Published online Jul 16, 2025. doi: 10.4253/wjge.v17.i7.105773
Revised: April 2, 2025
Accepted: June 7, 2025
Published online: July 16, 2025
Processing time: 153 Days and 1.1 Hours
Air embolism (AE) is a rare but potentially fatal complication of intestinal endoscopy (IE).
Herein, we report the case of an 18-year-old woman who underwent a successful Kasai portoenterostomy (KPE) for biliary atresia but died of AE during intraoperative IE for stone removal at the portoenterostomy site. Our review of the English literature identified only four similar cases of fatal AE during IE in patients undergoing KPE. The common clinical setting in the five patients, including our case, was high-pressure air insufflation into the blind closed afferent loop of the KPE to secure visibility. We hypothesize that the highly pre
Meticulous performance of IE, especially on the KPE blind loop, is warranted owing to the risk of AE.
Core Tip: Low-pressure CO2 insufflation instead of high-pressure air insufflation is more suitable during intestinal endoscopy in patients with Kasai portoenterostomy to prevent fatal air embolism.
- Citation: Shin SY, Yeon HJ, Lee SO, Lee JR, Leem G, Han SJ. Fatal air embolism during intestinal endoscopy in Kasai portoenterostomy for biliary atresia: A case report. World J Gastrointest Endosc 2025; 17(7): 105773
- URL: https://www.wjgnet.com/1948-5190/full/v17/i7/105773.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i7.105773
Air embolism (AE) during intestinal endoscopy (IE) is rare. Small AEs, if absorbed spontaneously, are subclinical with no adverse outcomes. However, large amounts of air infused into the blood circulation may be fatal due to AE. The first case of fatal AE during IE was reported in 1988 in an infant who had previously undergone Kasai portoenterostomy (KPE) for biliary atresia (BA)[1]. To date, three more cases of KPE with AE, with two of them being fatal, have been reported under a similar endoscopic study setting as in the first case[2-4]. We recently encountered a case of fatal AE during an IE examination in an 18-year-old woman with a history of successful KPE. Unfortunately, a massive AE during intraoperative IE resulted in her sudden and unexpected death.
The purpose of this report is to share the experience of contending with a fatal AE occurring during IE in patients who have undergone KPE and propose a hypothesis regarding the mechanism by which massive AE may occur in such patients.
The patient presented with jaundice as the chief complaint.
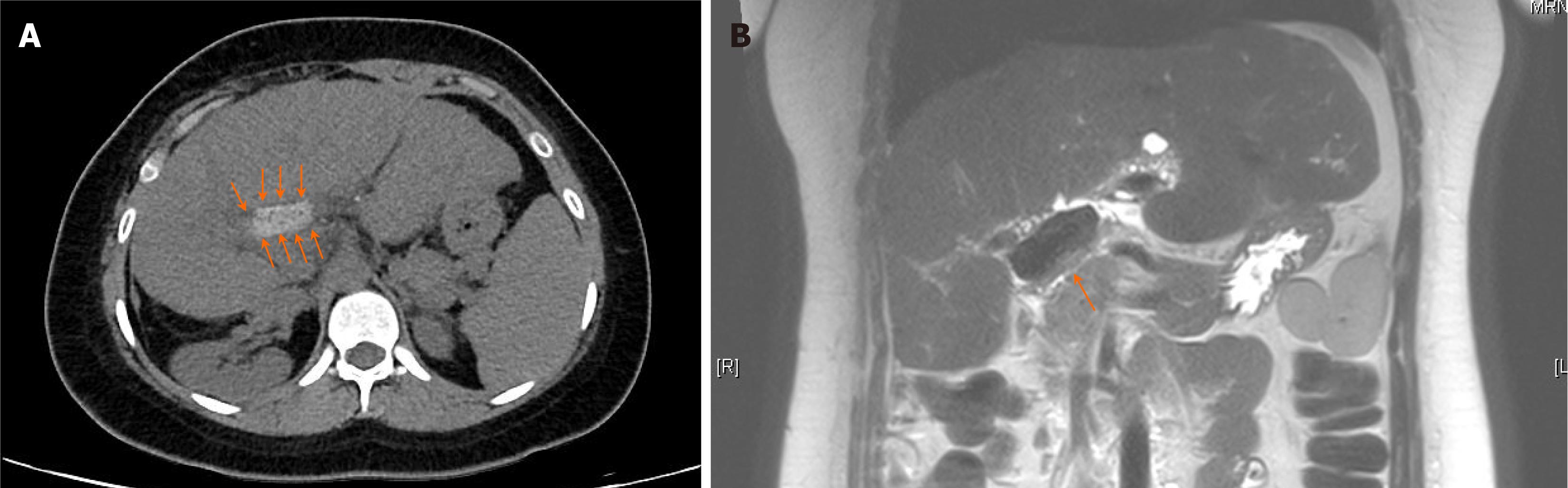
An 18-year-old woman was transferred to our hospital after 7 days of admission at a local hospital for acute cholangitis and hepatic duct stone. She was originally diagnosed with BA at 43 days of age and underwent KPE, which was performed by the corresponding author. After KPE, complete disappearance of the jaundice and gradual improvement in the hepatic fibrosis score with eventual normalization were noted. She was followed up at half-year intervals at the outpatient clinic of our hospital with medication (ursodeoxycholic acid, 3-400 mg/day), during which, cholangitis was not noted. However, an abdominal computed tomography performed at the local hospital before transfer showed a hyperdense lesion in the hepatic hilum, suggesting bile sludge or stone (Figure 1A).
Agitated saline transthoracic contrast echocardiography for intrapulmonary or intracardiac shunt showed the injected microbubbles filling the left atrium and ventricle of the heart within 7-8 heartbeats after intravenous injection of agitated saline, suggesting a minimal non-pathological intrapulmonary shunt. During the follow-up for BA at our hospital, serial imaging studies, including abdominal ultrasonography and magnetic resonance imaging (MRI), revealed progressive atrophic changes in the right lobe of the liver with compensatory hypertrophy of the left hepatic lobe; additionally, the formation of multiple tiny intrahepatic cysts without abnormal shadows suggestive of bile plugs or stone formation were noted.
Following admission to our hospital for suspected acute cholangitis with a stone in the hepatic hilum, abdominal MRI revealed a T2 low-signal intensity lesion at the KPE site (Figure 1B), suspected to be a stone or sludge lump. KPE site stones or sludge were inferred to be the likely causes of the cholangitis.
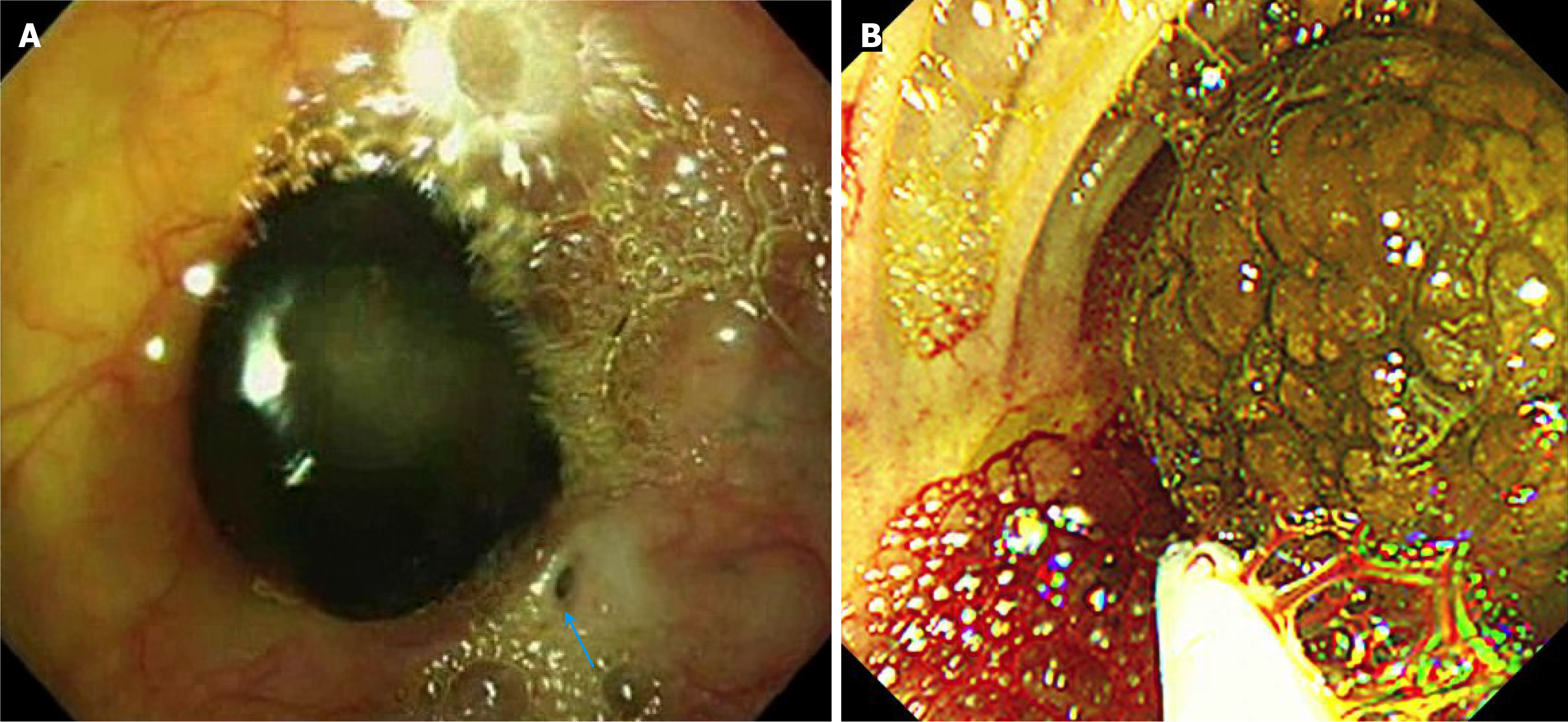
The final diagnosis was biliary stone at KPE site.
Following treatment for cholangitis with broad-spectrum antibiotics, an attempt at percutaneous transhepatic biliary drainage for removal of the stone failed owing to lack of ductal dilatation on sonography. Therefore, we decided to remove the stone from the KPE via an intraoperative endoscopy. After adhesiolysis of the subhepatic space, the afferent blind jejunal loop of the KPE was identified, and a small jejunotomy was performed. A flexible intestinal endoscope (GIF-Q260, 9.2 mm; Olympus, Tokyo, Japan) was inserted into the jejunotomy site and slowly advanced to the blind end of the KPE site while insufflating air. During the procedure, no leak of insufflated air from the jejunotomy site was observed as the diameter of the endoscope fit the size of the jejunotomy opening perfectly. IE revealed a large, thick, yellow bile sludge-like lump hanging from the KPE site, which was easily broken during endoscopic removal (Figure 2).
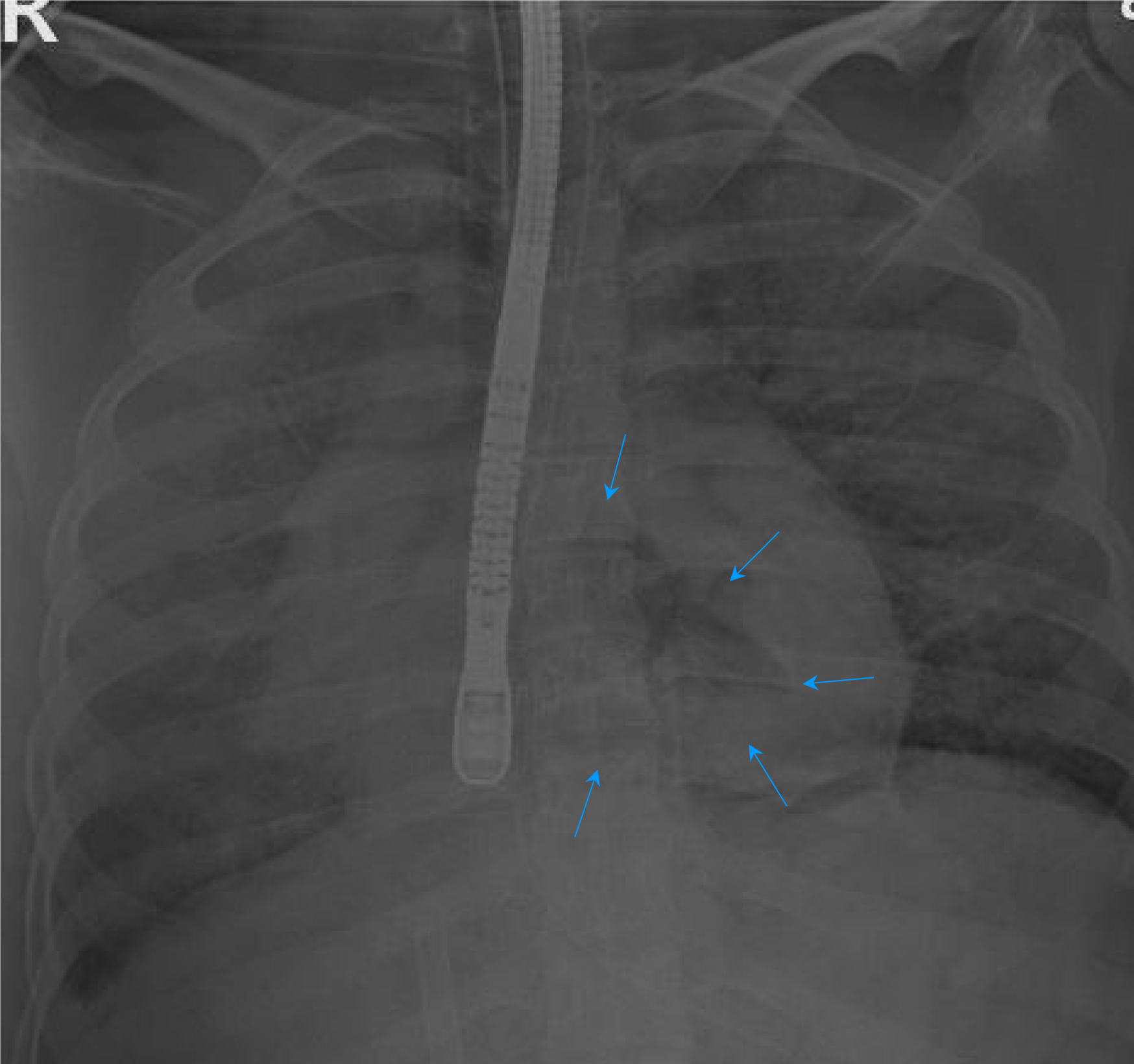
Approximately 3 minutes after starting the endoscopic procedure, end-tidal CO2 was suddenly undetectable, and the electroencephalography wave on the anesthetic depth monitor flattened. The patient’s heart rate changed from a normal sinus rhythm to severe bradycardia and asystole, the blood pressure suddenly dropped, and oxygen saturation was not measured. Rapid cardiopulmonary resuscitation, including chest compressions and repeated administration of epinephrine and vasopressin, was initiated. However, immediately after two cycles of cardiac compression and epinephrine administration, uncontrollable frothy pink bleeding from the endotracheal tube was noted. As the patient had been previously healthy, no intraoperative difficulties such as bleeding had been anticipated. We had inserted only two large-bore peripheral intravenous catheters for anesthesia. Anesthesiologists attempted to insert a central venous catheter through the internal jugular vein for proper resuscitation; however, no vessels were detected on ultrasonographic examination. Therefore, femoral venous cannulation was performed, and air bubbles were noted in the blood withdrawn from the venous cannula. Intraoperative transesophageal echocardiography confirmed the presence of a large amount of air in all four heart chambers. Simple chest radiography also showed shadows of entrapped air in the cardiac chambers (Figure 3). Subsequently, venoarterial extracorporeal membrane oxygenation was successfully applied through the right femoral vessels; however, this took approximately 30 minutes because of the collapsed vessels and an unstable surgical field due to continuous chest compression.
Despite successful extracorporeal membrane oxygenation, progression of the patient’s condition to multiple organ failure following no restoration of vital signs led us to declare the patient dead 5 hours after cardiac arrest. Although recommended, autopsy was not performed on account of her parents’ refusal (Table 1).
| Timeline | Patient’s course |
| HOD 1 | Admission for jaundice and stone at KPE site |
| HOD 6 | MRCP |
| HOD 11 | Attempted PTBD, but the procedure failed due to the patient's uncooperativeness |
| HOD 16, 08:40 AM | Operation starts |
| 12:00 PM | Intraoperative endoscopy insertion |
| 12:03 PM | Arrhythmia, hypotension, bradycardia |
| 12:10 PM | Asystole, CPR start |
| 13:07 PM | ECMO insertion, compression stop |
| 15:15 PM | Operation end, the patient was sent to ICU |
| 17:10 PM | The patient expired. |
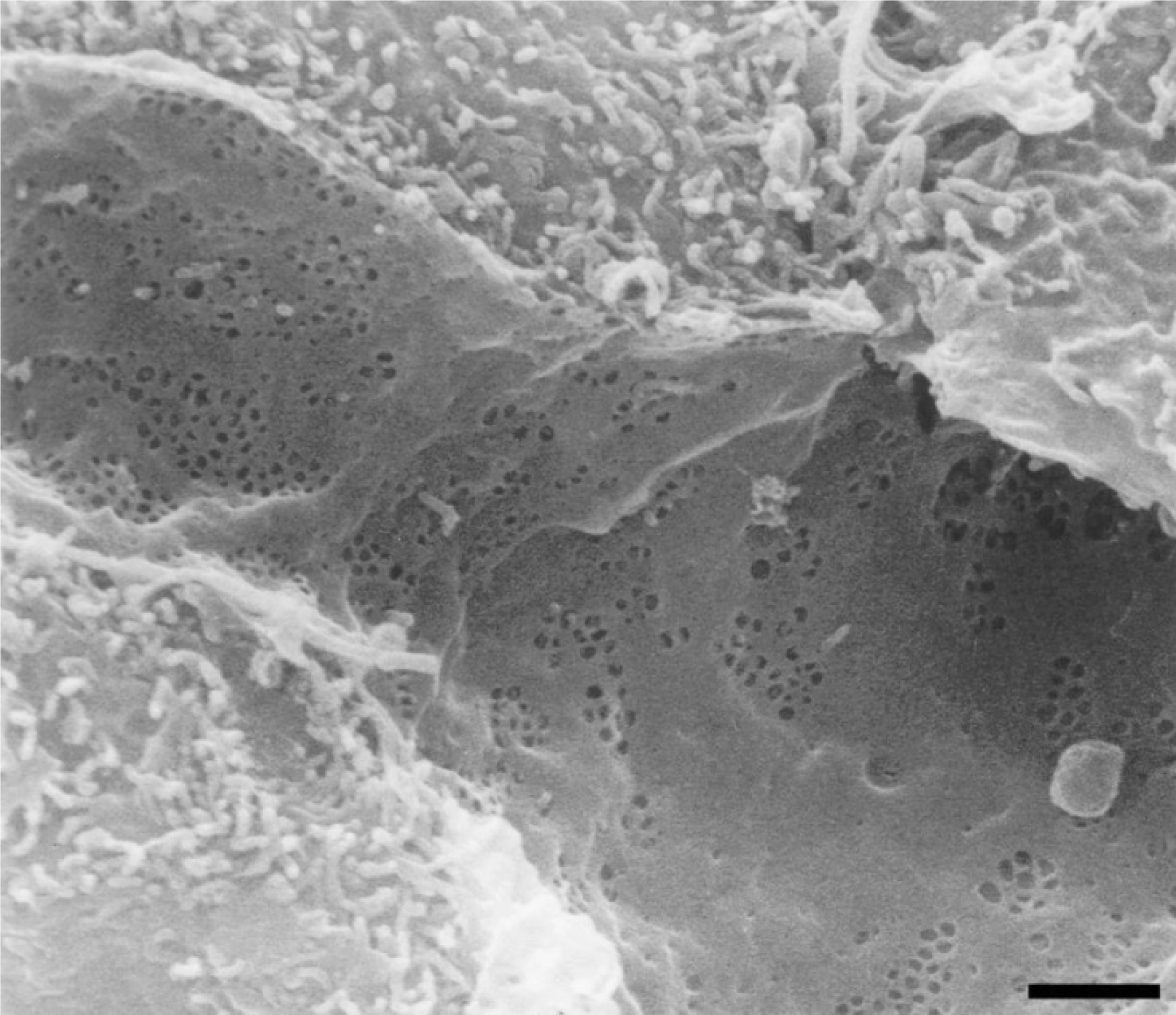
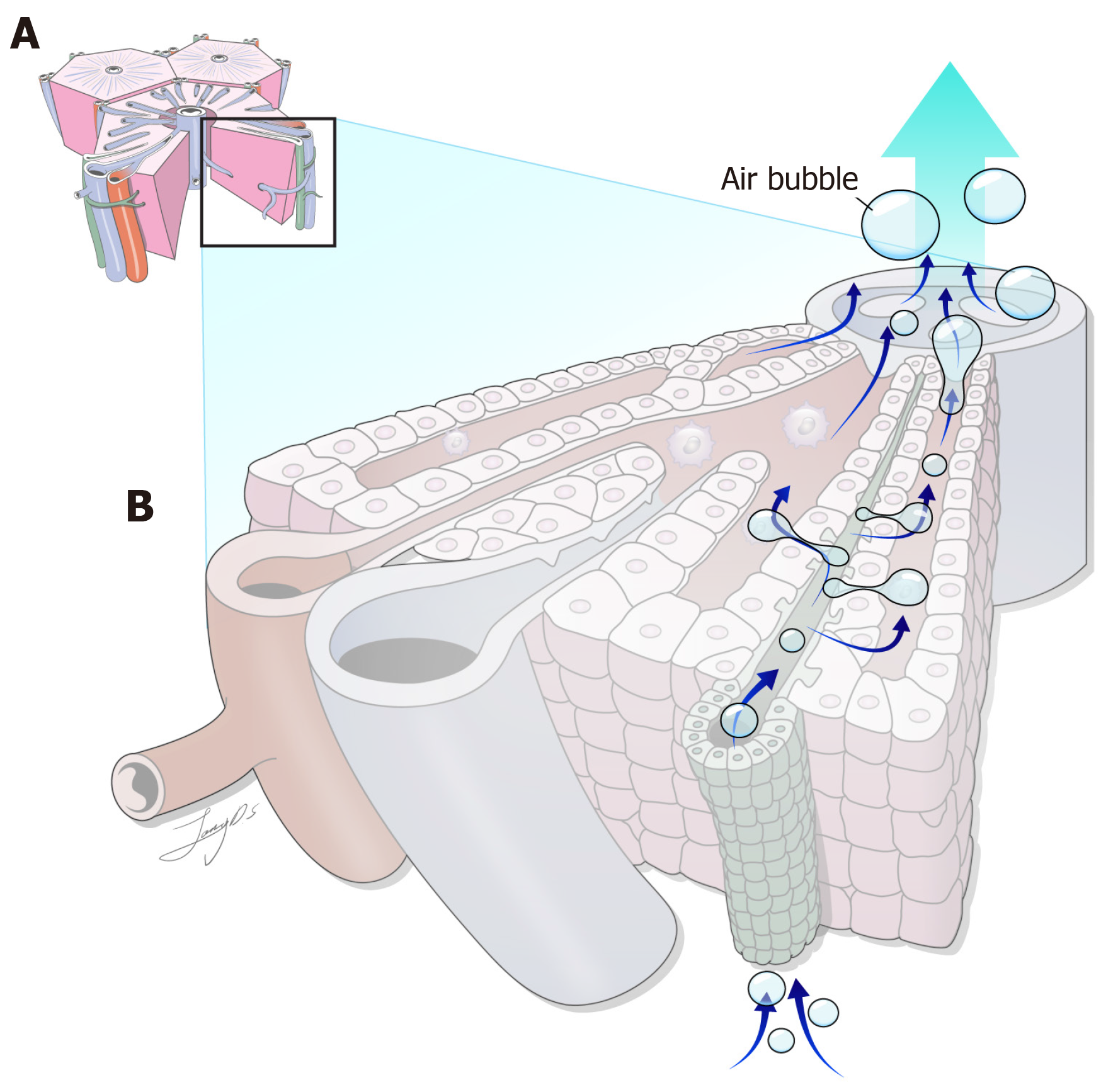
AE during IE is rare but fatal. In a survey of the members of the American Society for Gastrointestinal Endoscopy in 1976[5], no episodes of AE were found in 211410 IE procedures. According to a systematic review of the PubMed database on reported AE, 41 cases of AE during IE were identified in the English literature up to 2013[6]. The first case of AE during IE was reported in 1988 by Lowdon and Tidmore[1], involving a 4-month-old infant with a history of KPE for BA who died from fatal AE during intraoperative endoscopic exploration of the afferent loop of KPE. Since then, three additional cases of fatal AE in patients with KPE have been reported in the English literature (Table 2)[1-4]. Several conditions must be fulfilled for AE to occur during an IE. For air embolization to occur, air must pass through the gap in the physical barrier between the intestine and blood vessels. Moreover, there must be an interruption in the air-inflated intestine or bile duct barrier[3]. AE is more frequently observed during endoscopic exploration of the biliary system, such as endoscopic retrograde cholangiopancreatography, than during other intestinal endoscopic procedures[6]. The microscopic anatomy of the sinusoidal structure of the liver is critical in the occurrence of AE. Liver sinusoids comprise liver sinusoidal endothelial cells (LSECs) and are distinct from other capillaries in the body because of their open pores characterized by the absence of both a diaphragm and basal lamina beneath the endothelial layer (Figure 4). LSEC crucially regulates the exchange of macromolecules, solutes, and fluids between blood and surrounding tissues, such as bile canaliculi, through these fenestrae[7]. When high-pressure air is insufflated into a closed blind loop during IE in patients with KPE, air enters the bile canaliculi, passes through these tiny fenestrae in the LSEC, and easily enters the circulating bloodstream of the venous system, potentially leading to fatal AE (Figure 5). Next, air in the venous system can enter the systemic circulation through several mechanisms, including intracardiac or intrapulmonary shunting, or incomplete filtration of the intrapulmonary vessels, such as a paradoxical shunt[8,9]. The patient in this case also had a minimal intrapulmonary shunt, which could have acted as a pathway for air in the venous system to enter systemic circulation. In patients with a history of KPE, IE to explore the biliary tract can only be performed through the afferent blind loop of the Roux-en-Y limb. This approach can result in higher-pressure air insufflation compared to other endoscopic procedures, which may easily lead to AE during IE[10].
| Ref. | Age | Indication | Endoscopic entry | Air insufflation to closed loop | Time to arrest (minutes) | Paradoxical embolism | Result |
| Lowdon and Tidmore[1], 1988 | 4 months | Cholangitis | Enterotomy of A-loop | Yes | 5 | Yes | Died (autopsy) |
| Desmond and MacMahon[2], 1990[2] | 10 years | Stone of KPE site | Enterotomy of A-loop | Yes | 10 | Yes | Died (autopsy) |
| Park et al[3], 2010 | 17 years | Intestinal bleeding | Enterotomy of A-loop | Yes | Immediately | Yes | Survived |
| Pujari et al[4], 2012 | 5 years | Intestinal bleeding | Enterotomy of A-loop | Yes | 1 | Yes | Died (no autopsy) |
| 2023 (present case) | 18 years | Stone at KPE site | Enterotomy of A-loop | Yes | 3 | Yes | Died (no autopsy) |
Therefore, to prevent fatal AE we recommend using low-pressure CO2 insufflation instead of air insufflation through a blind afferent loop during IE in patients with hepatobiliary disease, such as those who have undergone biliary duct surgery, including biliary-enteric anastomosis, especially in patients with KPE.
AE during IE is rare but can be life-threatening. In this case, we hypothesized how severe AEs may develop in patients with KPE during IE. We recommend using low-pressure CO2 insufflation instead of high-pressure air insufflation during IE in patients with KPE to prevent fatal AE.
We thank MID (Medical Illustration & Design), a member of the Medical Research Support Services of Yonsei University College of Medicine, for providing excellent support with medical illustrations.
| 1. | Lowdon JD, Tidmore TL Jr. Fatal air embolism after gastrointestinal endoscopy. Anesthesiology. 1988;69:622-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 27] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Desmond PV, MacMahon RA. Fatal air embolism following endoscopy of a hepatic portoenterostomy. Endoscopy. 1990;22:236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Park YH, Kim HJ, Kim JT, Kim HS, Kim CS, Kim SD. Prolonged paradoxical air embolism during intraoperative intestinal endoscopy confirmed by transesophageal echocardiography -A case report-. Korean J Anesthesiol. 2010;58:560-564. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Pujari VS, Thomas MK, Bevinaguddaiah Y, Anandaswamy TC. Is intraoperative endoscopy safe in a child with Kasai procedure? J Anaesthesiol Clin Pharmacol. 2012;28:508-509. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Mandelstam P, Sugawa C, Silvis SE, Nebel OT, Rogers BH. Complications associated with esophagogastroduodenoscopy and with esophageal dilation. Gastrointest Endosc. 1976;23:16-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 124] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Donepudi S, Chavalitdhamrong D, Pu L, Draganov PV. Air embolism complicating gastrointestinal endoscopy: A systematic review. World J Gastrointest Endosc. 2013;5:359-365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 64] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (5)] |
| 7. | Braet F, Wisse E. Structural and functional aspects of liver sinusoidal endothelial cell fenestrae: a review. Comp Hepatol. 2002;1:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 539] [Cited by in RCA: 540] [Article Influence: 22.5] [Reference Citation Analysis (2)] |
| 8. | Hopkins WE, Waggoner AD, Barzilai B. Frequency and significance of intrapulmonary right-to-left shunting in end-stage hepatic disease. Am J Cardiol. 1992;70:516-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 123] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Sasaki T, Hasegawa T, Kimura T, Okada A, Mushiake S, Matsushita T. Development of intrapulmonary arteriovenous shunting in postoperative biliary atresia: evaluation by contrast-enhanced echocardiography. J Pediatr Surg. 2000;35:1647-1650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Yamamoto H. Be aware of the fatal risk of air embolism. Dig Endosc. 2014;26:23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/