Published online Feb 16, 2025. doi: 10.4253/wjge.v17.i2.101135
Revised: November 5, 2024
Accepted: January 11, 2025
Published online: February 16, 2025
Processing time: 159 Days and 18.1 Hours
Juvenile polyps (JPs) are non-neoplastic polyps. In adults, JPs present with hematochezia in only approximately half the patients and are often found incidentally during endoscopic screening. JPs have no mucosal fascia at the tip, and spontaneous shedding and massive gastrointestinal hemorrhage may occur. Thus, the JP bleeding detected in this case by extravascular contrast leakage on computed tomography scans and treated with endoscopic clipping is rare.
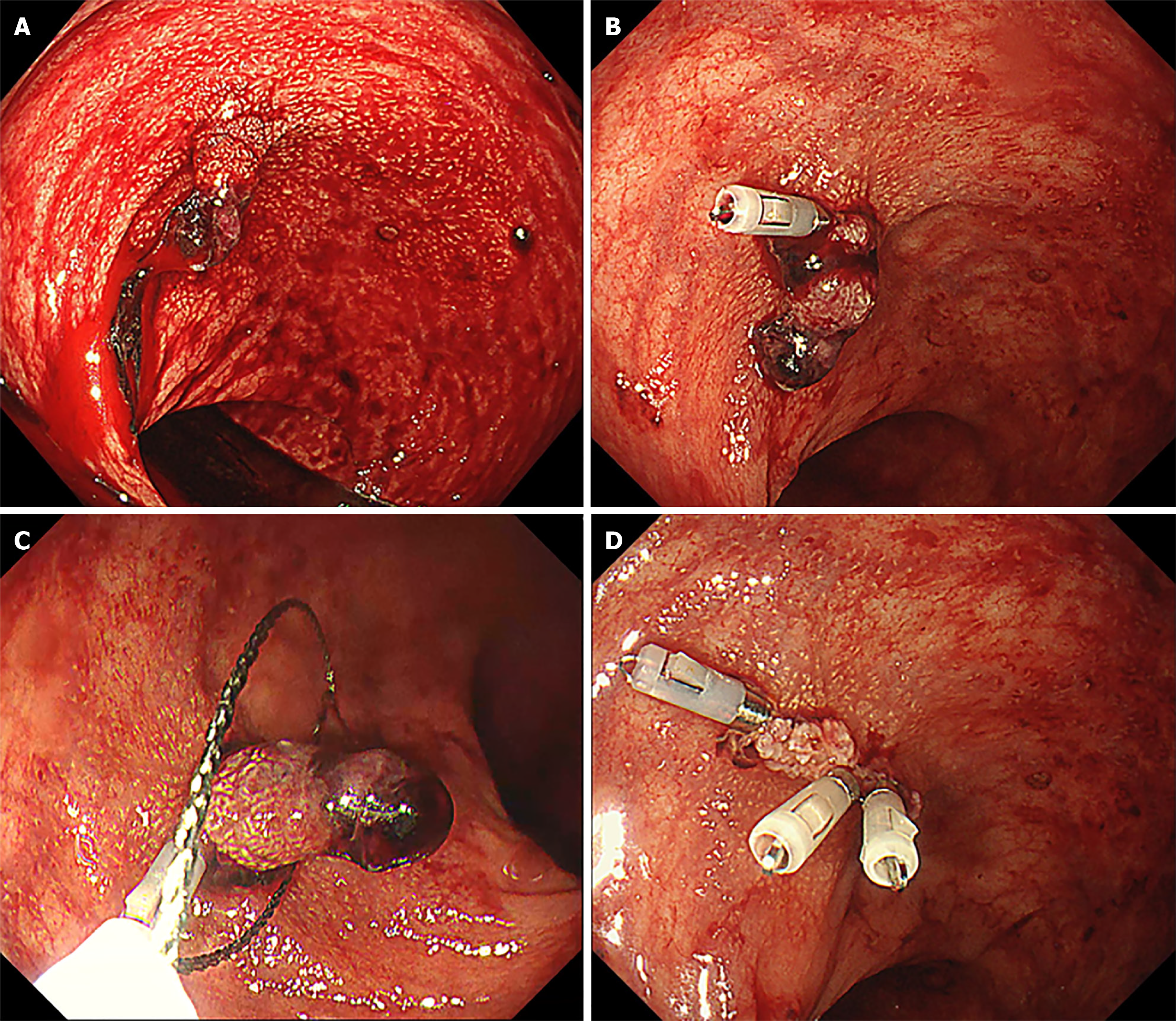
A previously healthy 31-year-old male patient presented with a 2-day history of bloody stools. Upon hospital arrival, rectal examination revealed fresh blood, and abdominal computed tomography scans showed extravascular contrast leakage from the lower rectum’s left-side wall. His blood pressure was slightly low at 104/62 mmHg. However, his pulse rate (69 bpm) and oxygen level (99% on room air) were within normal limits. Emergency endoscopy revealed a pedunculated lesion in the rectum covered by a non-neoplastic mucosal epithelium. No neo
There are no reports of adult JPs presenting with contrast extravasation where endoscopic hemostasis was successful, as in this case.
Core Tip: A 31-year-old male presented with hematochezia lasting for 2 days. computed tomography scans showed extravasation, and endoscopy was used to confirm and stop bleeding from the stem of a juvenile polyp (JP). Emergency endoscopy revealed persistent bleeding from the base of the polyp, and diagnostic polypectomy and hemostasis was performed. JPs are often detected with bloody stools. However, there have been no reports of JPs with active bleeding seen on computed tomography scans as extravasation. In this rare case, an endoscopic video showed persistent bleeding, and successful endoscopic hemostasis was achieved, and captured on video.
- Citation: Kataoka F, Nakanishi T, Araki H, Ichino S, Kamei M, Makino H, Nagao R, Asano T, Tagami A, Moriwaki H. Adult juvenile polyp bleeding detected by extravascular contrast leakage and treated with endoscopic clipping: A case report. World J Gastrointest Endosc 2025; 17(2): 101135
- URL: https://www.wjgnet.com/1948-5190/full/v17/i2/101135.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i2.101135
Juvenile polyps (JPs) are categorized as non-neoplastic polyps. Approximately 80%-90% of JPs are located in the sigmoid colon and rectum and are most common in children aged 3-10 years, although many adult cases have been reported[1,2]. In terms of the trigger for detection, most childhood cases were found to present with hematochezia, whereas in adults, hematochezia is reported in only approximately half of all cases and is often found incidentally during endoscopy screening[1,3,4]. As JPs have no mucosal fascia growth at the tip of the polyp, spontaneous shedding and massive gastrointestinal hemorrhage may occur[5]. However, according to our research, no such reports were found upon searching PubMed using the keywords “juvenile polyp,” “computed tomography,” and “extravascular leakage.” Thus, the JP bleeding detected in this case by extravascular leakage of contrast medium on computed tomography (CT) scans and treated with endoscopic clipping is rare.
A previously healthy 31-year-old male patient presented with a 2-day history of bloody stools.
He stayed home but then suffered from a large volume of fresh bloody stools and was referred to our hospital after visiting his family doctor.
He denied any personal history of illness.
There were no specific findings in his medical history or medications and no family history of JPs.
The patient’s vital signs were stable, with no obvious abnormalities in the physical examination; his abdomen was flat and soft, with no abdominal tenderness. Shifting dullness in the abdomen was negative. A large volume of red stools was reported.
At the time of presentation, the patient was not anemic and had a serum hemoglobin (Hb) level of 13.7 g/dL (normal range, 13.7-16.8 g/dL).
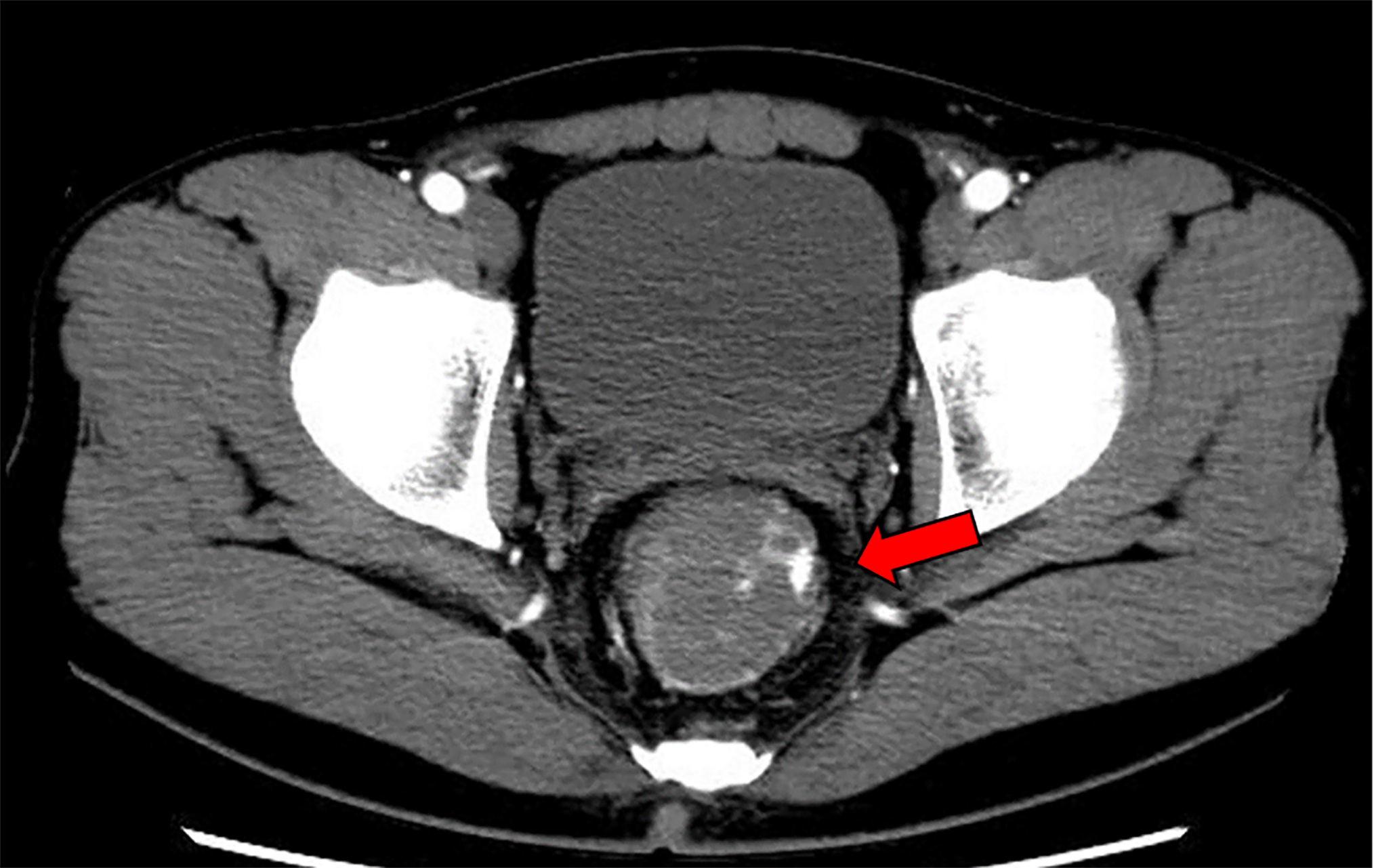
Contrast-enhanced abdominal CT scans revealed extravascular leakage of contrast medium from the left wall of the lower rectum (Figure 1).
The final diagnosis was JPs.
We performed an emergency colonoscopy and found a pedunculated polyp on the left wall of the lesion below the perito
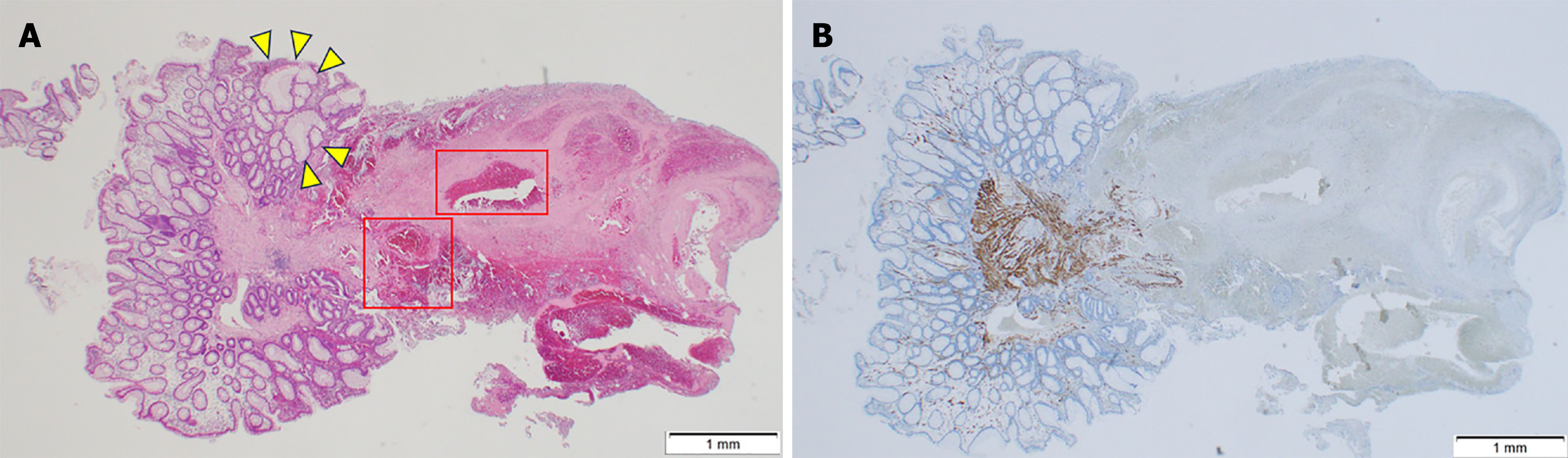
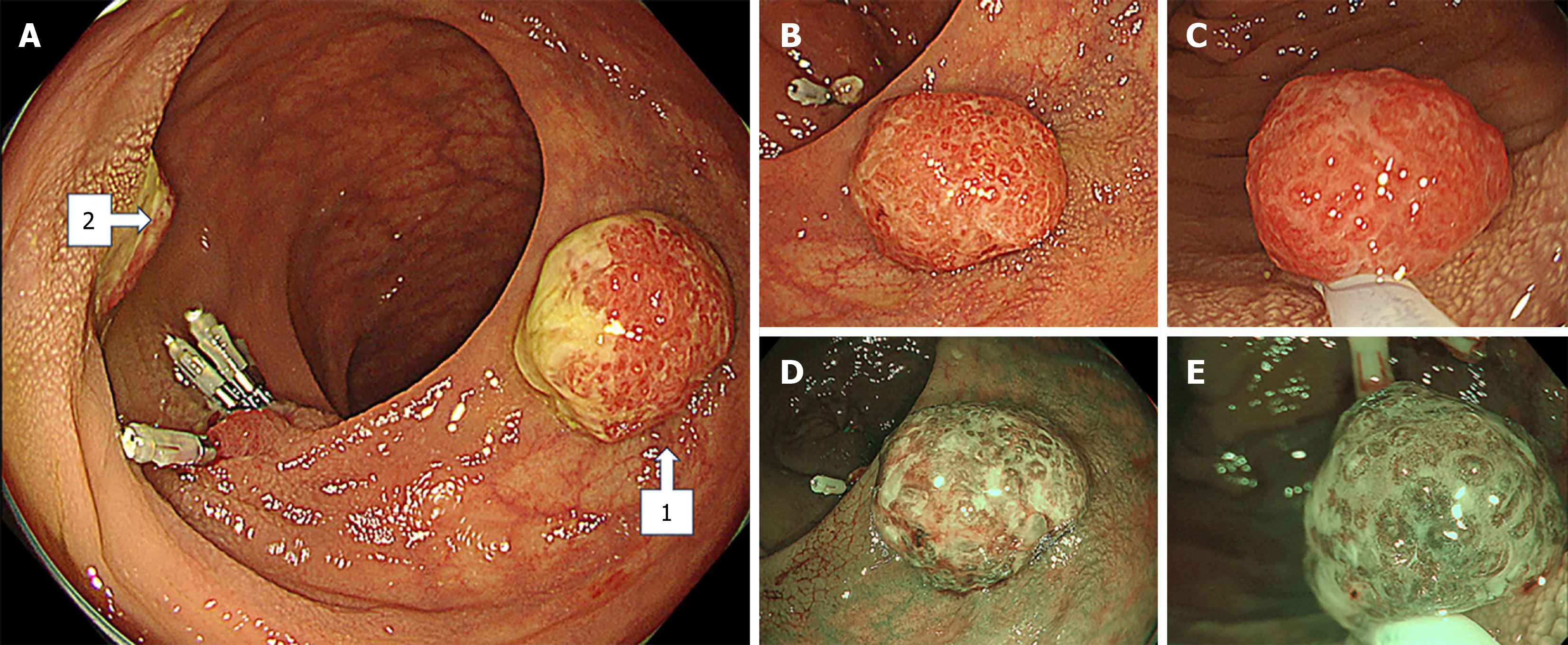
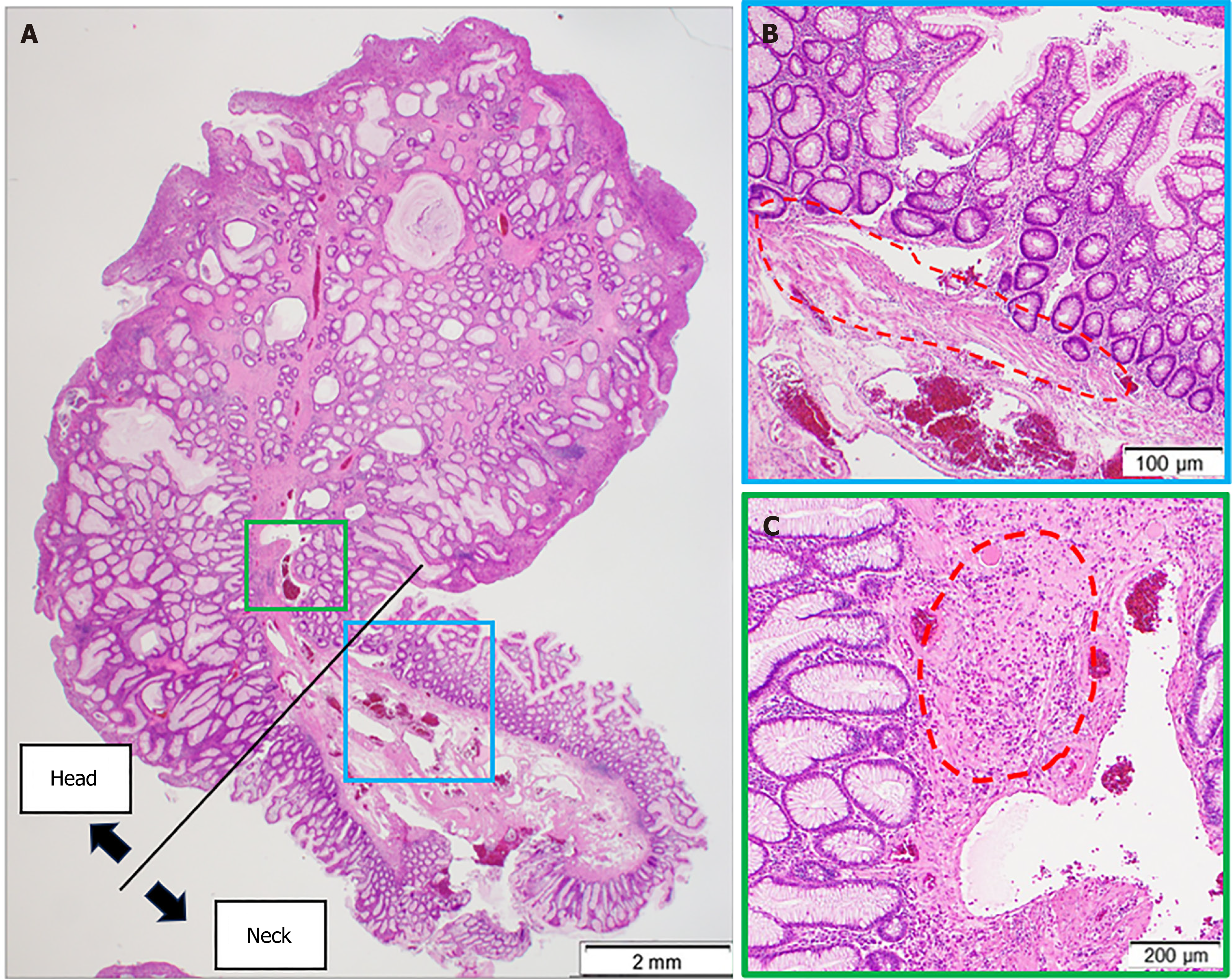
On the fourth day of hospitalization, the patient’s serum Hb level dropped to 10.4 g/dL, although no fresh bloody stools were observed. On the sixth day of hospitalization, we performed a total colonoscopy and found two semi-pedunculated polyps, approximately 15 mm in diameter, near the bleeding lesion in the rectum (Figure 3). The polyps were intensely erythematous, had smooth surfaces and erosions, and were moss-white in color. Narrow-band imaging revealed that the glands were dilated, with no irregular vessels or surface patterns, confirming diagnosis for the Japan narrow-band imaging expert team classification type 1 (Figure 4). As these polyps showed characteristic JP findings, we performed endoscopic mucosal resection. Histopathology revealed high inflammatory cell infiltrates and cystically dilated glandular formations filled with mucus. However, a lack of lamina muscularis mucosae in the head of the polyp further confirmed they were JPs (Figure 5). The patient showed favorable progress after the endoscopic procedure and was discharged on the seventh day of hospitalization. Subsequently, we performed an upper gastrointestinal endoscopy that revealed no polyps in the stomach. As the possibility of juvenile polyposis syndrome (JPS) could not be ruled out, we recommended an examination of the small intestine. However, the patient did not wish to undergo further examinations.
JPs were first described by Horrilleno et al[6] in 1957. As previously mentioned, most pediatric cases (under 10 years of age) present with hematochezia, whereas in adult cases, hematochezia is mainly detected incidentally by colonoscopy. Endoscopic features are described as pedunculated, with smooth or granular surfaces and reddish-colored polyps with slight irregularities. They often show erosions, mucous membranes, and hemorrhages[3]. Histological findings are characterized by cystically dilated glandular formations filled with mucus. The differential diagnoses of JPs on endoscopy include adenomas, familial adenomatous polyposis, and inflammatory polyps[2].
Colonic polyps are a rare cause of bloody stools. According to a large Japanese study on acute hematochezia, the most common cause of hematochezia was diverticular hemorrhage (63.6%), followed by ischemic enteritis (9.1%), and only 0.4% of cases were caused by colorectal polyps. The mechanism of hematochezia of JPs with stroma is considered as follows: Stromal polyps have large blood vessels inside[7], and JPs tend to shed spontaneously and bleed profusely because the mucosal muscle plate is not embedded in the polyp head. In the case presented herein, although the head of the polyp was already detached, a large arteriovenous vein was running from the tissue of the detached transected edge and a surrounding cystic duct with dilated glandular ducts. This suggested that the head of the stemmed JP had spontaneously detached and presented with active bleeding. The rarity of this case lies in the fact that hemorrhage due to JPs was first confirmed by extravascular leakage observed on a CT scan. Considering that the frequency of extravascular leakage on contrast CT scans for hematochezia evaluations is reported to be 22% and that the aforementioned colonic polyps are the cause of 0.4% of hematochezia, one can see how unusual it is that bleeding from a colonic polyp is detected by extravascular leakage of contrast media on CT[8]. Generally, contrast-enhanced CT scans can identify the source of bleeding if the bleeding is greater than 0.5 mL/minute[9]. In this case, the patient had experienced hematochezia for 2 days, indicating that the bleeding had persisted for at least 30 hours. Furthermore, by the fourth day after hospitalization, the patient’s Hb level had decreased by 3.3 g/dL. Considering the amount of bleeding detected by CT scans[9] and given that the patient weighed 60 kg, the total volume of blood loss was estimated to be approximately 1 L.
Finally, we discuss the association between JP and cancer. Cases of JPs are usually solitary. However, cases with multiple polyps require additional examination for JPS. Patients with JPS have a high risk of developing gastrointestinal cancers, especially gastric and colorectal cancers, with an estimated cumulative risk of 9%-68%. Therefore, routine surveillance is required for patients with JPS, considering the risk of cancer[10]. JPS is diagnosed in the presence of any of the following: More than five JPs in the colorectum, multiple JPs throughout the gastrointestinal tract, or any number of JPs, and a family history of JPS. However, a single JP is believed not to increase the risk of cancer[3]. Thus, gastrointestinal surveillance is typically considered unnecessary in the absence of a family history of JPS[4,11]. However, some case reports have described adenomas or adenocarcinomas on JPs. Giardiello et al[12] reported that multiple JPs or a family history of JPs increases the risk of colon neoplasia. Thus, total colonoscopy is recommended for these patients. In the present case, at least three JPs were identified, suggesting that routine surveillance will be necessary.
A limitation of this case is that the head of the hemorrhagic pedunculated lesion had auto-amputated, and we could not establish the complete polyp form. However, the histopathology of the stalk showed dilated glandular ducts, a finding consistent with JP histology.
Although JPs are often encountered during screening endoscopies, we believe that cases of active hemorrhage observed on CT scans, as in this case, are rare. JP is often characterized by hematochezia and sometimes induces hemorrhagic shock. However, there have been no previous reports of JP in adults presenting with contrast extravasation on CT scans and where endoscopic hemostasis was successfully performed for active bleeding, as in this very rare case.
| 1. | Dong J, Ma TS, Xu YH, Li P, Chen WY, Tu JF, Chen YW. Characteristics and potential malignancy of colorectal juvenile polyps in adults: a single-center retrospective study in China. BMC Gastroenterol. 2022;22:75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 2. | Popović M, Knežević A, Dolinaj Škopelja J, Đolai M. Juvenile polyp in adults. Acta Clin Croat. 2022;61:354-358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Vrakas S, Ignatova S, Karapiperis G, Kartsoli S, Karapiperis D. A juvenile polyp on screening colonoscopy. Autops Case Rep. 2023;13:e2021414. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Jelsig AM, Ousager LB, Brusgaard K, Qvist N. Juvenile Polyps in Denmark From 1995 to 2014. Dis Colon Rectum. 2016;59:751-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Kim DY, Bae JY, Ko KO, Cheon EJ, Lim JW, Song YH, Yoon JM. Juvenile Polyp associated with Hypovolemic Shock Due to Massive Lower Gastrointestinal Bleeding. Pediatr Gastroenterol Hepatol Nutr. 2019;22:613-618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Horrilleno EG, Eckert C, Ackerman LV. Polyps of the rectum and colon in children. Cancer. 1957;10:1210-1220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Dobrowolski S, Dobosz M, Babicki A, Głowacki J, Nałecz A. Blood supply of colorectal polyps correlates with risk of bleeding after colonoscopic polypectomy. Gastrointest Endosc. 2006;63:1004-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 68] [Article Influence: 3.4] [Reference Citation Analysis (1)] |
| 8. | Nagata N, Kobayashi K, Yamauchi A, Yamada A, Omori J, Ikeya T, Aoyama T, Tominaga N, Sato Y, Kishino T, Ishii N, Sawada T, Murata M, Takao A, Mizukami K, Kinjo K, Fujimori S, Uotani T, Fujita M, Sato H, Suzuki S, Narasaka T, Hayasaka J, Funabiki T, Kinjo Y, Mizuki A, Kiyotoki S, Mikami T, Gushima R, Fujii H, Fuyuno Y, Gunji N, Toya Y, Narimatsu K, Manabe N, Nagaike K, Kinjo T, Sumida Y, Funakoshi S, Kawagishi K, Matsuhashi T, Komaki Y, Miki K, Watanabe K, Fukuzawa M, Itoi T, Uemura N, Kawai T, Kaise M. Identifying Bleeding Etiologies by Endoscopy Affected Outcomes in 10,342 Cases With Hematochezia: CODE BLUE-J Study. Am J Gastroenterol. 2021;116:2222-2234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 9. | Kuhle WG, Sheiman RG. Detection of active colonic hemorrhage with use of helical CT: findings in a swine model. Radiology. 2003;228:743-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 153] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 10. | Matsumoto T, Umeno J, Jimbo K, Arai M, Iwama I, Kashida H, Kudo T, Koizumi K, Sato Y, Sekine S, Tanaka S, Tanakaya K, Tamura K, Hirata K, Fukahori S, Esaki M, Ishikawa H, Iwama T, Okazaki Y, Saito Y, Matsuura N, Mutoh M, Tomita N, Akiyama T, Yamamoto T, Ishida H, Nakayama Y. Clinical Guidelines for Diagnosis and Management of Juvenile Polyposis Syndrome in Children and Adults-Secondary Publication. J Anus Rectum Colon. 2023;7:115-125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 11. | Thakkar K, Alsarraj A, Fong E, Holub JL, Gilger MA, El Serag HB. Prevalence of colorectal polyps in pediatric colonoscopy. Dig Dis Sci. 2012;57:1050-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Giardiello FM, Hamilton SR, Kern SE, Offerhaus GJ, Green PA, Celano P, Krush AJ, Booker SV. Colorectal neoplasia in juvenile polyposis or juvenile polyps. Arch Dis Child. 1991;66:971-975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 134] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/