drainage were enrolled and managed according to standard guidelines. The study protocol was approved by the Institutional Research and Ethics Committee (approval No. KIIT/KIMS/IEC/1331/2023), and written informed consent was obtained from all participants before their participation.
Patients aged 18 years or older with EHBO and serum bilirubin levels greater than 6 mg/dL were eligible for the study. Exclusion criteria were patients who were not feasible for ERCP, associated liver disorder causing intrahepatic cho
Liver function tests were performed on the day of the procedure, followed by days 1, 2, 7, 15, 1 month, 2 months, and 3 months. Endpoint was the time taken to reach a total bilirubin level < 3 mg/dL or 3 months of follow-up, whichever comes first. If there is renal dysfunction at the time of admission, renal function tests were also sent along with liver function test on their respective days. The diagnosis and the severity of cholangitis were assessed using the Tokyo 2018 classification[7]. Acute kidney injury (AKI) was diagnosed according to Kidney Disease Improving Global Outcomes Clinical Practice Guideline for AKI 2012[8].
The primary outcome was the percentage of patients with EHBO and jaundice who underwent ERCP for biliary drainage and experienced a fall in total serum bilirubin level by the 7th day. The secondary outcome was the proportion of patients achieving a serum bilirubin < 3 mg/dL, to evaluate the factors that determine the rate of fall in total serum bilirubin levels, and to study the impact of a fall in serum bilirubin levels on reintervention and mortality.
Delta bilirubin levels were calculated by calculating absolute reductions (Δ values) from baseline to various time points and comparing subgroups (e.g., etiology, baseline bilirubin) using t-tests. Inferential statistics included independent samples t-tests for normally distributed variables, and Mann-Whitney U tests for non-parametric comparisons. χ2 and Fisher’s exact tests were used for associations between categorical variables. Temporal trends in biochemical markers were analyzed using repeated-measures analysis of variance. Multivariate analysis was performed using binary logistic regression to identify predictors of ≥ 50% bilirubin reduction by day 7 and 3-month mortality. The results were reported as adjusted odds ratios (aOR) with 95% confidence intervals (CIs). Time to event analysis was examined by the duration to achieve total bilirubin < 3 mg/dL, categorized into intervals (e.g., within 1 day, 2 days, 7 days, or 15 days) and compared using χ2 tests. P < 0.05 was considered statistically significant. Analyses were performed using Microsoft Excel 2019 and IBM SPSS v26.0.
In this study involving 101 patients with EHBO (Table 1), the median age of the patients was 56 years (range: 22-92), with a slight male predominance (54.5%). Malignant obstruction was more common, affecting 61 patients (60.4%), while benign obstruction was present in 40 patients (39.6%). Among patients with a malignant etiology, 45.9% (28/61) had a perihilar block, and 54.1% (33/61) had a distal block. Clinical cholangitis was present in approximately half of the study population (52/101, 51.5%), with rates of 57.5% (23/40) and 47.5% (29/61) in benign and malignant EHBO, respectively. Baseline total bilirubin levels in malignant and benign cases were 14.45 mg/dL and 11.77 mg/dL, respectively. Ten patients had baseline AKI. Ninety-four participants received plastic stents, while 7 participants received metallic stents. Complications occurred in 9 participants (8.9%); 4 had post-ERCP pancreatitis and 5 had minor bleeding.
| Parameters | Total (n = 101) | Benign (n = 40) | Malignant (n = 61) | P value |
| Age, years | 56 (22-92) | 50 (22-79) | 58 (26-92) | 0.008 |
| Male gender | 55 (54.5) | 23 (57.5) | 32 (52.5) | 0.618 |
| Comorbidities | 27 (26.7) | 12 (30) | 15 (24.6) | 0.548 |
| Diabetes mellitus | 15 (14.8) | 8 (20) | 7 (11.5) | |
| Hypertension | 2 (2.0) | 1 (2.5) | 1 (1.6) | |
| DM + hypertension | 5 (4.9) | 1 (2.5) | 4 (6.5) | |
| Others | 5 (4.9) | 2 (5) | 3 (4.9) | |
| Cholangitis | 52 (51.5) | 23 (57.5) | 29 (47.5) | 0.327 |
| Leucocyte count, × 103 per mm3 | 10.35 (4.69-44.0) | 10.23 (5.6-34.1) | 10.74 (4.69-44.0) | 0.843 |
| PT-INR | 1.2 (0.9-4.1) | 1.2 (1.0-3.2) | 1.3 (0.9-4.1) | 0.044 |
| Serum creatinine, mg/dL | 0.7 (0.4-5.7) | 0.8 (0.4-5.7) | 0.6 (0.4-2.9) | 0.069 |
| Total bilirubin level, mg/dL | 11.8 (6.0-30.2) | 9.9 (6.0-24.7) | 13.5 (6.1-30.2) | 0.008 |
| Alkaline phosphatase, IU/L | 368 (109-2000) | 360 (119-1500) | 372 (109-2000) | 0.034 |
| Plastic stent | 94 (93.1) | 40 (100) | 54 (88.5) | 0.040 |
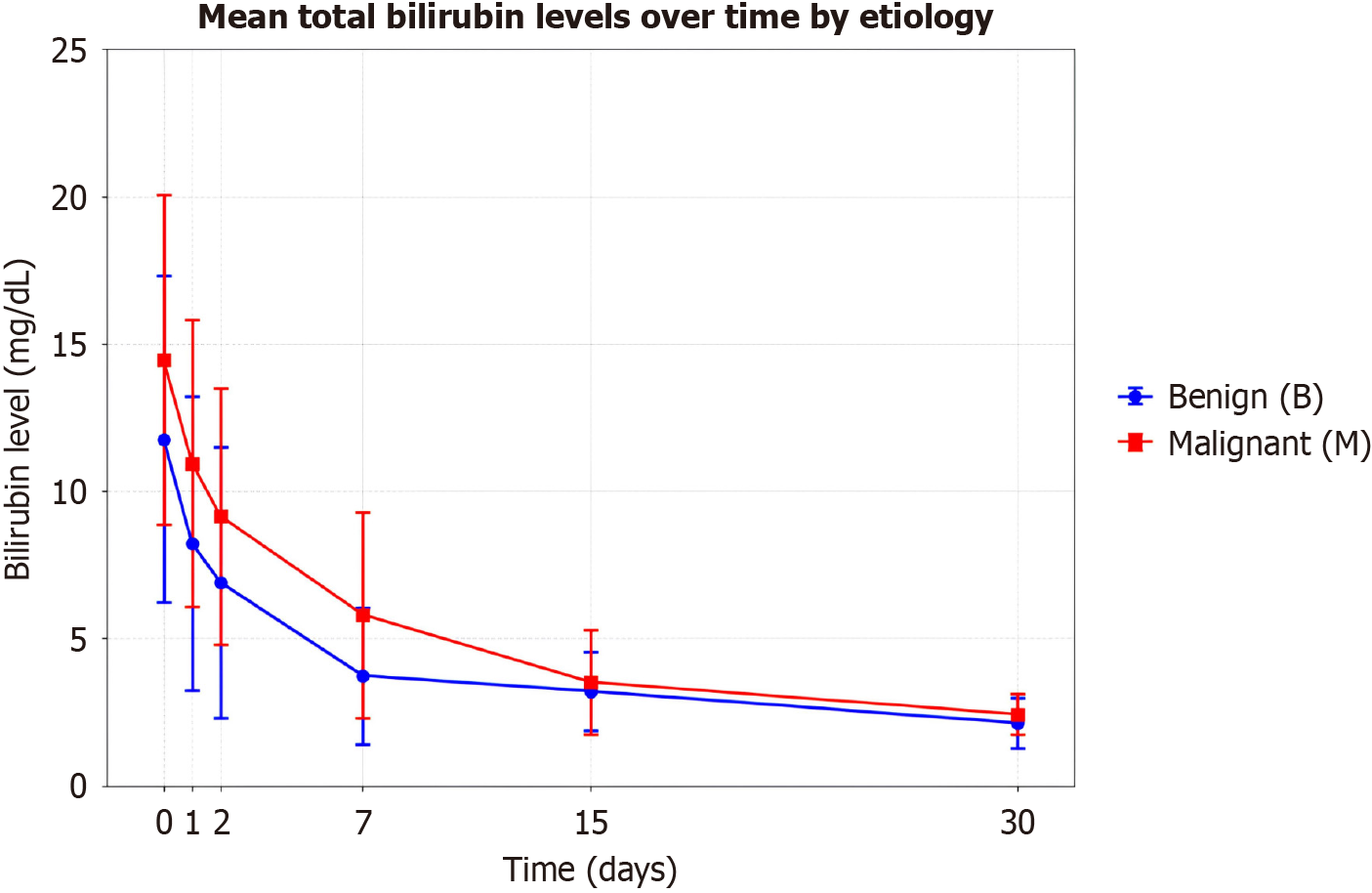
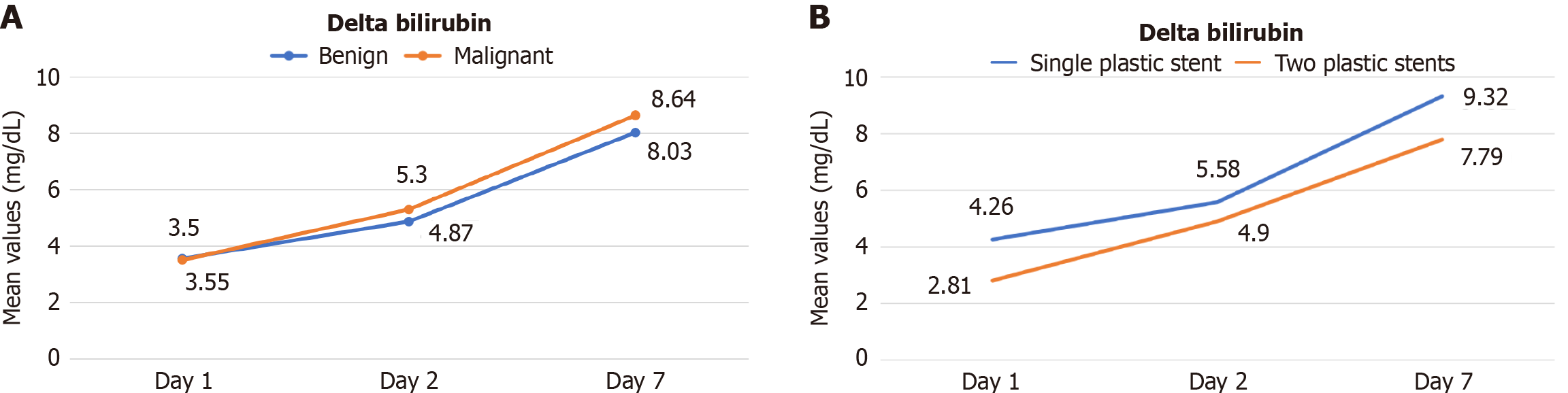
Figure 1 shows the fall in mean bilirubin levels over 30 days, comparing benign and malignant etiologies. A total of 81 out of 101 (80.2%) patients achieved a > 50% reduction in total bilirubin by day 7, and the majority had benign etiologies (37/40, 92.5% vs 44/61, 72.1%; P = 0.011) (Table 2). ΔBilirubin between the benign and malignant groups showed no statistically significant difference (Figure 2A). In malignant cases, there was no significant difference in delta bilirubin between the single and two plastic stent groups by day 7 (Δbilirubin7, 9.40 mg/dL vs 8.30 mg/dL, P = 0.162) (Figure 2B). The re-intervention group had a slightly lower Δbilirubin compared to the control group, but this difference was not statistically significant at day 7 (7.75 mg/dL vs 8.51 mg/dL, P = 0.967).
| Groups | Within 1 day | Within 2 days | Within 7 days | Within 15 days | Within 30 days | Total |
| Total | 1 (0.9) | 6 (5.9) | 36 (35.6) | 70 (69.3) | 86 (85.1) | 101 |
| Etiology of EHBO | ||||||
| Benign | 1 (2.5) | 6 (15.0)1 | 23 (57.5)1 | 33 (82.5)1 | 38 (95.0)1 | 40 |
| Malignant | 0 (0.0) | 0 (0.0) | 13 (21.3) | 37 (60.6) | 48 (78.7) | 61 |
| Bilirubin level | ||||||
| ≤ 10 mg/dL | 2 (5.6) | 9 (25.0)1 | 26 (72.2)1 | 33 (91.7)1 | 35 (97.2)1 | 36 |
| > 10 mg/dL | 0 (0.0) | 0 (0.0) | 10 (15.4) | 37 (56.9) | 52 (80.0) | 65 |
A total of 71 out of 101 (70.3%) patients achieved bilirubin levels < 3 mg/dL by day 15, and the majority had benign etiologies (33/40, 82.5% vs 37/61, 60.6%; P = 0.030) (Table 2). Based on the baseline bilirubin level, a higher proportion of patients with baseline bilirubin < 10 mg/dL achieved bilirubin levels < 3 mg/dL by day 15 (33/36, 91.7% vs 37/65, 56.9%; P ≤ 0.001) (Table 2).
Table 3 shows the multivariate analysis evaluating predictors of a greater than 50% reduction in total bilirubin by day 7 and achieving a total bilirubin level < 3 mg/dL by day 15. Among these, benign etiology of EHBO (aOR: 4.303, 95%CI: 1.085-17.059; P = 0.038) and younger age (aOR: 0.95, 95%CI: 0.91-0.99; P = 0.032) were identified as independent pre
| Variables | > 50% in bilirubin by day 7 | Bilirubin < 3 mg/dL by day 15 | ||
| Odds ratio (95%CI) | P value | Odds ratio (95%CI) | P value | |
| Age | 0.952 (0.910-0.995) | 0.03 | 0.989 (0.939-1.043) | 0.689 |
| Female gender | 0.723 (0.236-2.215) | 0.571 | 0.622 (0.145-2.664) | 0.522 |
| No cholangitis at baseline | 0.639 (0.210-2.029) | 0.447 | 4.944 (0.857-28.524) | 0.074 |
| Benign etiology | 4.303 (1.085-17.059) | 0.038 | 1.226 (0.239-6.303) | 0.807 |
| Baseline total bilirubin | 0.935 (0.849-1.030) | 0.175 | 0.79 (0.72-0.89) | < 0.001 |
| ALP | 1.002 (1.000-1.004) | 0.066 | 1.002 (1.000-1.003) | 0.043 |
During the 3-month follow-up period, 16 patients (15.8%) required reintervention. We conducted multivariate analysis using two parameters of bilirubin reduction separately (Table 4). Failure to achieve > 50% reduction in bilirubin by day 7 was an independent predictor of reintervention but not failure to achieve bilirubin < 3 mg/dL by day 15. On subgroup analysis of malignant etiology only, similar findings were observed.
| Variables | Model 1 (> 50% in bilirubin by day 7) | Model 2 (bilirubin < 3 mg/dL by day 15) | ||
| Odds ratio (95%CI) | P value | Odds ratio (95%CI) | P value | |
| All patients | ||||
| Benign etiology | 0.235 (0.024-2.348) | 0.218 | 0.200 (0.021-1.880) | 0.159 |
| No cholangitis at baseline | 4.528 (0.966-21.235) | 0.055 | 5.258 (1.091-25.348) | 0.039 |
| Baseline bilirubin < 10 mg/dL | 1.467 (0.286-7.513) | 0.646 | 2.512 (0.422-14.955) | 0.312 |
| Failure to achieve > 50% in bilirubin by day 7 | 4.751 (1.035-21.086) | 0.045 | - | - |
| Failure to achieve bilirubin < 3 mg/dL by day 15 | - | - | 4.411 (0.795-24.475) | 0.090 |
| Malignant etiology | ||||
| No cholangitis at baseline | 3.555 (0.689-18.333) | 0.130 | 4.039 (0.780-20.901) | 0.096 |
| Baseline bilirubin < 10 mg/dL | 1.085 (0.173-6.807) | 0.930 | 1.813 (0.262-12.554) | 0.547 |
| Failure to achieve > 50% in bilirubin by day 7 | 5.473 (1.089-27.498) | 0.039 | - | - |
| Failure to achieve bilirubin < 3 mg/dL by day 15 | - | - | 4.406 (0.776-25.030) | 0.094 |
Out of 101 patients, 15 patients expired within 3 months (14 were malignant, and one patient with choledocholithiasis expired because of complications secondary to laparoscopic cholecystectomy). Overall mortality was 14.8%, with striking differences between malignant and benign groups (23% vs 2.5%, P = 0.004). Multivariate analysis identified AKI and failure to achieve bilirubin < 3 mg/dL by day 15 as independent predictors of mortality, but not the inability to achieve > 50% reduction in bilirubin by day 7. On subgroup analysis of malignant etiology only, similar findings were observed (Table 5).
| Variables | Model 1 (> 50% in bilirubin by day 7) | Model 2 (Bilirubin < 3 mg/dL by day 15) | ||
| Odds ratio (95%CI) | P value | Odds ratio (95%CI) | P value | |
| All patients | ||||
| Age | 1.013 (0.967-1.062) | 0.582 | 1.011 (0.964-1.060) | 0.654 |
| Benign etiology | 0.116 (0.013-1.015) | 0.052 | 0.128 (0.014-1.127) | 0.064 |
| No AKI at baseline | 0.136 (0.031-0.601) | 0.009 | 0.194 (0.041-0.927) | 0.040 |
| Failure to achieve > 50% in bilirubin by day 7 | 2.075 (0.522-8.254) | 0.300 | - | - |
| Failure to achieve bilirubin < 3 mg/dL by day 15 | - | - | 5.396 (1.370-21.254) | 0.016 |
| Malignant etiology | ||||
| Age | 1.024 (0.971-1.079) | 0.385 | 1.017 (0.965-1.072) | 0.530 |
| No AKI at baseline | 0.103 (0.020-0.541) | 0.007 | 0.154 (0.027-0.886) | 0.036 |
| Failure to achieve > 50% in bilirubin by day 7 | 1.965 (0.457-8.455) | 0.364 | - | - |
| Failure to achieve bilirubin < 3 mg/dL by day 15 | - | - | 6.915 (1.496-31.963) | 0.013 |
This prospective single-center study evaluated the kinetics of bilirubin decline following EBD in patients with EHBO and explored its relevance for short-term clinical outcomes, need for re-intervention, and survival. The principal findings were: (1) Serum total bilirubin declined significantly and progressively over the first 7 days following drainage; (2) Benign etiologies exhibited faster biochemical recovery than malignant etiologies in absolute terms, but the relative fall in bilirubin (Δ-bilirubin) was comparable between groups; (3) Younger age and benign etiology independently predicted early (day 7) biochemical response, whereas baseline bilirubin and ALP predicted bilirubin normalization by day 15; and (4) Inability to achieve a 50% reduction in total bilirubin by day 7 was associated with higher odds of reintervention. These findings have both mechanistic and pragmatic implications for post-ERCP monitoring and clinical decision-making in jaundiced patients with EHBO.
The mean bilirubin decreased from 13.4 mg/dL pre-procedure to 4.9 mg/dL by day 7, representing an approximate 63% reduction. Weston et al[4] reported a similar temporal pattern in malignant obstruction, although normalization took up to 6 weeks when pre-stent bilirubin exceeded 10 mg/dL. Our findings are concordant with baseline bilirubin pre
Baseline bilirubin was significantly higher in malignant obstruction, reflecting the typically progressive, high-grade nature of malignant strictures involving the distal bile duct or hilum. Benign lesions such as choledocholithiasis or postoperative strictures are usually amenable to complete drainage in a single ERCP, resulting in faster biochemical recovery. Comparable patterns have been reported by Muckova et al[9], who found no significant difference in bilirubin fall between benign and malignant obstruction when normalized for baseline values. Our study corroborates that once drainage is achieved, the improvement in liver function is similar across etiologies, provided that adequate segments are decompressed. In malignancy, incomplete drainage of one or more hepatic segments or underlying parenchymal infiltration often limits bilirubin normalization. Studies on perihilar cholangiocarcinoma and unresectable hilar malignancy have reported that a ≥ 50% bilirubin reduction within 7-14 days correlates with adequate drainage and improved tolerance of subsequent therapy, even if bilirubin levels remain above 3 mg/dL[10,11]. Our findings reinforce the validity of this relative threshold as a practical early indicator of procedural success.
Multivariate analysis identified younger age and benign etiology as independent predictors of a rapid decline in bilirubin (≥ 50% by day 7). Younger patients generally have benign disease, better hepatic functional reserve, and fewer comorbidities, allowing faster recovery once cholestasis is relieved[12]. In benign disease, complete restoration of bile flow after stone extraction or stricture dilatation produces rapid clearance of conjugated bilirubin. In contrast, malignant strictures are frequently multifocal, associated with lobar exclusion or partial drainage, and complicated by cholangitis or sarcopenia, all of which can blunt biochemical improvement[13,14]. Baseline bilirubin and ALP were independently associated with achieving total bilirubin < 3 mg/dL by day 15. A higher degree of ALP elevation indicates a more severe degree of biliary obstruction, with a faster reduction in bilirubin after the establishment of drainage.
Failure to achieve a total bilirubin < 3 mg/dL by day 15 was strongly associated with adverse outcomes, particularly in malignant EHBO. This biochemical milestone is clinically relevant because persistent hyperbilirubinemia delays initiation of chemotherapy and predicts poor survival. Mikalsen et al[15] observed that patients achieving ≥ 50% bilirubin reduction within 30 days had significantly better survival, with mortality exceeding 30% in non-responders. Similarly, our data demonstrate that delayed bilirubin clearance identifies patients at high risk for early death, likely reflecting either inadequate drainage or advanced hepatic infiltration. In practice, monitoring bilirubin trajectory offers a simple yet powerful prognostic tool. Patients who fail to meet the day 15 target should undergo early imaging to evaluate stent function, with consideration for repeat ERCP, multi-segmental drainage, or percutaneous access in cases of complex hilar obstruction. Integrating these biochemical checkpoints into routine follow-up can improve timely intervention and outcomes.
AKI emerged as a critical adverse prognostic factor. Patients with AKI had higher baseline bilirubin and ALP levels and exhibited higher re-intervention rates and mortality. The interplay between obstructive jaundice and renal dysfunction is multifaceted. Cholestasis promotes systemic inflammation, bile-salt nephrotoxicity, and hemodynamic alterations that predispose to renal ischemia. Conversely, impaired renal clearance can exacerbate hyperbilirubinemia by reducing excretion of bilirubin conjugates[15]. Previous work, including Weston et al[4] and Mikalsen et al[15], has also identified renal dysfunction as an indicator of poor tolerance to biliary procedures and higher early mortality, un
The novelty of this study lies in establishing specific and clinically actionable bilirubin-based milestones, ≥ 50% reduction by day 7 and < 3 mg/dL by day 15, as predictors of both procedural adequacy and short-term survival fo
This study emphasizes that post-ERCP biochemical trends are as crucial as procedural success metrics. Serial bilirubin and ALP measurements provide objective evidence of functional drainage and can identify early failure before overt clinical deterioration occurs. Relative decline (Δ-bilirubin ≥ 50%) reflects immediate response, whereas absolute normalization (< 3 mg/dL by day 15) predicts sustained recovery. Together, the two indices can serve as performance benchmarks for endoscopic drainage procedures. For endoscopists, these findings support the adoption of bilirubin kinetics as a quality-of-care indicator. Early bilirubin non-response should trigger a systematic review for residual obstruction, stent malfunction, or unrecognized sepsis. In oncology practice, bilirubin decline could guide the safe timing of systemic therapy and reduce unnecessary delays in initiating treatment. Moreover, identifying high-risk subgroups, like elderly patients, those with AKI, or malignant hilar lesions, can inform tailored post-procedure monitoring protocols.
This study has certain limitations that warrant consideration. As a single-center study, the findings may not be generalizable to diverse patient populations or practice settings, and therefore, multicenter prospective studies are needed to validate these observations. Owing to logistical constraints, the number of patients who received self-expandable metal stents was relatively small, which may have limited the ability to discern the expected differences in outcomes compared with plastic stents. Future studies with a higher proportion of self-expandable metal stents placements could provide more definitive insights into their relative efficacy and clinical impact. The three-month follow-up period, although sufficient for evaluating the kinetics of bilirubin decline and short-term clinical outcomes, was inadequate for assessing long-term survival and stent patency. An extended follow-up at six months or beyond would better elucidate the prognostic implications of early biochemical response. Furthermore, the sample size in specific subgroups, particularly those defined by cholangitis severity and stent type, may have been insufficient to achieve adequate statistical power, potentially masking clinically meaningful associations. Finally, histopathological confirmation was not uniformly available for all cases of malignant obstruction, which may have introduced diagnostic heterogeneity.
In conclusion, this study demonstrates that the rate of bilirubin decline after EBD provides meaningful insight into drainage adequacy and prognosis in EHBO. Benign etiologies exhibit faster normalization, yet the relative fall in bilirubin is comparable across causes, highlighting the importance of dynamic indices such as Δ-bilirubin. Younger age and benign disease predict rapid recovery, whereas high baseline bilirubin, elevated ALP, malignancy, and AKI portend slower clearance and higher morbidity. Failure to achieve bilirubin > 50% at day 7 was an independent predictor of reintervention, and failure to achieve bilirubin < 3 mg/dL by day 15 was an independent predictor of mortality. These post-ERCP bilirubin kinetics are clinically meaningful, prognostically relevant, and readily measurable in routine practice. These parameters should be considered for incorporation into standardized post-EBD monitoring pathways and may serve as quality-of-care indicators in endoscopic management of EHBO.
| 1. | Odongo CN, Dreque CC, Mutiibwa D, Bongomin F, Oyania F, Sikhondze MM, Acan M, Atwine R, Kirya F, Situma M. Etiology, Clinical Presentations, and Short-Term Treatment Outcomes of Extrahepatic Obstructive Jaundice in South-Western Uganda. Clin Exp Gastroenterol. 2022;15:79-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Sharma MP, Ahuja V. Aetiological spectrum of obstructive jaundice and diagnostic ability of ultrasonography: a clinician's perspective. Trop Gastroenterol. 1999;20:167-169. [PubMed] |
| 3. | Sahu SK, Nath P, Mallick B, Praharaj D, Giri S, Panigrahi SC, Anand AC. Etiological Profile of Obstructive Jaundice and Acute Cholangitis: Three-year Data from a Tertiary Care Center in Eastern India. Euroasian J Hepatogastroenterol. 2024;14:187-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Weston BR, Ross WA, Wolff RA, Evans D, Lee JE, Wang X, Xiao LC, Lee JH. Rate of bilirubin regression after stenting in malignant biliary obstruction for the initiation of chemotherapy: how soon should we repeat endoscopic retrograde cholangiopancreatography? Cancer. 2008;112:2417-2423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Keulen AV, Gaspersz MP, van Vugt JLA, Roos E, Olthof PB, Coelen RJS, Bruno MJ, van Driel LMJW, Voermans RP, van Eijck CHJ, van Hooft JE, van Lienden KP, de Jonge J, Polak WG, Poley JW, Pek CJ, Moelker A, Willemssen FEJA, van Gulik TM, Erdmann JI, Hol L, IJzermans JNM, Büttner S, Koerkamp BG. Success, complication, and mortality rates of initial biliary drainage in patients with unresectable perihilar cholangiocarcinoma. Surgery. 2022;172:1606-1613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 6. | Pausawasdi N, Termsinsuk P, Charatcharoenwitthaya P, Limsrivilai J, Kaosombatwattana U. Development and validation of a risk score for predicting clinical success after endobiliary stenting for malignant biliary obstruction. PLoS One. 2022;17:e0272918. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 7. | Kiriyama S, Kozaka K, Takada T, Strasberg SM, Pitt HA, Gabata T, Hata J, Liau KH, Miura F, Horiguchi A, Liu KH, Su CH, Wada K, Jagannath P, Itoi T, Gouma DJ, Mori Y, Mukai S, Giménez ME, Huang WS, Kim MH, Okamoto K, Belli G, Dervenis C, Chan ACW, Lau WY, Endo I, Gomi H, Yoshida M, Mayumi T, Baron TH, de Santibañes E, Teoh AYB, Hwang TL, Ker CG, Chen MF, Han HS, Yoon YS, Choi IS, Yoon DS, Higuchi R, Kitano S, Inomata M, Deziel DJ, Jonas E, Hirata K, Sumiyama Y, Inui K, Yamamoto M. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25:17-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 468] [Cited by in RCA: 487] [Article Influence: 60.9] [Reference Citation Analysis (0)] |
| 8. | Levin A, Stevens PE. Summary of KDIGO 2012 CKD Guideline: behind the scenes, need for guidance, and a framework for moving forward. Kidney Int. 2014;85:49-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 599] [Article Influence: 46.1] [Reference Citation Analysis (0)] |
| 9. | Muckova N, Che K, Srikureja W, Olafsson S. Percentage Decrease in Total Serum Bilirubin after ERCP Therapy for Obstructive Jaundice is Similar for Malignant and Benign Causes. Am J Gastroenterol. 2008;103:S66-S67. [DOI] [Full Text] |
| 10. | Ipek S, Alper E, Cekic C, Cerrah S, Arabul M, Aslan F, Unsal B. Evaluation of the effectiveness of endoscopic retrograde cholangiopancreatography in patients with perihilar cholangiocarcinoma and its effect on development of cholangitis. Gastroenterol Res Pract. 2014;2014:508286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Malokar R, Jain S, Joshi M, Debnath P, Jena A, Rane S, Patel S, Gandhi H, Chudasama J, Pandey D, Mavuri V, Sundaram S, Chandnani S, Rathi P. Efficacy of ≥ 50% biliary drainage in advanced unresectable malignant hilar biliary obstruction: A prospective study. Indian J Gastroenterol. 2025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Hybner L, Tabushi FI, Collaço LM, Rosa ÉGD, Rocha BFMD, Bochnia MF. Does Age Influence in Endoscopic Therapeutic Success on the Biliary Tract? Arq Bras Cir Dig. 2022;34:e1607. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 13. | Dorrell R, Pawa S, Pawa R. Endoscopic Management of Malignant Biliary Stricture. Diagnostics (Basel). 2020;10:390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Ingabire Z, Hanna AB, Sebera E, Murayire J, Mohamed GS, Rutaganda E, Shikama F, Mukanumviye MS, Nyampinga D, Dadamessi I, Dua K, Berhane R. Management and outcomes of patients with obstructive jaundice from pancreatobiliary diseases in Rwanda. BMC Gastroenterol. 2025;25:535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Mikalsen IM, Breder S, Medhus AW, Folseraas T, Aabakken L, Ånonsen KV. ERCP for the initial management of malignant biliary obstruction - real world data on 596 procedures. Scand J Gastroenterol. 2024;59:369-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/