Published online Jul 16, 2025. doi: 10.4253/wjge.v17.i7.107059
Revised: April 22, 2025
Accepted: June 18, 2025
Published online: July 16, 2025
Processing time: 117 Days and 15.3 Hours
Ectopic gallbladder, occurring in 0.1% to 0.7% of the population, is rarely found in the left liver lobe without situs inversus totalis. Functional gallbladder disorder (FGBD), characterized by biliary pain without stones or sludge, affects 8% of men and 21% of women. No prior cases of concomitant FGBD and left-sided gallbla
A 73-year-old woman with a 20-year history of epigastric pain was diagnosed with a left-sided gallbladder and FGBD based on imaging findings and impaired gallbladder contraction. Laparoscopic cholecystectomy was performed and con
This is the first reported case of FGBD with a left-sided gallbladder. Preoperative imaging, such as magnetic resonance cholangiopancreatography or computed tomography, is crucial for identifying anatomical variations of the gallbladder. Laparoscopic cholecystectomy is feasible but requires careful planning to avoid complications.
Core Tip: This first-documented case describes a 73-year-old woman with two concurrent diagnoses: Functional gallbladder disorder and left-sided gallbladder, presenting with 20-year epigastric pain. Preoperative magnetic resonance imaging and computed tomography imaging were pivotal in identifying the ectopic gallbladder adherent to the left hepatic lobe. Laparoscopic cholecystectomy successfully resolved symptoms despite anatomical complexity, with postoperative pathology confirming absence of stones, sludge, or inflammation. The case highlights the necessity of advanced preoperative imaging
- Citation: Wu JR, Wang CC, Li BY, Li JH, Zhang T, Li ZY. Concomitant functional gallbladder disorder and left-sided gallbladder: A case report. World J Gastrointest Endosc 2025; 17(7): 107059
- URL: https://www.wjgnet.com/1948-5190/full/v17/i7/107059.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i7.107059
The gallbladder is typically located in the gallbladder fossa on the posterior aspect of the right lobe of the liver. When the gallbladder is found in other locations, it is defined as ectopic. The incidence of ectopic gallbladder is approximately 0.1% to 0.7%[1]. The main positional variations include: (1) Under the left liver lobe; (2) Intrahepatic; (3) Transverse; (4) Retro
The presence of an ectopic gallbladder, particularly in cases where it is left-sided, can complicate both diagnosis and management. The abnormal positioning of the gallbladder may contribute to motility dysfunction, potentially leading to functional gallbladder disorder (FGBD). FGBD is characterized by biliary pain in patients with an intact gallbladder and the absence of stones or sludge[4]. The prevalence of FGBD is approximately 8% in men and 21% in women[5]. FGBD is now listed as an indication for cholecystectomy in 10%-20% of adults[6], although it is rarely diagnosed outside the United States[7].
To date, there have been no reported cases of concomitant FGBD and left-sided gallbladder. Both conditions can cause abdominal pain, making it difficult to differentiate them from other diseases. Additionally, due to the anatomical ectopia of the gallbladder, surgical challenges may arise during cholecystectomy, potentially resulting in injury to the bile ducts or blood vessels. Therefore, this case report aimed to provide a reference and insights for the diagnosis and treatment concomitant FGBD and left-sided gallbladder.
A 73-year-old woman presented with intermittent epigastric colicky pain for over 20 years, without any other associated symptoms.
The patient had experienced intermittent epigastric colicky pain for more than two decades.
The patient had a history of well-controlled hypertension for 5 years and no prior surgical interventions.
No special personal or family history of diseases was mentioned by the patient.
Mild tenderness was noted in the upper abdomen. No rebound tenderness was found. No jaundice was observed in the skin or sclera.
Laboratory tests showed normal levels of inflammatory markers, liver enzymes, conjugated bilirubin, and amylase/lipase.
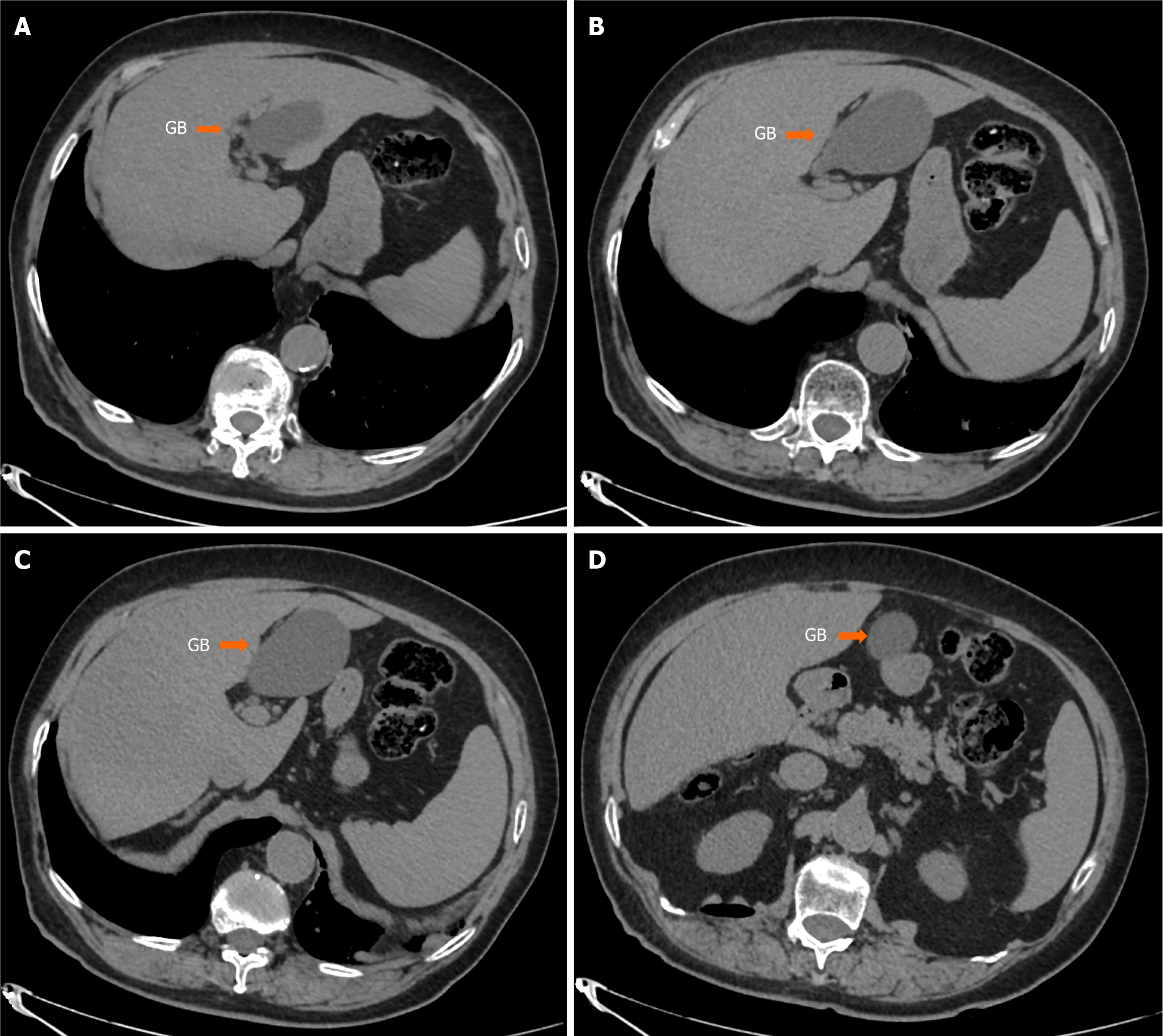
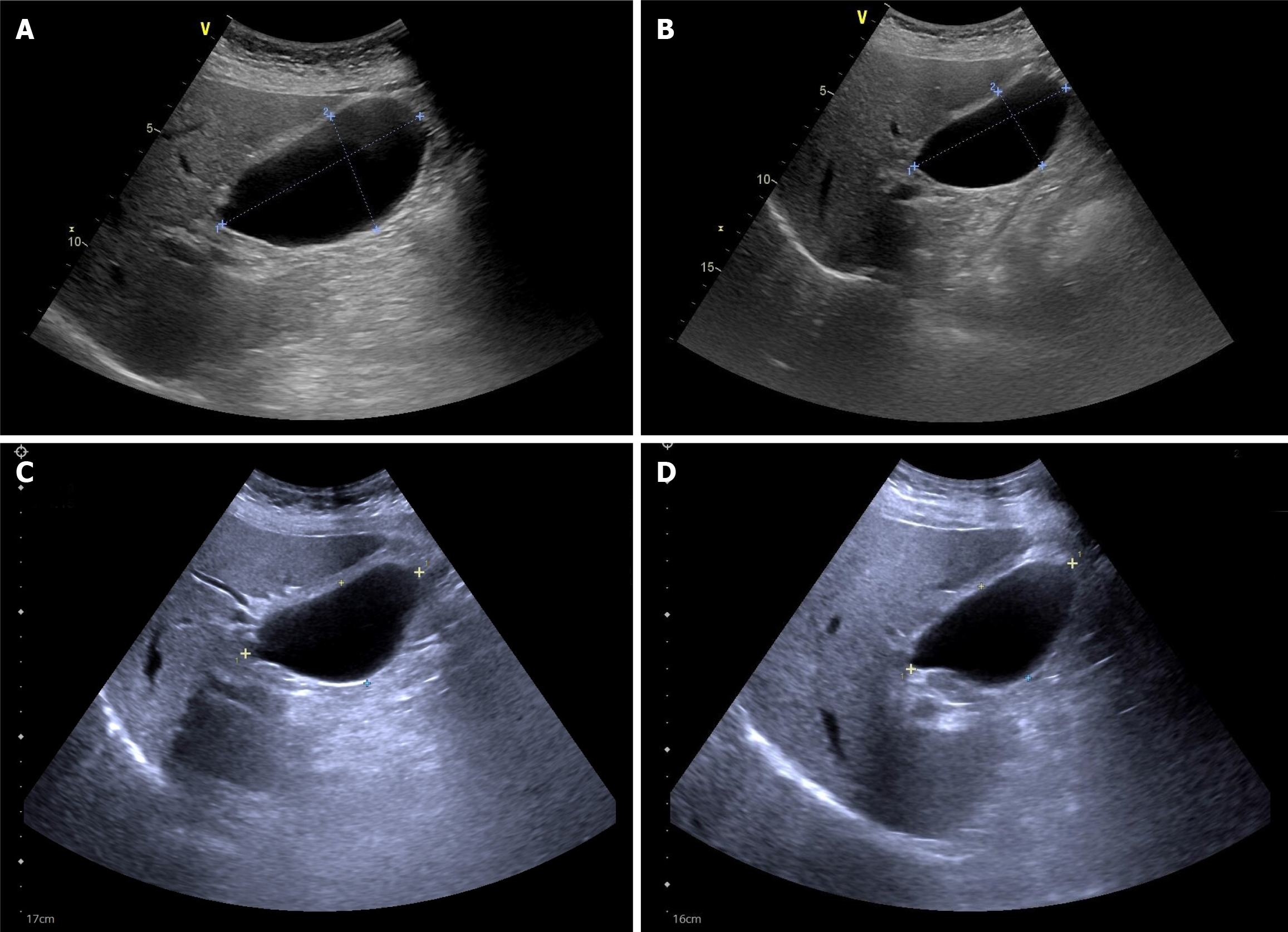
Computed tomography (CT scan showed that the gallbladder was located below the ligamentum teres hepatis, with a suspected attachment to the left lobe of the liver (Figure 1). Abdominal ultrasonography revealed no abnormalities in the liver, bile ducts, gallbladder, pancreas, or spleen. Endoscopic ultrasound (EUS) revealed chronic superficial gastritis, but no gallstones or extrahepatic biliary dilation was detected. Fatty meal-stimulated, ultrasound-guided gallbladder emp
The patient was diagnosed with FGBD and left-sided ectopic gallbladder.
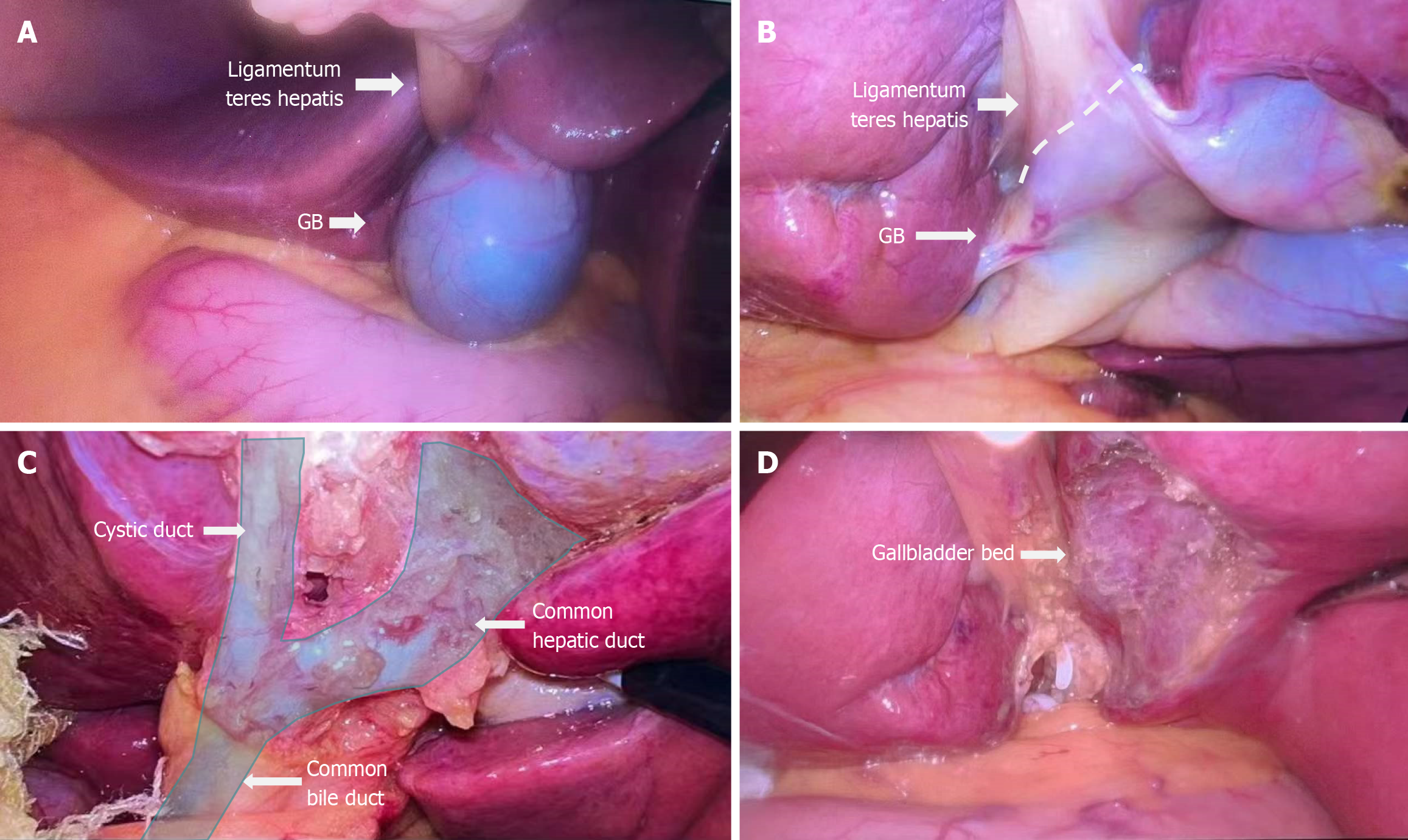
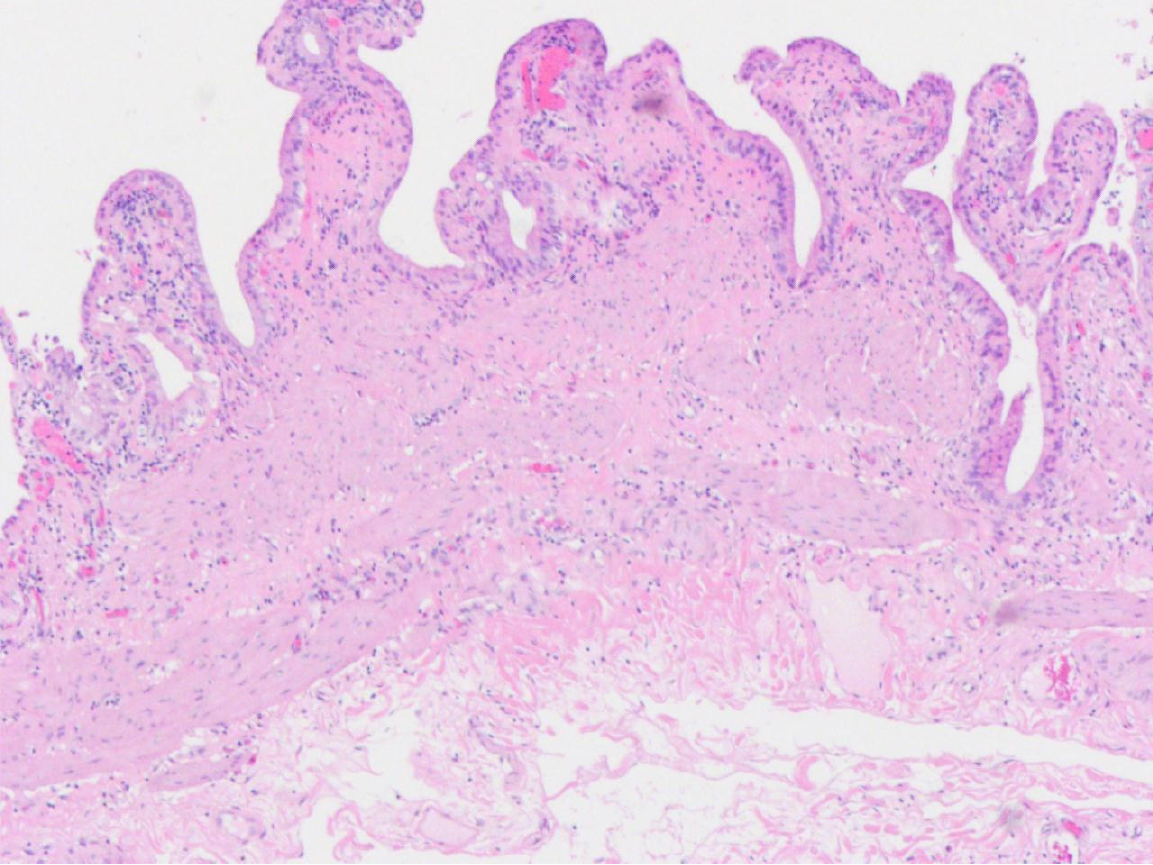
Considering the presence of FGBD and potential gallbladder ectopia, laparoscopic cholecystectomy was performed. Intraoperatively, the majority of the gallbladder was found adhering to the left lateral lobe of the liver, with a small portion attached to the ligamentum teres hepatis. The common hepatic duct and common bile duct were located below the ligamentum teres hepatis (Figure 3). Following the surgery, an anatomical examination of the excised gallbladder revealed dark green bile with a uniform texture. No stones or sludge were observed, and the pathological report in
The patient was discharged on the fifth postoperative day with significant relief of abdominal pain. After three months of follow-up, the patient's symptoms completely resolved (Supplementary Figure 1).
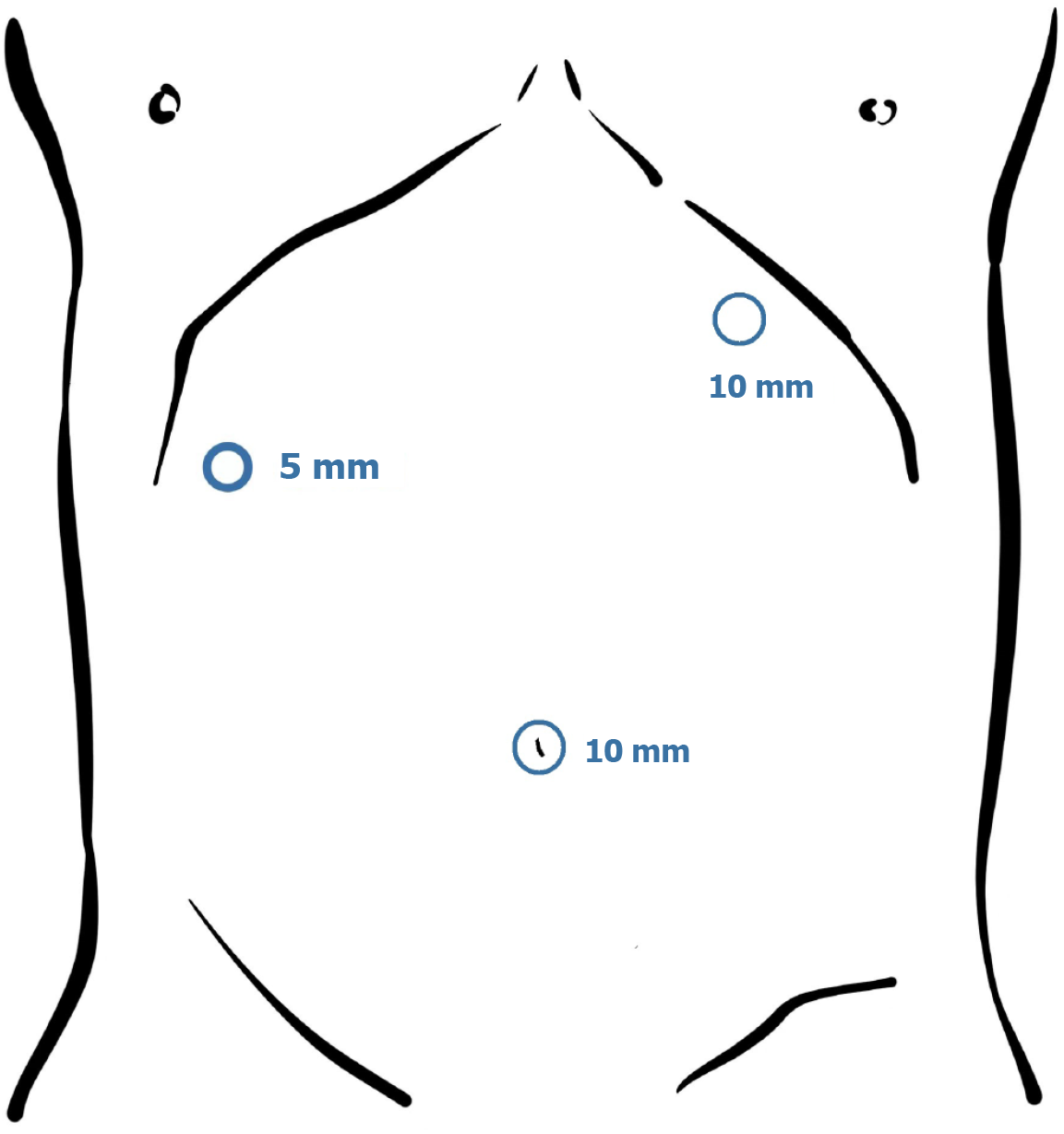
The incidence of variations in the cystic duct in patients with ectopic gallbladders ranges from approximately 18% to 23%[8]. To avoid inadvertent injury during surgery, several important considerations should be taken into account during the perioperative management of such patients: (1) Preoperative imaging should be used to assess for any cystic duct variations, as this is crucial in preventing bile duct injury during the surgical procedure; (2) Once laparoscopic access is established, if an ectopic gallbladder is identified, the position of the trocar should be adjusted promptly and flexibly to ensure the surgeon can comfortably and efficiently access the target area (Figure 5); and (3) The anatomy of the gall
In our case, a gallbladder emptying test using ultrasound after fatty meal stimulation was applied to assess gallbladder motility. Although this non-invasive test is valuable and practical in clinical settings, its diagnostic accuracy remains limited due to the lack of standardized protocols regarding timing, meal composition, and criteria for abnormal con
Additionally, functional gallbladder disease can also cause abdominal pain, which may arise from increased gall
Furthermore, the postoperative pathological examination did not reveal any definitive abnormalities. Therefore, further research is needed to investigate whether there are neurologically related functional disorders in the patient's gallbladder.
We report the first case of FGBD combined with a left-sided gallbladder. Up till now, there has been limited experience in the diagnosis and treatment of such cases. We believe that such patients often seek medical attention due to upper abdominal pain. Therefore, before considering the possibility of FGBD and gallbladder ectopia, it is crucial to rule out other abdominal organ diseases that may cause pain, such as upper gastrointestinal ulcers or perforations. Furthermore, it is essential to develop appropriate preoperative plans to address different variations that may occur during surgery to minimize the risk of surgical-related injury to the bile ducts and blood vessels. Thus, doctors should make the best use of imaging examinations to recognize variations in the gallbladder, cystic duct, and extrahepatic bile ducts preoperatively. Recommended examinations include magnetic resonance pancreatography, ERCP, and CT, among others. Lastly, high-resolution laparoscopy can provide clear visualization of anatomical abnormalities in the patient. Therefore, laparoscopic surgery should be considered a feasible option whenever possible. However, blind puncture must be avoided to mini
| 1. | Guerin JB, Venkatesh SK, Roberts LR. Ectopic Gallbladder. Clin Gastroenterol Hepatol. 2015;13:e69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Ben Ismail I, Zenaidi H, Sghaier M, Rebii S, Zoghlami A. Cholecystitis in a midline gallbladder: A rare ectopic location. Int J Surg Case Rep. 2022;93:106969. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 3. | Southam JA. Left-sided gallbladder:: calculous cholecystitis with situs inversus. Ann Surg. 1975;182:135-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Cotton PB, Elta GH, Carter CR, Pasricha PJ, Corazziari ES. Rome IV. Gallbladder and Sphincter of Oddi Disorders. Gastroenterology. 2016;150:1420-1429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 125] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 5. | Croteau DI. Functional gallbladder disorder: an increasingly common diagnosis. Am Fam Physician. 2014;89:779-784. [PubMed] |
| 6. | Bielefeldt K. The rising tide of cholecystectomy for biliary dyskinesia. Aliment Pharmacol Ther. 2013;37:98-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Preston JF, Diggs BS, Dolan JP, Gilbert EW, Schein M, Hunter JG. Biliary dyskinesia: a surgical disease rarely found outside the United States. Am J Surg. 2015;209:799-803; discussion 803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Wu YH, Liu ZS, Mrikhi R, Ai ZL, Sun Q, Bangoura G, Qian Q, Jiang CQ. Anatomical variations of the cystic duct: two case reports. World J Gastroenterol. 2008;14:155-157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Velanovich V. Biliary dyskinesia and biliary crystals: a prospective study. Am Surg. 1997;63:69-74. [PubMed] |
| 10. | Brugge WR, Brand DL, Atkins HL, Lane BP, Abel WG. Gallbladder dyskinesia in chronic acalculous cholecystitis. Dig Dis Sci. 1986;31:461-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 50] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Sharma BC, Agarwal DK, Dhiman RK, Baijal SS, Choudhuri G, Saraswat VA. Bile lithogenicity and gallbladder emptying in patients with microlithiasis: effect of bile acid therapy. Gastroenterology. 1998;115:124-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Ruffolo TA, Sherman S, Lehman GA, Hawes RH. Gallbladder ejection fraction and its relationship to sphincter of Oddi dysfunction. Dig Dis Sci. 1994;39:289-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 33] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/