Published online Sep 16, 2025. doi: 10.4253/wjge.v17.i9.108639
Revised: May 24, 2025
Accepted: August 8, 2025
Published online: September 16, 2025
Processing time: 146 Days and 6.6 Hours
Achalasia is a rare esophageal motility disorder characterized by the inability of the lower esophageal sphincter (LES) to relax, accompanied by the loss of peristalsis in the esophageal body. Although more prevalent in adults, pediatric achalasia poses unique diagnostic challenges due to its atypical presentation. Peroral Endoscopic Myotomy (POEM) has emerged as a minimally invasive alternative to laparoscopic Heller myotomy for managing achalasia, particularly in children, but its efficacy and safety remain under-investigated. A comprehensive literature review was conducted to assess the role of POEM in pediatric achalasia, focusing on procedure efficacy, clinical outcomes, and safety. Key parameters included pre- and post-procedure Eckardt scores and adverse events. Comparison of outcomes with alternative interventions, such as laparoscopic myotomy and pneumatic dilation were also investigated. Currently, POEM achieves high clinical success in pediatric patients, with significant reduction in post-procedure Eckardt scores and LES pressures. Clinical success rates of up to 90% with durable symptom relief have been observed over follow-up exceeding one year. Common adverse events include mucosal injury, capnoperitoneum, and postoperative reflux. This comprehensive review reveals that POEM is as effective as laparoscopic myotomy but offers shorter hospital stay and reduced recovery time at the cost of a higher complication rate. POEM is an effective treatment for pediatric achalasia, providing durable symptom relief, comparable to traditional interventions. Future research should focus on the identification of pediatric patients that would benefit the most from POEM.
Core Tip: In pediatric patients with achalasia, peroral endoscopic myotomy (POEM) has shown high clinical success rates, achieving significant reduction in post-procedure symptoms and esophageal pressures. The current literature shows clinical success of up to 90% with durable symptom relief lasting over a year. Compared to traditional treatments, POEM offers shorter hospital stays and reduced recovery times at the cost of a higher complication rate. As the field continues to evolve, future research should focus on minimizing potential side effects and identifying children that will benefit the most from this procedure.
- Citation: Belimezakis N, Gianni P, Geropoulos G, Giannis D. Peroral endoscopic myotomy in children with achalasia: A review of the literature. World J Gastrointest Endosc 2025; 17(9): 108639
- URL: https://www.wjgnet.com/1948-5190/full/v17/i9/108639.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i9.108639
Achalasia is a rare primary motility disorder of the esophagus[1], characterized by the loss of esophageal peristalsis and insufficient relaxation of the lower esophageal sphincter (LES). Achalasia impairs the passage of solid food and liquids into the stomach, causing symptoms such as dysphagia, regurgitation, chest pain and weight loss[2,3]. Achalasia in children is rare, with an estimated annual incidence of 2 to 31 cases per 107 children, approximately 10 times less frequent than in adults[2].
Children with achalasia most commonly present with dysphagia, regurgitation, chest pain, emesis, odynophagia, weight loss/poor weight gain or impaired growth[4]. The symptoms are less specific in younger children[5] and include refusal of oral intake, failure to thrive, oropharyngeal dysphagia, aspiration, vomiting, abdominal pain, and nocturnal cough[6]. Non-specific symptoms may lead to misdiagnosis[7] and diagnostic delay (up to 6-10 years)[5].
Achalasia is related to an imbalance between the inhibitory and excitatory activity of esophageal nerve cells, as a result of the degeneration of the inhibitory myenteric plexus, that innervates the LES and the esophageal body[8]. Loss of inhibitory nitric oxide-producing and cholinergic neurons results in the loss of esophageal peristaltic waves and impaired LES relaxation. The pathogenetic mechanisms of neuronal degeneration in achalasia have not been completely characterized. Previous studies have suggested an association between achalasia and viral or parasitic infections[9-13]. The risk of achalasia is greater in people with allergic disorders, adrenal insufficiency, Allgrove syndrome (achalasia, adrenal deficiency, alacrimation)[14,15], and neurological disorders, such as familial dysautonomia[16,17]. A genetic predisposition has also been suggested, based on cases associated with Down syndrome or familial achalasia. Autoimmune mechanisms have also been suspected to cause degeneration of esophageal nerve cells[16,17].
Achalasia may be diagnosed with a barium swallow study that demonstrates a dilated esophagus with tapering of the distal end (‘bird’s beak’)[6,18]. However, the diagnostic gold standard is esophageal manometry[19] (Table 1). Achalasia is classified in 3 main subtypes according to the Chicago classification: (I) Achalasia characterized by absent distal esophageal pressurization; (II) Achalasia characterized by panesophageal pressurization; and (III) Achalasia characterized by 2 or more spastic contractions with or without periods of pressurization[20,21]. Achalasia subtype I is associated with elevated integrated relaxation pressure (IRP) (> 15 mmHg) and complete absence (100%) of peristalsis, while subtype II is also associated with increased IRP and patients commonly present with weight loss. Patients with achalasia subtype III more commonly present with chest pain. Of note, this subtype is not widely accepted, particularly in pediatric patients where it is exceedingly rare[22]. The subtype classification of achalasia has significant clinical implications, because patients in subtype II are more likely to respond to operative intervention[23]. However, it is important to note that occasionally pediatric patients may not be able to tolerate high-resolution manometry[24].
| Aspect | Details |
| Diagnostic methods | 1 Barium swallow study: Demonstrates dilated esophagus with tapering distal esophagus ("bird's beak sign") |
| 2 Esophageal manometry: Gold standard for diagnosis | |
| Achalasia subtypes | Subtype I: Absent distal esophageal pressurization |
| Subtype II: Panesophageal pressurization | |
| Subtype III (A, B, C, D): Spastic contractions (≥ 2) with or without periods of pressurization | |
| A: Spastic achalasia: Premature/spastic contractions with impaired LES relaxation | |
| B: Hypercontractile achalasia: High amplitude and long-duration contractions with incomplete LES relaxation | |
| C: Segmental achalasia: Abnormal contractions limited to specific segments (commonly distal third) | |
| D: Peristaltic achalasia: Proximal esophageal peristalsis retained with distal esophagus spastic activity | |
| Clinical presentation | Subtype I: 100% failure of peristalsis |
| Subtype II: Increased IRP, commonly associated with weight loss | |
| Subtype III: Chest pain common symptom | |
| Clinical implications | Patients with subtype II are more likely to respond to operative interventions |
A new endoscopic classification, that has not been widely accepted, was proposed by Li and Linghu[25] in 2013 (Ling classification). This classification is mainly used for the selection of patients eligible for endoscopic myotomy, and includes 3 types: (I) No multi-ring, crescent-like structure or diverticulum structure; (II) Presence of multi-ring or crescent-like structure but without diverticulum structure; and (III) Presence of diverticulum structure[26,27]. Type III achalasia is the most rare (approximately 10% of patients with achalasia) and the most difficult to treat[27].
Severe complications of achalasia in children include aspiration pneumonia, malnutrition due to inadequate oral intake, esophagitis, esophageal perforation, and increased risk of esophageal squamous cell carcinoma. The management of achalasia in children may include medical treatments (botulinum toxin injection, oral nitrates and calcium channel blockers), laparoscopic Heller Myotomy (LHM)[28], pneumatic dilation (PD)[29], and peroral endoscopic myotomy (POEM). Currently, there is inadequate evidence regarding the optimal treatment of pediatric achalasia and there is high heterogeneity in its management worldwide. This review provides an up-to-date overview of the utilization of POEM in children with achalasia, based on a thorough analysis of existing literature.
A systematic literature search was conducted (last search date: November 11, 2024) in PubMed with combinations and variations of the following keywords: "POEM", "per-oral endoscopic myotomy", “peroral endoscopic myotomy”, "pediatric achalasia", “child* achalasia”. Original research studies that involved pediatric populations (< 18 years) or mixed populations with pediatric data were included. Studies that only included adults (> 18 years) were excluded. Data extraction was performed independently by two reviewers to assess study design, patient characteristics, and outcomes. The narrative synthesis was structured around key variables of interest, such as efficacy, procedure-specific details, adverse events, and long-term outcomes.
In 2007, Pasricha et al[30] described the efficacy of submucosal endoscopic esophageal myotomy in animal models of achalasia, and subsequently the POEM procedure was introduced as a less invasive alternative to LHM in Japan in 2008 by Inoue et al[31]. Following the establishment of its efficacy and safety in adult patients, the POEM procedure has become an important alternative treatment for achalasia in children[32].
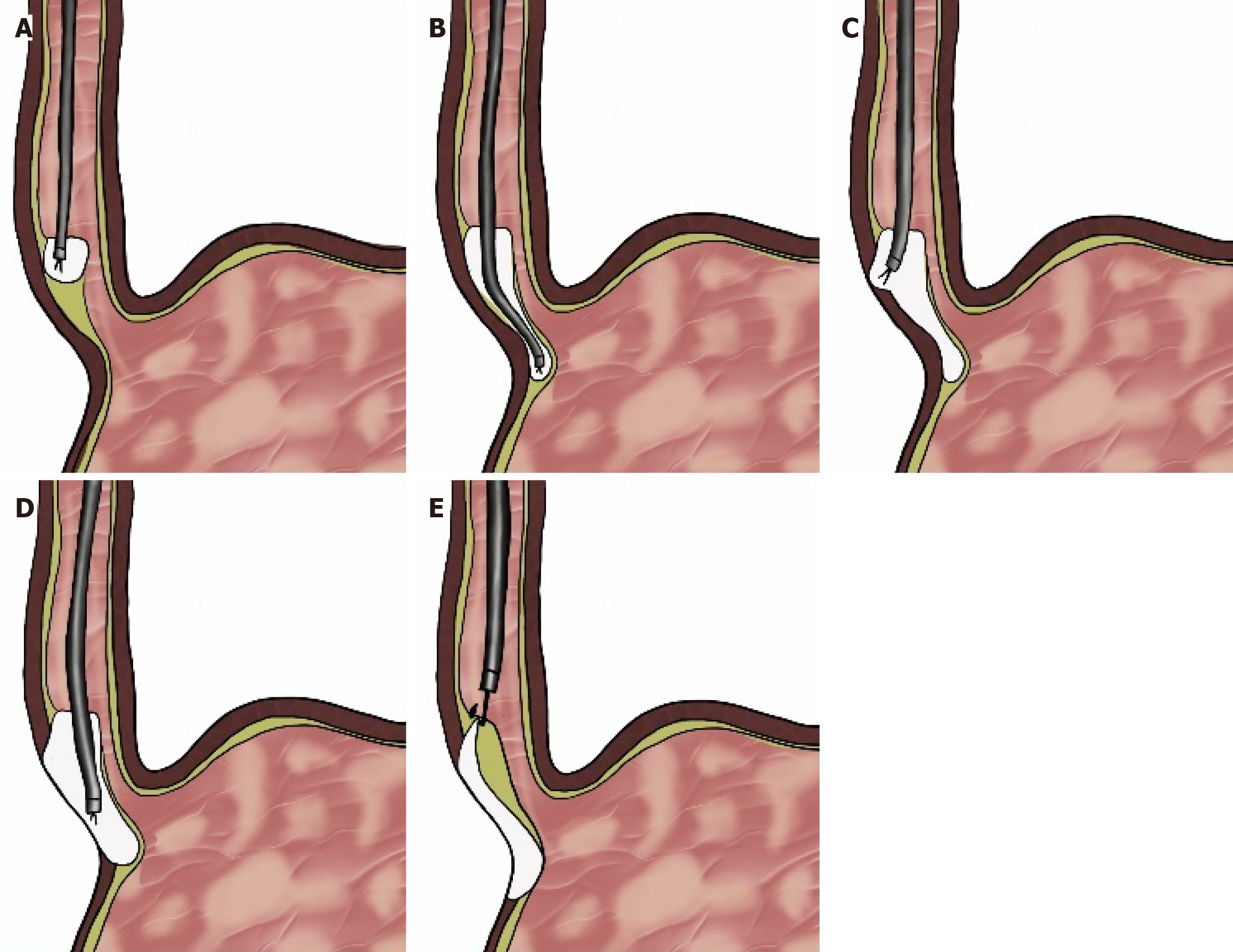
POEM requires careful pre-procedure preparation to ensure optimal outcomes in pediatric patients. The day before POEM pediatric patients receive a liquid diet and prophylactic antibiotics are given prior to scope insertion. POEM in pediatric patients is most commonly performed under general anesthesia via endotracheal intubation and a standard single-channel endoscope[33,34]. The preferred insufflating agent is carbon dioxide[35]. POEM is a procedure that is associated with unique challenges for anesthesiologists and requires specialized anesthesia management considering the risk of pneumomediastinum/pneumoperitoneum[36]. The average duration of POEM is 63 minutes[3]. The basic steps of POEM include: (1) Insertion of the endoscope into the submucosal space through a mucosotomy; (2) Creation of a submucosal tunnel distally; (3) Myotomy performed with electrocautery; (4) Inspection of the tunnel after the myotomy; and (5) Repair of the mucosal incision with endoscopic clips[37] (Figure 1). The circular muscle layer is incised proximally 2-3 cm beyond the mucosal incision in the esophagus and distally to 2-3 cm into the gastric cardia[35], and the myotomy length in the pediatric literature ranges between 3-21 cm[16,34,38]. The preservation of the external longitudinal muscle fibers during the myotomy and the closure of the mucosal incision are two steps of utmost importance to minimize potential complications during POEM[31]. Postoperatively, the routine use of antibiotics has not been shown to prevent infection[39].
Recent studies have sought to optimize the efficacy, duration, and safety of POEM by defining the endpoint of POEM or through the use of different scopes. One such study by Rafeeqi et al[40] used endoFLIP, a device that uses a sensory balloon to obtain measurements of the area and pressure inside the esophagus, and demonstrated that endoFLIP is a valuable tool in diagnosing and managing achalasia. Another innovative approach to POEM has been proposed by Bapaye et al[41], who successfully performed the procedure in an 18-month old child using a transnasal ultra-slim gastroscope, instead of a standard gastroscope due to technical and/or anatomical space constraint. Lastly, in 2018, Nabi et al[42] conducted a retrospective study in 10 pediatric patients with achalasia (4 with type I, 5 with type II and 1 patient with type III) using a triangular knife with water jet and reported decreased procedure duration and clinical success in 9 patients with significant reduction in Eckardt scores at 1 month after POEM.
POEM is indicated in children with achalasia, including type III achalasia because it allows for a more extensive myotomy compared to LHM[43,44], and it is the next treatment in patients who have undergone previous treatments for achalasia, such as botulinum toxin injection, pneumatic dilation, and LHM[45]. The contraindications to perform POEM include prior irradiation to the mediastinum, severe pulmonary disease, coagulopathy, thrombocytopenia (< 30000-50000/μL), prior endoscopic mucosal resection, ablative therapy or mucosal resection that has compromised the integrity of the esophageal mucosa, and portal hypertension[6,45].
Current experience with POEM indicates that the technique can be applied successfully in pediatric populations[35]. The Eckardt score system that ranges between 0-12 and is a composite of points assigned to 4 symptoms (dysphagia, regurgitation, chest pain, and weight loss), remains the key indicator of clinical efficacy in the treatment of achalasia. Clinical success is defined as an Eckardt score less than 3[37,46].
Large studies with mixed pediatric and adult data have shown promising results for POEM. A retrospective study by Ramchandani et al[47] analyzed data from a mixed population of 220 adult and pediatric patients (mean age: 39 years, range 9-74) between 2013-2014 undergoing POEM in a single center and had a clinical success rate of 96%. In another study, Shiwaku et al[48] conducted a retrospective analysis of 100 patients (mean age 48.2 years, range 9-91 years) with a 3-month follow up and reported a mean pre-procedure and post-procedure IRP of 33.5 ± 15.2 mmHg and 15.3 ± 6.5 mmHg, respectively, significantly decreased Eckardt score from 5.9 ± 2.5 to 0.8 ± 0.9, respectively, and a clinical success rate of 99%. A subsequent multicenter study by the same research group included 1300 patients (mean age 47.2 years, range 3-95 years) who underwent POEM for achalasia and showed consistent results, with a clinical success rate of 95.1% at 3 months and 94.7% at one year post-procedure[49] (Table 2).
| Ref. | Year | Country | n | Population | Mean pre-POEM Eckardt score | Mean post-POEM Eckardt score |
| Bapaye et al[41] | 2023 | India | 1 | Children | NR | NR |
| Bi et al[28] | 2023 | China | 48 | Children | 8 | 1.1 |
| Caldaro et al[7] | 2015 | Italy | 9 | Children | 7 | 0 |
| Chen et al[50] | 2014 | China | 27 | Children | 8.3 | 0.7 |
| Choné et al[38] | 2019 | France | 117 | Children | 7.5 | 0.9 |
| Familiari et al[29] | 2013 | Italy | 3 | Children | 5.3 | 0 |
| Filser et al[85] | 2015 | Germany | 1 | Children | 8 | 1 |
| Hsu et al[5] | 2023 | Taiwan | 10 | Children | 5.7 | 1.1 |
| Kethman et al[23] | 2017 | United States | 10 | Children | 7 | 2.4 |
| Korrapati et al[99] | 2018 | India | 15 | Children | 7 | 1 |
| Li et al[87] | 2014 | China | 9 | Children | 7 | 0.8 |
| Liu et al[34] | 2019 | China | 130 | Children | 7.4 | 0.7 |
| Luvsandagva et al[53] | 2024 | Mongolia | 12 | Children | 7 | 1 |
| Mangiola et al[88] | 2018 | Italy | 26 | Children | 7.2 | 0.3 |
| Miao et al[33] | 2017 | China | 21 | Children | 7.18 | 0.75 |
| Nabi et al[75] | 2017 | India | 502 | Children & adults | 7.1 | 1.1 |
| Nabi et al[42] | 2018 | India | 10 | Children | 6.7 | 0.3 |
| Nabi et al[68] | 2019 | India | 44 | Children | 6.86 | 1.03 |
| Nabi et al[16] | 2022 | India | 69 | Children | 7 | 1 |
| Nabi et al[76] | 2019 | India | 17 | Children | 6.88 | NR |
| Nishimoto et al[86] | 2018 | Japan | 13 | Children | 7.0 | 1.1 |
| Petrosyan et al[4] | 2016 | United States | 33 | Children | 9.7 | 0.9 |
| Petrosyan et al[32] | 2022 | United States | 37 | Children | 6.73 | 0.6 |
| Peng et al[43] | 2022 | China | 24 | Children | 7.67 | 0.67 |
| Pop et al[24] | 2022 | Romania | 7 | Children | 6.5 | NR |
| Ramchandani et al[47] | 2016 | India | 220 | Children & adults | 7.2 | 1.18 |
| Ren et al[69] | 2012 | China | 119 | Children & adults | NR | NR |
| Rizzo et al[14] | 2020 | Europe | 1 | Children | 12 | 0 |
| Saez et al[89] | 2020 | Chile | 5 | Children | 10 | 0.5 |
| Samarakkody et al[90] | 2022 | New Zealand | 4 | Children | 5.5 | 0 |
| Samejima et al[54] | 2023 | Japan | 10 | Children | 6.4 | 0.5 |
| Shiwaku et al[48] | 2016 | Japan | 100 | Children & adults | 5.9 | 0.8 |
| Shiwaku et al[49] | 2019 | Japan | 1300 | Children & adults | 6.1 | 1.1 |
| Smirnov et al[91] | 2018 | Russia | 1 | Children | 7 | 1 |
| Stavropoulos et al[92] | 2017 | United States | 10 | Children | 7.9 | 0.4 |
| Tan et al[93] | 2016 | China | 12 | Children | 6.9 | 0.7 |
| Tang et al[51] | 2015 | China | 5 | Children | 7.5 | 0.7 |
| van Lennep et al[18] | 2019 | Netherlands | 68 | Children | NR | NR |
| Wood et al[52] | 2020 | United States | 21 | Children | 7 | 1 |
| Yamashita et al[94] | 2016 | Japan | 1 | Children | 7 | 0 |
| Yamashita et al[95] | 2018 | Japan | 218 | Children & adults | NR | NR |
| Yeung et al[96] | 2017 | China | 1 | Children | 9 | 0 |
| Zhang et al[67] | 2016 | China | 1679 | Children & adults | NR | NR |
A growing body of evidence from studies focusing exclusively on pediatric populations, has shown that POEM in children is as effective as it is in adults, considering a significant reduction between the pre- and post-POEM Eckardt scores[38,50]. A small retrospective study by Tang et al[51] in 2015, analyzed 5 pediatric patients that underwent POEM and reported a median operative time of 50 minutes (range: 40-90 minutes), a median submucosal tunnel length of 13 cm (range 7-15 cm), a median myotomy length of 8 cm (range: 6-11 cm), and successful treatment with Eckardt scores of less than 3 at a median follow-up of 18 months in all patients. These findings were consistent with a previous study by Familiari et al[29] in 2013 that showed decreased Eckardt scores (equal to zero) at 1 year follow up after POEM compared to a score of 5.3 at baseline. These results were further supported by a long-term single center study in 2018 by Miao et al[33] who investigated POEM in a cohort of 21 children and reported an average duration of 40 min, a significant decrease of 7 points between pre-POEM and post-POEM scores, and a success rate of 100%. More recent data from a multicenter international retrospective study showed clinical success (> 90%) of POEM in 117 patients who had an average baseline Eckardt score of 7.5 ± 2.0 compared to 0.9 ± 1.2 at a mean follow up of 545 days[38]. In 2020, Wood et al[52] conducted a single institution prospective cohort study in 21 pediatric patients who underwent POEM between 2014-2019 and reported a median Eckardt score of 1.0 ± 2.0 at 1-month follow-up, a score of 2.0 (range: 0-5) at 2.7 months follow-up (n = 18) and a score of 2.0 ± 1.4 at 1-year follow-up (n = 10), significantly improved from a pre-procedure score of 7.0 ± 2.0. In line with these findings, a study by Liu et al[34] that included 130 consecutive pediatric patients post-POEM, showed a mean preoperative Eckardt score and median LES pressure of 7.4 and 27.1 mmHg that significantly improved to 0.7 and 7.0 mmHg, respectively. In 2023, Bi et al[28] conducted a long-term follow-up (5.7 years) retrospective study in 34 pediatric patients after POEM and reported a clinical success rate of 97.2% and average post-POEM Eckardt score of 1.1 (range: 0-4) compared to baseline score of 8.0 (range: 4-11). The effectiveness of POEM in pediatric patients with achalasia was further demonstrated in the retrospective cohort study conducted by Luvsandagva et al[53] in 2024, that showed a notable post-procedure improvement of the IRP from a mean of 26.8 ± 5.4 mmHg pre-procedure to 10.8 ± 1.1 mmHg at 12 months (P < .001). Similarly, the Eckardt score decreased significantly to 1.0 ± 1.7 at 3 days post-procedure and remained stable at 1.0 ± 1.7 at one year post-procedure from a pre-procedure mean of 7.0 ± 1.0, reflecting enhanced patient quality of life and symptom alleviation. The outcomes of POEM in pediatric patients under 12 years of age (4 patients) were compared with those of patients aged between 13-18 years (6 patients) in the recent study by Samejima et al[54]. At three months after surgery, POEM demonstrated a 100% clinical success rate (Eckardt score < 3) in both groups and 50% of the patients in both groups experienced gastroesophageal reflux disease (GERD), which was treated with antacids in 2 patients of each group. The postoperative outcomes at 12 months were comparable and the clinical success rate remained at 100%.
Data from previous studies in purely pediatric populations were summarized by Lee et al[55] in a systematic review and meta-analysis of 12 studies involving 146 pediatric patients that showed a decrease in Eckardt score by 6.88 points (95%CI: 6.28-7.48, P < 0.001) and LES pressure by 20.73 mmHg (95%CI: 15.76-25.70, P < 0.001) post-POEM. The majority of the population experienced improvement or resolution of short-term (< 12 months - 96%) and long-term symptoms (> 12 months - 93%). An updated systematic review and meta-analysis by Nabi et al[3] published in 2022 identified 14 studies including 419 patients and showed similar results with a cumulative technical success rate of 97.1%, clinical success rate of 94.4%, and an average reduction in Eckardt scores of 6.71 points. Lastly, the most recent systematic review and meta-analysis published in 2024, reported mean pre- and post-procedure reductions of Eckardt scores and LES pressures of 4.39 and 3.63 mmHg, respectively, with a mean procedure time of 83.6 minutes[56].
Based on these findings, the outcomes of POEM between pediatric and adult populations are comparable. In terms of technical success rates pediatric studies demonstrate high efficacy (90%-100%) that are comparable to those reported in adults (85%-100%). However, the anatomical considerations present unique challenges in pediatric patients, and technical difficulties in the creation of the submucosal tunnel due to underlying fibrosis may necessitate the abortion of the procedure[57]. The smaller caliber and variable anatomy of pediatric esophagi may require greater endoscopic expertise. Centers with higher procedural volumes and more experienced endoscopists tend to have lower complication rates, with early data showing that efficiency is achieved at 40 cases while mastery is achieved at 60 cases[58]. Later data from an important and methodologically rigorous study by Liu et al[59] in 2018 placed that threshold higher and showed that the learning curve for POEM is approximately 100 cases in mixed adult/pediatric populations. Above that threshold, the risk of technical failure, adverse events, and clinical failure significantly decrease. In that study, POEM was performed by endoscopists with extensive experience in endoscopic mucosal dissection and in a high-volume center. Suspected risk factors for failure include pre-procedural (pre-treatment Eckardt score, prolonged disease duration, prior achalasia treatment, dilated esophagus and sigmoid-shaped esophagus, achalasia other than type II and cardiac muscle thickness), intra-procedural (location/Length of myotomy, experience of the operator, mucosal injury), and post-procedural factors (GERD)[60]. Younger age and higher pre-procedural Eckardt score, which includes weight loss as one of its components, have been identified as predictors of poor response to POEM in mixed populations[61,62]. Furthermore, delayed diagnosis and treatment, can lead to significant weight loss and worse nutritional status, which are good surrogates for disease severity[63]. However, data regarding the duration of symptoms are conflicting, with earlier data of mixed adult/pediatric population from 2018 by Li et al[64] supporting that long disease duration greater than 10 years is a risk factor for recurrence, and later data from 2023-2024 studies showing no association with symptom duration[65,66].
The most common adverse events during POEM in pediatric patients include mucosal injury, capnoperitoneum, and retroperitoneal CO2[60] (Table 3). Major adverse events in pediatric patients include conversion to surgery, hemodynamic instability, bleeding requiring transfusion, aspiration pneumonia, prolonged hospital stay, post-procedure intensive care unit stay, and hospital readmission[3,34,35]. Mild perioperative adverse events include insufflation-related adverse events, mucosal injuries, minor bleeding, and pain requiring analgesic medications[43]. The adverse events may occur several months after the procedure[67].
| Ref. | Year | n | Mucosal perforation | Recurrent dysphagia | Wound infection | Pneumothorax | Pneumoperitoneum | Pneumomediastinum | Pneumonia | Subcutaneous emphysema | Fever | GERD | Reflux esophagitis | Leak within the tunnel/Dehiscence at entry site | Mucosotomy |
| Bapaye et al[41] | 2023 | 1 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Bi et al[28] | 2023 | 48 | 3 | - | - | - | 2 | - | - | 2 | - | - | - | - | - |
| Caldaro et al[7] | 2015 | 9 | 1 | - | - | - | 1 | - | - | - | - | 1 | - | - | - |
| Chen et al[50] | 2014 | 27 | 5 | - | - | 4 | - | 10 | - | 7 | 1 | 4 | 3 | - | - |
| Choné et al[38] | 2019 | 27 | - | - | - | - | - | - | - | - | - | 17 | 25 | - | - |
| Familiari et al[29] | 2013 | 3 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Filser et al[85] | 2015 | 1 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Hsu et al[5] | 2023 | 10 | - | - | - | - | 6 | 2 | - | 2 | 2 | - | - | - | - |
| Hu et al[97] | 2023 | 1 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Inoue et al[31] | 2010 | 10 | - | - | - | - | - | - | - | - | - | - | 1 | - | - |
| Kethman et al[23] | 2017 | 10 | - | - | - | 1 | 1 | - | - | - | - | - | - | 2 | - |
| Li et al[87] | 2014 | 9 | - | - | - | - | - | - | - | 1 | - | - | 1 | - | - |
| Liu et al[34] | 2019 | 130 | - | - | - | 1 | - | - | - | - | 30 | 17 | - | - | |
| Luvsandagva et al[53] | 2024 | 12 | - | 2 | - | - | - | - | - | 2 | - | 3 | 3 | - | - |
| Mangiola et al[88] | 2018 | 26 | - | - | - | - | 4 | - | 1 | 4 | - | - | - | - | - |
| Miao et al[33] | 2017 | 21 | - | - | - | - | 1 | 1 | - | 1 | 1 | 6 | 2 | - | - |
| Nabi et al[42] | 2018 | 10 | - | 1 | - | - | 2 | - | - | 1 | - | - | - | - | - |
| Nabi et al[76] | 2019 | 17 | - | - | - | - | 1 | - | - | - | - | - | 9 | - | - |
| Nabi et al[68] | 2019 | 44 | 1 | - | - | - | 10 | - | - | - | - | 12 | 11 | - | - |
| Nabi et al[16] | 2022 | 69 | - | - | - | - | - | - | - | - | - | 29 | 14 | - | - |
| Nabi et al[75] | 2017 | 502 | - | - | - | 5 | 62 | 1 | - | 106 | 1 | - | 53 | - | - |
| Nabi et al[98] | 2017 | 1 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Nishimoto et al[86] | 2018 | 13 | - | - | - | 1 | - | - | - | - | - | 1 | - | 1 | - |
| Petrosyan et al[4] | 2016 | 33 | 2 | 5 | 1 | 1 | - | - | - | - | - | - | - | - | - |
| Petrosyan et al[32] | 2022 | 37 | - | - | - | 9 | 10 | 2 | - | - | - | 3 | - | - | 5 |
| Pop et al[24] | 2022 | 4 | - | - | - | - | 2 | 1 | - | - | - | - | - | - | - |
| Ramchandani et al[47] | 2016 | 220 | 14 | - | - | 3 | 40 | - | - | 32 | - | - | 14 | - | - |
| Ren et al[69] | 2012 | 119 | - | 1 | - | 30 | 47 | 35 | - | 66 | - | - | - | - | - |
| Rizzo et al[14] | 2020 | 1 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Saez et al[89] | 2020 | 5 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Samarakkody et al[90] | 2022 | 4 | - | 1 | - | - | 1 | - | - | 1 | - | 1 | - | - | - |
| Samejima et al[54] | 2023 | 10 | - | - | - | - | - | - | - | - | - | - | 1 | - | - |
| Shiwaku et al[48] | 2016 | 100 | - | - | - | 1 | 11 | 1 | - | - | - | - | - | 1 | - |
| Shiwaku et al[49] | 2019 | 1300 | 5 | - | - | - | - | - | - | - | - | 173 | 1176 | - | - |
| Smirnov et al[91] | 2018 | 1 | - | - | - | - | - | - | - | - | - | - | - | 1 | - |
| Stavropoulos et al[92] | 2017 | 10 | 3 | - | - | - | - | - | - | - | - | - | 2 | - | - |
| Tan et al[93] | 2016 | 12 | - | - | - | - | - | - | - | 1 | - | - | 2 | - | - |
| Tang et al[51] | 2015 | 5 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| van Lennep et al[18] | 2019 | 68 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Wood et al[52] | 2020 | 21 | - | - | - | - | 1 | - | - | - | 1 | - | - | - | - |
| Yamashita et al[94] | 2016 | 1 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Yeung et al[96] | 2017 | 1 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Zhang et al[67] | 2016 | 1679 | - | - | - | 25 | - | - | - | - | - | - | - | - | - |
Rates of adverse events after POEM in pediatric patients vary widely across different studies. In 2016, Zhang et al[67] included 77 pediatric patients in their 5-year analysis, and reported 1 case of pneumothorax, no tunnel orifice dehiscence, no hydrothorax, and a total of 3 major adverse events (3.9%). In 2019 Nabi et al[68] conducted a retrospective study in 44 children post- POEM and found a 27.9% incidence of intra-operative adverse events, including retroperitoneal CO2, intraoperative capnoperitoneum requiring drainage, and intra-operative mucosal injury. Subsequently, in 2022, Petrosyan et al[32] reported a series of 37 children treated with POEM for achalasia that were followed at a mean of 22.6 months. Intraoperative complications occurred in 16 patients (43.2%), including mucosotomies outside of the site of POEM (13.5%), pneumomediastinum (5.4%), pneumothorax (24.3%), pneumoperitoneum (27%), failed POEM (2.7%). Postoperative complications included GERD (8.1%) and recurrent dysphagia (13.5%). In the 2023 retrospective study of Bi et al[28], that included 48 pediatric patients, the reported overall complications rate was lower (14.6%) compared to the other studies, and included mucosal injury (6.2%), pneumoperitoneum (4.2%), and subcutaneous emphysema (4.2%).
Higher rates of complications have been observed with the use of air as the insufflating agent in mixed pediatric/adult populations[69]. Another possible explanation for the variable incidence and higher rates of adverse events in some studies is that endoscopes used in POEM are designed for adults, and are relatively large for pediatric patients, thereby increasing the risk of mucosal injury. In addition, due to the smaller body size of pediatric patients, performing the procedure under adult conditions may be associated with excessive insufflation and severe emphysema. Therefore, further development of thinner endoscopes for therapeutic use and improvements in the CO2 insufflation system (such as transitioning from the current volume control method to a pressure control system similar to that used in laparoscopy) should be considered. Due to the anatomic difference between the child and adult esophagus, POEM in pediatric achalasia is performed with shorter length of myotomy. In addition, the thin esophageal wall of children requires caution during the establishment of the submucosal tunnel[2]. Most pediatric POEM procedures have traditionally employed myotomy lengths between 7.0-11.0 cm and submucosal tunnel length between 10.0-12.6 cm[2]. Recent studies have explored the feasibility of shorter myotomies in mixed populations and have shown comparable efficacy and safety between short (2.76-5 cm) and standard myotomy (6.9-10 cm)[70]. A shorter myotomy length may reduce the rate of reflux esophagitis and the risk of blown out myotomy, which is a pseudodiverticulum that gradually enlarges and affects esophageal emptying[71].
Pediatric literature comparing POEM with other treatments is limited. In adults, according to the ACG Clinical Guidelines[72] for the management of achalasia, PD, LHM and POEM are effective therapies with comparable outcomes in achalasia type I and II, while POEM would be a better option in achalasia type III. Pharmacological treatment options, such as calcium channel blockers or endoscopic botulinum toxin injections in the LES are rarely used in the pediatric population because of their short-term effectiveness and potential side effects of calcium-channel blockers, such as headache and dizziness[73]. Despite the limited evidence, POEM has shown promising results compared to PD and LHM in children[74] (Table 4). In the study by Nabi et al[75] in a mixed population of adults and children in 2018, outcomes of POEM as a first treatment were compared with outcomes of POEM as treatment for prior failure. They showed a significantly prolonged operative time (74.9 minutes vs 67.0 minutes, P = 0.002) in the group undergoing POEM as a treatment for failure, but success rates (92.4% vs 92.5%, P = 0.95) and adverse events associated with gas insufflation and mucosotomy were comparable between the groups. In 2019, the same group of authors evaluated POEM in a retrospective cohort of 53 pediatric patients, including 6 patients with prior PD, one with prior LHM, and one with both prior LHM and PD, and showed no difference in success rates (77.8% vs 100%, P = 0.471) and adverse events (33.3% vs 25%, P = 1.0) between “naïve” POEM and POEM for prior failure[76]. Based on the current evidence, the SAGES guidelines suggest that POEM and LHM are both appropriate choices in pediatric patients with type I or type II achalasia considering a shared-decision making between patients and providers, while POEM is recommended over LHM in type III pediatric achalasia based on expert experience[77].
| Treatment | Peroral endoscopic myotomy | Laparoscopic heller myotomy | Pneumatic dilation |
| Complications (%) | > 20 | 7-30 | 0-10 |
| Success rate (%) | 96.2-100 | 35-100 | 0-100 |
| Need for further surgery (%) | < 0.1 | 3-42 | 17-100 |
POEM and PD in pediatric patients have similar effectiveness as in adult patients, but in pediatric patients POEM may be associated with a higher rate of clinical success compared to PD. The main advantage of PD is its low cost and that it can be repeated if needed before or after myotomy[78]. Pooled data from a systematic review conducted in 2020 by Goneidy et al[74], who summarized 33 studies including 742 children treated for achalasia, showed that patients who underwent POEM instead of PD had more prior treatments (21.3% vs 9.1%), more complications (24.4% vs 5.0%), fewer comorbidities (0.01% vs 22.9%) and lower need for further surgical investigation (0.01% vs 62.3%). The success rate of POEM was 99.3% and the success rate of PD was 44.9%. POEM can be performed without technical difficulties in patients who previously had undergone PD, even in patients who had previously undergone PD twice[79]. Age should be taken into account, considering that age younger than 7 years is a negative predictive factor for PD success[78].
In both adults and pediatric patients, POEM and LHM yield comparable outcomes and complications. In adults, POEM and LHM have shown comparable results[80-82], but a meta-analysis by Marano et al[83], that included 196 patients that underwent POEM and 290 patient after LHM, showed that POEM resulted in a significantly shorter length of hospital stay and reduced symptomatic GERD. In pediatric patients, the retrospective study by Caldaro et al[7], that included 18 pediatric patients who underwent LHM (n = 9) or POEM (n = 9) between 2009 to 2013, found that POEM was associated with shorter procedure time and longer myotomy compared to LHM. According to the systematic review by Goneidy et al[74], POEM had a higher clinical success rate (99.3%) compared to LHM (77.9%), and patients with LHM had undergone more prior treatments (30%) than patients with POEM (21.3%), and more frequently had comorbidities (18.8% vs 0.01%) and needed further surgical intervention (10.9% vs 0.01%). Nevertheless, POEM was associated with an approximately two-fold higher risk of complications (24.4%) compared to LHM (12.8%). The current evidence indicates that POEM is superior to LHM in terms of efficacy at the cost of a higher complication rate.
Achalasia in children is a rare condition, and its management is a significant challenge. Based on the current literature, POEM has the potential to become the first-line treatment for achalasia in pediatric patients in the future. POEM appears to have the highest success rate, but it has been associated with higher complication rates compared to LHM and PD. POEM is a relatively new technique that has been applied to pediatric patients only since 2008, and the existing data in the literature are promising but not sufficient to definitively favor one therapeutic option over another. Identifying and individualizing the most appropriate treatment for achalasia in children through shared decision making between providers and patients/parents is crucial, considering a long life-expectancy, and the effect that achalasia exerts on their quality of life. The need for large, prospective trials involving children with achalasia is of utmost importance. Mussies et al[84] have proposed their protocol for a prospective international multicenter randomized controlled clinical trial and the results of this study are highly anticipated.
| 1. | Chiou EH. Poetry in motion: examining the role of peroral endoscopic myotomy in children. Gastrointest Endosc. 2015;81:101-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Zhong C, Tan S, Huang S, Peng Y, Lü M, Tang X. Clinical outcomes of peroral endoscopic myotomy for achalasia in children: a systematic review and meta-analysis. Dis Esophagus. 2021;34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Nabi Z, Talukdar R, Chavan R, Basha J, Reddy DN. Outcomes of Per-Oral Endoscopic Myotomy in Children: A Systematic Review and Meta-analysis. Dysphagia. 2022;37:1468-1481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Petrosyan M, Khalafallah AM, Guzzetta PC, Sandler AD, Darbari A, Kane TD. Surgical management of esophageal achalasia: Evolution of an institutional approach to minimally invasive repair. J Pediatr Surg. 2016;51:1619-1622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Hsu CT, Chen CC, Lee CT, Shieh TY, Wang HP, Wu MS, Lee JM, Wu JF, Tseng PH. Effect of peroral endoscopic myotomy on growth and esophageal motility for pediatric esophageal achalasia. J Formos Med Assoc. 2024;123:62-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Franklin AL, Petrosyan M, Kane TD. Childhood achalasia: A comprehensive review of disease, diagnosis and therapeutic management. World J Gastrointest Endosc. 2014;6:105-111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 82] [Cited by in RCA: 78] [Article Influence: 6.5] [Reference Citation Analysis (4)] |
| 7. | Caldaro T, Familiari P, Romeo EF, Gigante G, Marchese M, Contini AC, Federici di Abriola G, Cucchiara S, De Angelis P, Torroni F, Dall'Oglio L, Costamagna G. Treatment of esophageal achalasia in children: Today and tomorrow. J Pediatr Surg. 2015;50:726-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Park W, Vaezi MF. Etiology and pathogenesis of achalasia: the current understanding. Am J Gastroenterol. 2005;100:1404-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 257] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 9. | de Oliveira RB, Rezende Filho J, Dantas RO, Iazigi N. The spectrum of esophageal motor disorders in Chagas' disease. Am J Gastroenterol. 1995;90:1119-1124. [PubMed] |
| 10. | Sodikoff JB, Lo AA, Shetuni BB, Kahrilas PJ, Yang GY, Pandolfino JE. Histopathologic patterns among achalasia subtypes. Neurogastroenterol Motil. 2016;28:139-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 95] [Article Influence: 9.5] [Reference Citation Analysis (1)] |
| 11. | Jones DB, Mayberry JF, Rhodes J, Munro J. Preliminary report of an association between measles virus and achalasia. J Clin Pathol. 1983;36:655-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 49] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Robertson CS, Martin BA, Atkinson M. Varicella-zoster virus DNA in the oesophageal myenteric plexus in achalasia. Gut. 1993;34:299-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 120] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Furuzawa-Carballeda J, Aguilar-León D, Gamboa-Domínguez A, Valdovinos MA, Nuñez-Álvarez C, Martín-del-Campo LA, Enríquez AB, Coss-Adame E, Svarch AE, Flores-Nájera A, Villa-Baños A, Ceballos JC, Torres-Villalobos G. Achalasia--An Autoimmune Inflammatory Disease: A Cross-Sectional Study. J Immunol Res. 2015;2015:729217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 73] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 14. | Rizzo R, Balassone V, Torroni F, De Angelis P, Dall'Oglio L. Peroral endoscopic myotomy in a child with Triple A syndrome (Allgrove syndrome). VideoGIE. 2020;5:235-237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Jarzębicka D, Czubkowski P, Sieczkowska-Gołub J, Kierkuś J, Kowalski A, Stefanowicz M, Oracz G. Achalasia in Children-Clinical Presentation, Diagnosis, Long-Term Treatment Outcomes, and Quality of Life. J Clin Med. 2021;10:3917. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Nabi Z, Ramchandani M, Basha J, Goud R, Darisetty S, Reddy DN. POEM Is a Durable Treatment in Children and Adolescents With Achalasia Cardia. Front Pediatr. 2022;10:812201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Berquist WE, Byrne WJ, Ament ME, Fonkalsrud EW, Euler AR. Achalasia: diagnosis, management, and clinical course in 16 children. Pediatrics. 1983;71:798-805. [PubMed] |
| 18. | van Lennep M, van Wijk MP, Omari TIM, Salvatore S, Benninga MA, Singendonk MMJ; European Society for Paediatric Gastroenterology, Hepatology and Nutrition Motility Working Group. Clinical Management of Pediatric Achalasia: A Survey of Current Practice. J Pediatr Gastroenterol Nutr. 2019;68:521-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 19. | Poornachand V, Kumarasamy K, Karamath SP, Seenivasan V, Bavanandam S, Dheivamani N. Achalasia Cardia in a Young Infant. Indian J Pediatr. 2018;85:673-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 20. | Richter JE. High-resolution manometry in diagnosis and treatment of achalasia: help or hype. Curr Gastroenterol Rep. 2014;16:420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Mari A, Abu Baker F, Pellicano R, Khoury T. Diagnosis and Management of Achalasia: Updates of the Last Two Years. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 22. | Patel DA, Lappas BM, Vaezi MF. An Overview of Achalasia and Its Subtypes. Gastroenterol Hepatol (N Y). 2017;13:411-421. [PubMed] |
| 23. | Kethman WC, Thorson CM, Sinclair TJ, Berquist WE, Chao SD, Wall JK. Initial experience with peroral endoscopic myotomy for treatment of achalasia in children. J Pediatr Surg. 2018;53:1532-1536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | Pop D, Pop RS, Blaga TS, David L, Asavoaie C, Tantau M, Dumitrascu DL, Farcau D. New diagnostic and therapeutic procedures applied in pediatric esophageal achalasia in a pediatric tertiary center: A case series. Exp Ther Med. 2023;25:101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 25. | Li HK, Linghu EQ. New endoscopic classification of achalasia for selection of candidates for peroral endoscopic myotomy. World J Gastroenterol. 2013;19:556-560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 26. | Zhang WG, Linghu EQ, Chai NL, Li HK. Ling classification describes endoscopic progressive process of achalasia and successful peroral endoscopy myotomy prevents endoscopic progression of achalasia. World J Gastroenterol. 2017;23:3309-3314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Li MY, Wang QH, Chen RP, Su XF, Wang DY. Pathogenesis, clinical manifestations, diagnosis, and treatment progress of achalasia of cardia. World J Clin Cases. 2023;11:1741-1752. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (4)] |
| 28. | Bi YW, Lei X, Ru N, Li LS, Wang NJ, Zhang B, Yao Y, Linghu EQ, Chai NL. Per-oral endoscopic myotomy is safe and effective for pediatric patients with achalasia: A long-term follow-up study. World J Gastroenterol. 2023;29:3497-3507. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 29. | Familiari P, Marchese M, Gigante G, Boskoski I, Tringali A, Perri V, Costamagna G. Peroral endoscopic myotomy for the treatment of achalasia in children. J Pediatr Gastroenterol Nutr. 2013;57:794-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 30. | Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB, Hawes RH, Kalloo AN, Kantsevoy SV, Gostout CJ. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007;39:761-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 368] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 31. | Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1168] [Cited by in RCA: 1283] [Article Influence: 80.2] [Reference Citation Analysis (1)] |
| 32. | Petrosyan M, Mostammand S, Shah AA, Darbari A, Kane TD. Per Oral Endoscopic Myotomy (POEM) for pediatric achalasia: Institutional experience and outcomes. J Pediatr Surg. 2022;57:728-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 33. | Miao S, Wu J, Lu J, Wang Y, Tang Z, Zhou Y, Huang Z, Ying H, Zhou P. Peroral Endoscopic Myotomy in Children With Achalasia: A Relatively Long-term Single-center Study. J Pediatr Gastroenterol Nutr. 2018;66:257-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 34. | Liu Z, Wang Y, Fang Y, Huang Y, Yang H, Ren X, Xu M, Chen S, Chen W, Zhong Y, Zhang Y, Qin W, Hu J, Cai M, Yao L, Li Q, Zhou P. Short-term safety and efficacy of peroral endoscopic myotomy for the treatment of achalasia in children. J Gastroenterol. 2020;55:159-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 35. | Mencin AA, Sethi A, Barakat MT, Lerner DG. Peroral Endoscopic Myotomy (POEM) in Children: A State of the Art Review. J Pediatr Gastroenterol Nutr. 2022;75:231-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 36. | Manici M, İşgüzar AR, Adanur UD, Gürkan Y, Söğüt MS, Aslan F, Arıkan Ç. The Ventilatory Changes of Pediatric Peroral Endoscopic Myotomy Patients. Turk J Anaesthesiol Reanim. 2024;52:101-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 37. | Tashiro J, Petrosyan M, Kane TD. Current management of pediatric achalasia. Transl Gastroenterol Hepatol. 2021;6:33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 38. | Choné A, Familiari P, von Rahden B, Desai P, Inoue H, Shimamura Y, Eleftheriadis N, Yamashita K, Khashab MA, Shiwaku H, Seewald S, Draganov PV, Alvarez LBM, Chaussade S, Tantau M, Abraham M, Marks J, Arevalo G, Albéniz E, Mion F, Roman S, Rivory J, Dubois R, Lachaux A, Benech N, Subtil F, Ponchon T, Barret M, Pioche M. Multicenter Evaluation of Clinical Efficacy and Safety of Per-oral Endoscopic Myotomy in Children. J Pediatr Gastroenterol Nutr. 2019;69:523-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 39. | Maselli R, Oliva A, Badalamenti M, Galtieri PA, Belletrutti PJ, Spadaccini M, Nicoletti R, Finati E, Vetrano S, Fosso F, Correale C, Pellegatta G, Hassan C, Repici A. Single-dose versus short-course prophylactic antibiotics for peroral endoscopic myotomy: a randomized controlled trial. Gastrointest Endosc. 2021;94:922-929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 40. | Rafeeqi T, Salimi-Jazi F, Cunningham A, Wall J. The utility of Endoscopic Functional Luminal Imaging (EndoFLIP) in the diagnosis and management of children with achalasia. J Pediatr Surg. 2023;58:639-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 41. | Bapaye J, Korrapati SK, Gandhi A, Bapaye A. Modified technique of peroral endoscopic myotomy using transnasal ultra-slim gastroscope in a child with achalasia cardia. VideoGIE. 2023;8:60-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 42. | Nabi Z, Ramchandani M, Chavan R, Tandan M, Kalapala R, Darisetty S, Reddy DN. Peroral Endoscopic Myotomy in Children: First Experience With a New Triangular Knife. J Pediatr Gastroenterol Nutr. 2018;66:43-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 43. | Peng D, Tan Y, Li C, Lv L, Zhu H, Liang C, Li R, Liu D. Peroral Endoscopic Myotomy for Pediatric Achalasia: A Retrospective Analysis of 21 Cases With a Minimum Follow-Up of 5 Years. Front Pediatr. 2022;10:845103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 44. | Kumbhari V, Tieu AH, Onimaru M, El Zein MH, Teitelbaum EN, Ujiki MB, Gitelis ME, Modayil RJ, Hungness ES, Stavropoulos SN, Shiwaku H, Kunda R, Chiu P, Saxena P, Messallam AA, Inoue H, Khashab MA. Peroral endoscopic myotomy (POEM) vs laparoscopic Heller myotomy (LHM) for the treatment of Type III achalasia in 75 patients: a multicenter comparative study. Endosc Int Open. 2015;3:E195-E201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 173] [Cited by in RCA: 206] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 45. | Stavropoulos SN, Modayil R, Friedel D. Per oral endoscopic myotomy for the treatment of achalasia. Curr Opin Gastroenterol. 2015;31:430-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 46. | Eckardt VF. Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am. 2001;11:281-292, vi. [PubMed] |
| 47. | Ramchandani M, Nageshwar Reddy D, Darisetty S, Kotla R, Chavan R, Kalpala R, Galasso D, Lakhtakia S, Rao GV. Peroral endoscopic myotomy for achalasia cardia: Treatment analysis and follow up of over 200 consecutive patients at a single center. Dig Endosc. 2016;28:19-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 73] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 48. | Shiwaku H, Inoue H, Yamashita K, Ohmiya T, Beppu R, Nakashima R, Takeno S, Sasaki T, Nimura S, Yamashita Y. Peroral endoscopic myotomy for esophageal achalasia: outcomes of the first over 100 patients with short-term follow-up. Surg Endosc. 2016;30:4817-4826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 49. | Shiwaku H, Inoue H, Onimaru M, Minami H, Sato H, Sato C, Tanaka S, Ogawa R, Okushima N. Multicenter collaborative retrospective evaluation of peroral endoscopic myotomy for esophageal achalasia: analysis of data from more than 1300 patients at eight facilities in Japan. Surg Endosc. 2020;34:464-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 50. | Chen WF, Li QL, Zhou PH, Yao LQ, Xu MD, Zhang YQ, Zhong YS, Ma LL, Qin WZ, Hu JW, Cai MY, He MJ, Cui Z. Long-term outcomes of peroral endoscopic myotomy for achalasia in pediatric patients: a prospective, single-center study. Gastrointest Endosc. 2015;81:91-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 80] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 51. | Tang X, Gong W, Deng Z, Zhou J, Ren Y, Zhang Q, Chen Z, Jiang B. Usefulness of peroral endoscopic myotomy for treating achalasia in children: experience from a single center. Pediatr Surg Int. 2015;31:633-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 52. | Wood LS, Chandler JM, Portelli KE, Taylor JS, Kethman WC, Wall JK. Treating children with achalasia using per-oral endoscopic myotomy (POEM): Twenty-one cases in review. J Pediatr Surg. 2020;55:1006-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 53. | Luvsandagva B, Adyasuren B, Bagachoimbol B, Luuzanbadam G, Bai T, Jalbuu N, Duger D, Hou X. Efficacy and safety of peroral endoscopic myotomy for pediatric achalasia: A nationwide study. Medicine (Baltimore). 2024;103:e38970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 54. | Samejima Y, Yoshimura S, Okata Y, Sakaguchi H, Abe H, Tanaka S, Kodama Y, Bitoh Y. Peroral Endoscopic Myotomy in Pediatric Patients with Achalasia up to 12 Years of Age: A Pilot Study in a Single-Center Experience in Japan. Eur J Pediatr Surg. 2024;34:97-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 55. | Lee Y, Brar K, Doumouras AG, Hong D. Peroral endoscopic myotomy (POEM) for the treatment of pediatric achalasia: a systematic review and meta-analysis. Surg Endosc. 2019;33:1710-1720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 56. | Dimopoulou A, Dimopoulou D, Analitis A, Dimopoulou K, Dellaportas D, Zavras N. Laparoscopic Heller myotomy versus peroral endoscopic myotomy in children with esophageal achalasia: a systematic review and meta-analysis. Ann Gastroenterol. 2024;37:655-664. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 57. | Sbaraglia F, Familiari P, Maiellare F, Mecarello M, Scarano A, Del Prete D, Lamacchia R, Antonicelli F, Rossi M. Pediatric anesthesia and achalasia: 10 years' experience in peroral endoscopy myotomy management. J Anesth Analg Crit Care. 2022;2:25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 58. | Modayil R, Stavropoulos SN. How Many Peroral Endoscopic Myotomy Procedures Are Necessary for Proficiency? Clin Gastroenterol Hepatol. 2018;16:1393-1397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 59. | Liu Z, Zhang X, Zhang W, Zhang Y, Chen W, Qin W, Hu J, Cai M, Zhou P, Li Q. Comprehensive Evaluation of the Learning Curve for Peroral Endoscopic Myotomy. Clin Gastroenterol Hepatol. 2018;16:1420-1426.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 74] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 60. | Quénéhervé L, Vauquelin B, Berger A, Coron E, Olivier R. Risk factors for clinical failure of peroral endoscopic myotomy in achalasia. Front Med (Lausanne). 2022;9:1099533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 61. | Swei E, Wagh MS. Preoperative predictors of poor response to peroral endoscopic myotomy: Have we found the crystal ball? Gastrointest Endosc. 2021;93:406-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 62. | Ren Y, Tang X, Chen Y, Chen F, Zou Y, Deng Z, Wu J, Li Y, Huang S, Jiang B, Gong W. Pre-treatment Eckardt score is a simple factor for predicting one-year peroral endoscopic myotomy failure in patients with achalasia. Surg Endosc. 2017;31:3234-3241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 63. | Nicolas A, Aumar M, Tran LC, Tiret A, Duclaux-Loras R, Bridoux-Henno L, Campeotto F, Fabre A, Breton A, Languepin J, Kyheng M, Viala J, Coopman S, Gottrand F. Comparison of Endoscopic Dilatation and Heller's Myotomy for Treating Esophageal Achalasia in Children: A Multicenter Study. J Pediatr. 2022;251:134-139.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 64. | Li QL, Wu QN, Zhang XC, Xu MD, Zhang W, Chen SY, Zhong YS, Zhang YQ, Chen WF, Qin WZ, Hu JW, Cai MY, Yao LQ, Zhou PH. Outcomes of per-oral endoscopic myotomy for treatment of esophageal achalasia with a median follow-up of 49 months. Gastrointest Endosc. 2018;87:1405-1412.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 94] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 65. | Boutros CS, Khan SZ, Benson J, Lyons J, Hashimoto DA, Marks JM. Symptom duration is not associated with per oral endoscopic myotomy (POEM) failure. Surg Endosc. 2023;37:8000-8005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 66. | Benson J, Boutros CS, Khan SZ, Wieland P, Chatha HN, Katz G, Lyons J, Marks JM. Does preoperative symptom duration affect outcomes following per oral endoscopic myotomy (POEM)? Surg Endosc. 2024;38:5253-5258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 67. | Zhang XC, Li QL, Xu MD, Chen SY, Zhong YS, Zhang YQ, Chen WF, Ma LL, Qin WZ, Hu JW, Cai MY, Yao LQ, Zhou PH. Major perioperative adverse events of peroral endoscopic myotomy: a systematic 5-year analysis. Endoscopy. 2016;48:967-978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 100] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 68. | Nabi Z, Ramchandani M, Chavan R, Darisetty S, Kalapala R, Shava U, Tandan M, Kotla R, Reddy DN. Outcome of peroral endoscopic myotomy in children with achalasia. Surg Endosc. 2019;33:3656-3664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 69. | Ren Z, Zhong Y, Zhou P, Xu M, Cai M, Li L, Shi Q, Yao L. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases). Surg Endosc. 2012;26:3267-3272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 169] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 70. | Chandan S, Facciorusso A, Khan SR, Ramai D, Mohan BP, Bilal M, Dhindsa B, Kassab LL, Goyal H, Perisetti A, Bhat I, Singh S, McDonough S, Adler DG. Short versus standard esophageal myotomy in achalasia patients: a systematic review and meta-analysis of comparative studies. Endosc Int Open. 2021;9:E1246-E1254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 71. | Sanaei O, Singh S, Bhat I. Peroral endoscopic myotomy (POEM) for the treatment of achalasia: a narrative review of recent advances. Ann Laparosc Endosc Surg. 2024;9:33-33. [DOI] [Full Text] |
| 72. | Vaezi MF, Pandolfino JE, Yadlapati RH, Greer KB, Kavitt RT. ACG Clinical Guidelines: Diagnosis and Management of Achalasia. Am J Gastroenterol. 2020;115:1393-1411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 286] [Article Influence: 47.7] [Reference Citation Analysis (0)] |
| 73. | van Lennep M, van Wijk MP, Omari TIM, Benninga MA, Singendonk MMJ. Clinical management of pediatric achalasia. Expert Rev Gastroenterol Hepatol. 2018;12:391-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 74. | Goneidy A, Cory-Wright J, Zhu L, Malakounides G. Surgical Management of Esophageal Achalasia in Pediatrics: A Systematic Review. Eur J Pediatr Surg. 2020;30:13-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 75. | Nabi Z, Ramchandani M, Chavan R, Tandan M, Kalapala R, Darisetty S, Lakhtakia S, Rao GV, Reddy DN. Peroral endoscopic myotomy in treatment-naïve achalasia patients versus prior treatment failure cases. Endoscopy. 2018;50:358-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 62] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 76. | Nabi Z, Ramchandani M, Darisetty S, Kotla R, Reddy DN. Impact of prior treatment on long-term outcome of peroral endoscopic myotomy in pediatric achalasia. J Pediatr Surg. 2020;55:1552-1555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 77. | Kohn GP, Dirks RC, Ansari MT, Clay J, Dunst CM, Lundell L, Marks JM, Molena D, Rooker C, Saxena P, Swanstrom L, Wong RK, Pryor AD, Stefanidis D. SAGES guidelines for the use of peroral endoscopic myotomy (POEM) for the treatment of achalasia. Surg Endosc. 2021;35:1931-1948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 78. | Kotilea K, Mahler T, Bontems P, Devière J, Louis H. Management of esophageal motility disorders in children: a review. Acta Gastroenterol Belg. 2018;81:295-304. [PubMed] |
| 79. | Ling T, Pei Q, Pan J, Zhang X, Lv Y, Li W, Zou X. Successful use of a covered, retrievable stent to seal a ruptured mucosal flap safety valve during peroral endoscopic myotomy in a child with achalasia. Endoscopy. 2013;45 Suppl 2 UCTN:E63-E64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 80. | Hungness ES, Teitelbaum EN, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, Soper NJ. Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg. 2013;17:228-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 195] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 81. | Teitelbaum EN, Rajeswaran S, Zhang R, Sieberg RT, Miller FH, Soper NJ, Hungness ES. Peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy produce a similar short-term anatomic and functional effect. Surgery. 2013;154:885-91; discussion 891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 82. | Teitelbaum EN, Soper NJ, Pandolfino JE, Kahrilas PJ, Hirano I, Boris L, Nicodème F, Lin Z, Hungness ES. Esophagogastric junction distensibility measurements during Heller myotomy and POEM for achalasia predict postoperative symptomatic outcomes. Surg Endosc. 2015;29:522-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 133] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 83. | Marano L, Pallabazzer G, Solito B, Santi S, Pigazzi A, De Luca R, Biondo FG, Spaziani A, Longaroni M, Di Martino N, Boccardi V, Patriti A. Surgery or Peroral Esophageal Myotomy for Achalasia: A Systematic Review and Meta-Analysis. Medicine (Baltimore). 2016;95:e3001. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 73] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 84. | Mussies C, van Lennep M, van der Lee JH, Singendonk MJ, Benninga MA, Bastiaansen BA, Fockens P, Bredenoord AJ, van Wijk MP. Protocol for an international multicenter randomized controlled trial assessing treatment success and safety of peroral endoscopic myotomy vs endoscopic balloon dilation for the treatment of achalasia in children. PLoS One. 2023;18:e0286880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 85. | Filser J, Dick A, Meyer T, Germer CT, von Rahden BH. Peroral Endoscopic Myotomy for the Treatment of Achalasia in a 10-Year-Old Male Patient. European J Pediatr Surg Rep. 2015;3:18-22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 86. | Nishimoto M, Shimamura Y, Abad MRAZ, Mochizuki Y, Nishikawa Y, Ueno J, Fukuda H, Sumi K, Ikeda H, Onimaru M, Goda K, Ito H, Inoue H. Clinical outcome of per-oral endoscopic myotomy (POEM) in pediatric patients. J Gastroenterol Hepatol. 2018;33:546-548. |
| 87. | Li C, Tan Y, Wang X, Liu D. Peroral endoscopic myotomy for treatment of achalasia in children and adolescents. J Pediatr Surg. 2015;50:201-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 88. | Mangiola F, Familiari P, Landi R, Calì A, D'aversa F, Bove V, Boskoski I, Tringali A, Perri V, Costamagna G. Tu1149 peroral endoscopic myotomy for the treatment of achalasia in children: Experience of a single center with long term follow-up. Gastrointest Endosc. 2018;87:AB542. [DOI] [Full Text] |
| 89. | Saez J, Mejia R, Pattillo JC, Vuletin F, Monrroy H, Jaime F, Sharp A. Per oral endoscopic myotomy (POEM) in pediatric patients with esophageal achalasia: First Latin-American experience. J Pediatr Surg. 2021;56:706-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 90. | Samarakkody U, Weilert F, Cama J, Adams S. Lessons learned from early experience of per oral endoscopic myotomy in children. J Pediatr Surg. 2023;58:218-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 91. | Smirnov AA, Burakov AN, Shvetsov AN, Blinov EV, Semenikhin KD, Konkina NV, Dvoreckij SY. Peroral Endoscopic Myotomy in Diffuse Thickened Esophageal Wall in an Adolescent. Case Rep Gastroenterol. 2018;12:497-503. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 92. | Stavropoulos SN, Sosulski AB, Modayil RJ, Gurram KC, Brathwaite CE, Coren CV, Boinpally H, Grendell JH. Sa2075 Use of Peroral Endoscopic Myotomy (POEM) in Pediatric Patients as a Primary or Rescue Therapy for Achalasia. Gastrointest Endosc. 2017;85:AB285-AB286. [DOI] [Full Text] |
| 93. | Tan Y, Zhu H, Li C, Chu Y, Huo J, Liu D. Comparison of peroral endoscopic myotomy and endoscopic balloon dilation for primary treatment of pediatric achalasia. J Pediatr Surg. 2016;51:1613-1618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 94. | Yamashita K, Shiwaku H, Hirose R, Kai H, Nakashima R, Kato D, Beppu R, Takeno S, Sasaki T, Nimura S, Iwasaki A, Inoue H, Yamashita Y. Long-term outcome of peroral endoscopic myotomy for achalasia treatment in a 9-year-old female patient. Asian J Endosc Surg. 2016;9:332-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 95. | Yamashita K, Shiwaku H, Ohmiya T, Okada H, Inoue H, Hasegawa S. Safety and effectiveness of per-oral endoscopic myotomy in children with achalasia: a comparison of the results in paediatric and adult patients. United Eur Gastroenterol J. 2018;6:A135-A747. |
| 96. | Yeung F, Wong IYH, Chung PHY, Wong KKY, Law SYK, Tam PKH. Peroral Endoscopic Myotomy with EndoFLIP and Double-Endoscope: Novel Techniques for Achalasia in Pediatric Population. J Laparoendosc Adv Surg Tech A. 2018;28:343-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 97. | Hu X, Chen G, Gu Q, Chen X, Ji F. Peroral endoscopic myotomy in a 9-year-old girl with achalasia and annular stenosis in the lower esophagus. Rev Esp Enferm Dig. 2022;114:764-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 98. | Nabi Z, Ramchandani M, Reddy DN. Peroral Endoscopic Myotomy in a Child With Achalasia Cardia. J Pediatr Gastroenterol Nutr. 2017;65:e44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 99. | Korrapati SK, Nemade P, Mahadik M, Biradar V, Pujari R, Bapaye J, Bapaye A. Peroral endoscopic myotomy (POEM) for achalasia in children-single center experience. J Gastroenterol Hepatol. 2018;33:54-221. |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/