Published online Jan 16, 2025. doi: 10.4253/wjge.v17.i1.97840
Revised: December 19, 2024
Accepted: January 2, 2025
Published online: January 16, 2025
Processing time: 215 Days and 17.8 Hours
Endoscopic retrograde cholangiopancreatography is a challenging procedure involving bile duct cannulation. Despite the development of several cannulation devices, none have effectively facilitated the procedure.
To evaluate the efficacy of a recently developed catheter for bile duct cannulation.
We retrospectively examined 342 patients who underwent initial cholangiopancreatography. We compared the success rate of bile duct cannulation and the incidence of complications between the groups using existing and novel catheters.
The overall success rates of bile duct cannulation were 98.3% and 99.1% in the existing and novel catheter groups, respectively (P = 0.47). The bile duct cannulation rate using the standard technique was 73.0% and 82.1% in the existing and novel catheter groups, respectively (P = 0.042). Furthermore, when catheterization was performed by expert physicians, the bile duct cannulation rate was significantly higher in the novel catheter group (81.3%) than in the existing catheter group (65.2%) (P = 0.017). The incidence of difficult cannulation was also significantly lower in the novel catheter group (17.4%) than in the existing catheter group (33.0%) (P = 0.019).
The novel catheter improved the bile duct cannulation rate using the standard technique and reduced the frequency of difficult cannulation cases, valuable tool in endoscopic retrograde cholangiopancreatography procedures performed by experts.
Core Tip: The use of a novel contrast-enhanced catheter improved the bile duct cannulation rate when using the standard technique and reduced the frequency of cases with difficult cannulation. These advantages were particularly notable in procedures performed by experts. Further, its application by experts has shown promise in reducing the frequency of difficult cannulation, underscoring its utility in clinical practice.
- Citation: Kaneko T, Kida M, Kurosu T, Kitahara G, Koyama S, Nomura N, Tahara K, Kusano C. Outcomes of bile duct cannulation using a novel contrast-enhanced catheter: A single-center, retrospective cohort study. World J Gastrointest Endosc 2025; 17(1): 97840
- URL: https://www.wjgnet.com/1948-5190/full/v17/i1/97840.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i1.97840
Endoscopic retrograde cholangiopancreatography (ERCP) is useful for diagnosing and treating conditions affecting the biliopancreatic region[1-3]. ERCP is commonly used to manage diseases such as choledocholithiasis, obstructive jaundice, pancreaticobiliary malignancies, chronic pancreatitis, and biliary strictures. ERCP enables visualization of the biliary and pancreatic ducts and offers avenues for therapeutic interventions such as stone removal, stent placement, and tissue sampling for pathological examination. Notably, ERCP is a complex procedure involving several techniques, with selective bile duct cannulation being the initial and often challenging step. Selective bile duct cannulation is the first fundamental procedure to access the bile duct during ERCP. However, even experts can find it difficult to perform this procedure in some cases, with reports indicating a failure rate of approximately 5%-20% for selective bile duct cannulation in patients with a first papilla[4-7]. Difficulties in selective bile duct cannulation have been reported due to variations in patient anatomy, such as a parapapillary diverticulum or a specific papilla morphology[8-10] as well as differences in endoscopist skills[8-11]. Watanabe et al[10] focused on oral protrusion and difficulty in bile duct cannu
Various methods and devices have been developed to improve success rates of bile duct cannulation. The conventional contrast-guided cannulation has been widely used; however, in 1987, Siegel et al[12] reported the wire-guided cannulation (WGC) method using a guidewire (GW), which has now gained broad adoption in routine practice. In some cases, bile duct cannulation is difficult using only these standard methods. Therefore, various methods have been devised for such cases, including pre-cutting[13], the double- GW technique with a GW placed in the pancreatic duct[14], two devices in one-channel method[15], endoscopic ultrasound (EUS)-guided rendezvous technique[16], and various other bile duct cannulation methods.
Approximately 10% of patients undergoing ERCP experience incidental complications[17]. Post-ERCP pancreatitis (PEP) is the most fatal incidental complication of ERCP[18]. Repeated cannulation attempts increase the risk for PEP[19]. These findings underscore the importance of facilitating bile duct cannulation to improve its success rate and reduce accidental injuries such as PEP. Recently, a novel type of catheter for cholangiography has been introduced to the market. The catheter is soft and has a chamfered tip, which allows cannulation of the bile duct without stress on the bile duct and may facilitate the procedure. A previous study comparing sphincterotomes and contrast-enhanced catheters reported that WGC with sphincterotomes had a higher rate of selective bile duct cannulation and smaller incidence of PEP[20], whereas others reported that the rate of selective bile duct cannulation and the incidence of PEP was the same[21]. However, to the best of our knowledge, no study using the new catheter has been conducted. Therefore, this study aimed to retro
This single-center, retrospective cohort study was conducted at Kitasato University Medical Center in Japan. The study was performed in accordance with the Declaration of Helsinki and approved by our hospital’s Institutional Review Board, approval No. 2023011. All participants provided written informed consent before the procedure.
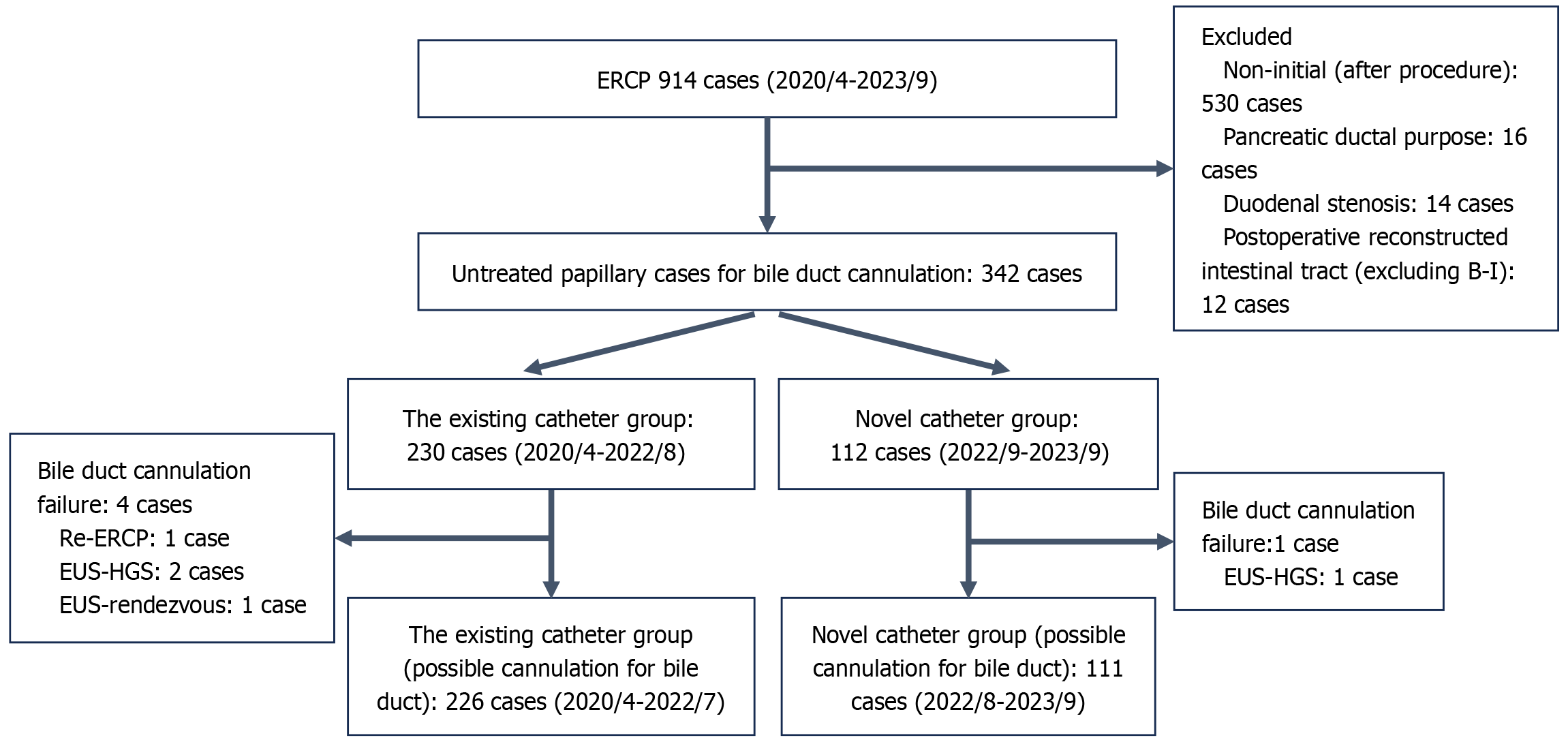
We retrospectively reviewed the medical records of patients who underwent ERCP at Kitasato University Medical Center from April 2020 to September 2023. During the specified period, 914 patients underwent ERCP, and those who met the inclusion criteria and none of the exclusion criteria were enrolled. The inclusion criteria were as follows: (1) History of ERCP for bile duct cannulation; and (2) Initial untreated papilla (naive papilla). The exclusion criteria were as follows: (1) History of ERCP for pancreatic diseases; (2) History of upper gastrointestinal surgery except the Billroth1 procedure; and (3) Duodenal stenosis that prevented endoscopic insertion to the duodenal papilla. Finally, a total of 342 patients fulfilled these criteria (Figure 1).
From April 2020 to July 2022, an existing catheter (MTW ERCP catheter; MTW Endoscopy, Wesel, Germany) was used, and from August 2022 to September 2023, a novel catheter (FineJet Cannula; Gadelius Medical, Tokyo, Japan Gadelius Medical Co. Ltd., Tokyo, Japan) was used for ERCP. Of the 342 patients with untreated papillae, 230 were treated with the existing catheter, and 112 were treated using the novel catheter.
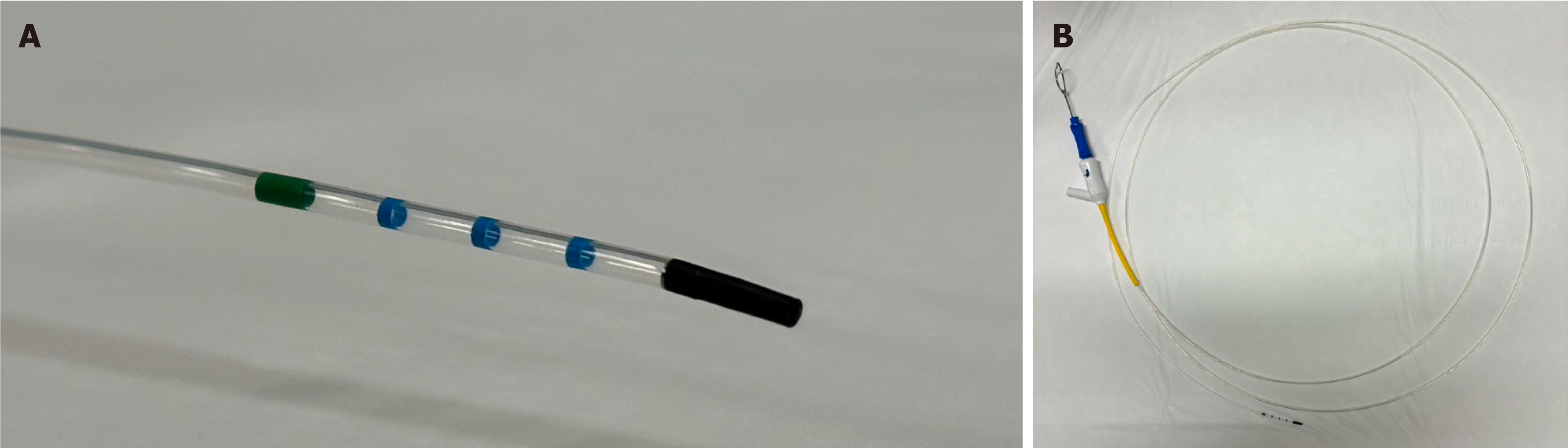
The novel catheter is a disposable contrast-enhanced catheter with a 4.4 French tapered and chamfered tip (Figure 2A). The shaft diameter is 7 French and total length is 220 cm, with a central lumen accommodating up to 0.035 inches of GW and contrast medium (Figure 2B). This configuration allowed simultaneous GW operation while contrast medium flows through the lumen. The catheter has a soft overall structure owing to its large central lumen.
Bile duct cannulation using only a contrast-enhanced catheter or WGC was defined as the standard technique, whereas cases wherein the catheter was changed to a sphincterotome (Clever Cut 3V; Olympus Medical Systems, Tokyo, Japan), pancreatic duct GW technique, or pre-cut two devices in one channel technique were defined as rescue techniques. Successful bile duct cannulation was defined as successful insertion of the catheter into the bile duct and successful cholangiography. Difficulty in bile duct cannulation was defined as five or more (> 5) attempts at bile duct cannulation. The procedure time was defined as the time from endoscope insertion to removal, and the bile duct cannulation time was defined as the time from the frontal view of the duodenal papillae to successful bile duct cannulation. Experts were defined as those with experience of performing > 500 ERCP procedures. When a trainee performs ERCP, the expert performs it together with the trainee as a caregiver in a supervisory position. large oral protrusion was defined as the length of the oral protuberance that was at least twice the lateral diameter of the duodenal papilla[15]. Adverse events (AE) severity was classified according to the lexicon of the American Society of Gastrointestinal Endoscopy[22].
The primary endpoint was the success rate of bile duct cannulation using only contrast-enhanced catheters. The secondary endpoints included the overall rate of bile duct cannulation, frequency of difficult cannulation cases, and incidence of AE.
Pethidine hydrochloride and midazolam were used for sedation. A duodenoscope (TJF290V, TJF260V, or JF260V; Olympus Medical Systems, Tokyo, Japan) was inserted into the duodenal papilla. The opening of the duodenal papillae was viewed in the frontal plane, and the bile duct was intubated with a GW (Visiglide2; Olympus Medical Systems, Filder25; Asahi Intech, Aichi, Japan) inserted into a contrast-enhanced catheter. Bile duct cannulation was initially performed using contrast-enhanced or conventional WGC. When bile duct cannulation was difficult, a rescue method was used, and the surgeon decided which method to use. Pre-cutting was performed via freehand fistulotomy using a Needle Knife (Needle Cut 3V; Olympus Medical Systems). After bile duct cannulation, endoscopic sphincterotomy, endoscopic lithectomy, or endoscopic biliary drainage was performed according to the case requirements. When a trainee performed ERCP and had difficulty intubating the bile duct, an expert replaced them after at least 10 minutes or ≥ 5-10 attempts.
According to a previous report[23], the success rate of bile duct cannulation using the conventional method is 62.8%. Assuming that the success rate improves to 80% when using a novel catheter, with an alpha error of 5% and a power of 80%, the required sample size for each group was calculated to be 105. Considering ineligible patients, we planned to include 112 patients in the novel catheter group. However, the existing catheter group had a significantly larger number of cases than the novel catheter group during the study period, with 230 cases observed, which exceeded the initially calculated sample size of 105 cases. Therefore, the number of cases observed during the observation period was used to define the sample size.
Statistical analysis was performed using SPSS version 17.0 (IBM Corp., Armonk, NY, United States) and R statistical package version 3.2.4 (R Foundation for Statistical Computing, Vienna, Austria). Continuous variables are expressed as medians and interquartile ranges, whereas categorical variables are presented as percentages and absolute numbers. Continuous variables were compared using the Mann-Whitney U-test, whereas categorical variables were compared using Fisher exact tests. All P values were two-sided, and statistical significance was set at P < 0.05. All authors have access to and reviewed the study data and approved the final manuscript.
A total of 342 patients were identified using database analysis. Among these, 230 patients underwent ERCP with existing catheters, and 112 with novel catheters. Table 1 describes the patients’ baseline characteristics. No significant differences were noted in age, sex, or primary disease between the existing and novel catheter groups. Similarly, no significant differences were observed in anatomical factors affecting bile duct cannulation[13-15], such as parapapillary diverticulum and long oral ridge, between the two groups. Further, no significant difference was noted between expert and non-expert physicians who performed the procedure in the two groups.
| Character | Existing catheter group (n = 230) | Novel catheter group (n = 112) | P value |
| Age median (range) | 77 (29-97) | 80.5 (44-104) | 0.84 |
| Sex (male/female) | 144/96 | 56/56 | 0.874 |
| Primary disease | |||
| Benign disease | 147 (63.9) | 73 (65.1) | - |
| Bile duct stones | 134 (58.2) | 66 (58.9) | - |
| Benign bile duct stricture | 6 (2.6) | 2 (1.8) | - |
| Other (benign) | 7 (3.0) | 5 (4.5) | - |
| Malignant disease | 83 (36.1) | 39 (34.8) | - |
| Pancreatic cancer | 33 (14.3) | 16 (14.2) | - |
| Cholangiocarcinoma | 46 (20.0) | 22 (19.6) | - |
| Other (malignant) | 4 (1.7) | 1 (0.9) | - |
| Benign/malignant disease | 147/83 | 73/39 | 0.90 |
| Parapapillary diverticular papilla | 60 (26.1) | 27 (24.1) | 0.79 |
| Oral protrusion-large | 60 (26.1) | 28 (25.0) | 0.90 |
| Expert/non-expert | 115/115 | 64/48 | 0.25 |
Table 2 presents the overall treatment results. The overall rates of bile duct cannulation were 98.2% and 99.1% in the existing and novel catheter groups, respectively, with no significant differences. Bile duct cannulation was not possible in five patients (1.5%): One patient underwent repeat ERCP to allow bile duct cannulation, three underwent EUS-guided hepaticogastrostomy, and one underwent bile duct cannulation using the EUS-guided rendezvous technique. The frequencies of difficult cannulation were 41.6% with existing catheters and 32.4% with the novel catheter, with no significant difference. In contrast, the rates of bile duct cannulation with the standard technique were 74.3% for existing catheters and 82.9% for the novel catheter, with a significant difference (P = 0.042). The incidences of AE were 5.2% in the existing catheter group and 4.5% in the novel catheter group, with no significant difference. The incidences of PEP were 4.3% in the existing catheter group and 2.7% in the novel catheter group, with no significant difference observed.
| Character | Existing catheter group (n = 230) | Novel catheter group (n = 112) | P value |
| Cannulation success rate | 98.3% (226/230) | 99.1% (111/112) | 0.47 |
| Number of attempts of cannulation, median (range) | 3 (1-20) | 3 (1-10) | 0.58 |
| Difficult cannulation (> 5 times) | 94 (40.9) | 36 (32.1) | 0.074 |
| Cannulation success rate with the standard technique | 73.0% (168/230) | 82.1% (92/112) | 0.042 |
| Rescue technique | |||
| Switch to sphincterotomes | 8 (3.5) | 0 | 0.039 |
| Pancreatic duct GW method | 14 (6.1) | 2 (1.8) | 0.059 |
| Precut | 35 (15.2) | 17 (15.3) | 0.56 |
| Two devices in one channel method | 1 (0.4) | 0 | 0.67 |
| Cannulation failure | 4 (1.7) | 1 (0.9) | 0.47 |
| Re-ERCP | 1 (0.4) | 0 | 0.67 |
| EUS-HGS | 2 (0.9) | 1 (0.9) | 0.70 |
| EUS-rendezvous | 1 (0.4) | 0 | 0.67 |
| Adverse event | |||
| Total | 12 (5.2) | 5 (4.5) | 0.70 |
| Bleeding | 2 (0.9) | 2 (1.8) | 0.60 |
| PEP | 10 (4.3) | 3 (2.7) | 0.59 |
| Mild | 9 (3.9) | 2 (1.8) | 0.51 |
| Moderate disease | 1 (0.4) | 1 (0.9) | 0.55 |
| Severe disease | 0 | 0 | - |
Table 3 presents the treatment performance results achieved by non-experts. The overall rates of bile duct cannulation were 99.1% in the existing catheter group and 100% in the novel catheter group, with no significant difference. The frequencies of difficult cannulation were 49.1% and 52.1% in the existing and novel catheter groups, respectively, with no significant differences. The rates of bile duct cannulation using the standard technique were 79.1% for the existing catheter group and 83.3% for the novel catheter group, with no significant differences. The incidences of AE were 3.5% in the existing catheter group and 6.3% in the novel catheter group, with no significant difference, and those of PEP were 2.6% in the existing catheter group and 2.1% in the novel, with no significant difference.
| Character | Existing catheter group (n = 115) | Novel catheter group (n = 48) | P value |
| Cannulation success rate | 99.1% (114/115) | 100% (48/48) | 0.71 |
| Number of attempts of cannulation median (range) | 4.5 (1-20) | 5 (1-10) | 0.67 |
| Difficult cannulation (> 5 times) | 56 (48.7) | 25 (52.1) | 0.73 |
| Cannulation success rate with the standard technique | 79.1% (91/115) | 83.3% (40/48) | 0.66 |
| Rescue technique | |||
| Switch to sphincterotomes | 2 (1.7) | 0 | 0.47 |
| Pancreatic duct GW method | 5 (4.3) | 1 (2.1) | 0.67 |
| Precut | 13 (11.3) | 7 (14.6) | 0.60 |
| Two devices in one channel method | 1 (0.9) | 0 | 0.69 |
| Cannulation failure | 1 (0.9) | 0 | 0.69 |
| Re-ERCP | 0 | 0 | - |
| EUS-HGS | 1 (0.9) | 0 | 0.69 |
| EUS-rendezvous | 0 | 0 | - |
| Adverse event | |||
| Total | 4 (3.5) | 3 (6.3) | 0.50 |
| Bleeding | 1 (0.9) | 2 (4.2) | 0.21 |
| PEP | 3 (2.6) | 1 (2.1) | 0.66 |
| Mild disease | 3 (2.6) | 1 (2.1) | 0.66 |
| Moderate disease | 0 | 0 | - |
| Severe disease | 0 | 0 | - |
Table 4 presents the treatment outcomes achieved by experts. The overall rates of bile duct cannulation were 97.3% and 98.4% in the existing and novel catheter groups, respectively, with no significant differences. The frequencies of difficult cannulation were 33.0% and 17.4% in the existing and novel catheter groups, respectively, with significantly less difficult cannulation in the novel catheter group (P = 0.019). The rates of bile duct cannulation with the standard technique were 65.2% for the existing catheters and 81.3% for the novel catheter, with a significant difference (P = 0.017). The incidences of AE were 7.0% in the existing catheter group and 3.1% in the novel catheter group, with no significant difference. The incidences of PEP were 6.1% in the existing catheter group and 3.1% in the novel catheter group, with no significant difference.
| Character | Existing catheter group (n = 115) | Novel catheter group (n = 64) | P value |
| Cannulation success rate | 97.3% (112/115) | 98.4% (63/64) | 0.55 |
| Number of attempts of cannulation median (range) | 2 (1-18) | 2 (1-10) | 0.67 |
| Difficult cannulation (> 5 times) | 37 (32.1) | 11 (17.2) | 0.021 |
| Cannulation success rate with the standard technique | 65.2% (75/115) | 81.3% (52/64) | 0.017 |
| Rescue technique | |||
| Switch to sphincterotomes | 6 (5.2) | 0 | 0.067 |
| Pancreatic duct GW method | 9 (7.8) | 1.6% (1/64) | 0.073 |
| Precut | 22 (19.1) | 15.6% (10/64) | 0.36 |
| Two devices in one channel method | 0 | 0 | - |
| Cannulation failure | 3 (2.7) | 1 (1.6) | 0.55 |
| Re-ERCP | 1 (0.9) | 0 | 0.64 |
| EUS-HGS | 1(0.9) | 1 (1.6) | 0.59 |
| EUS-rendezvous | 1 (0.9) | 0 | 0.64 |
| Adverse event | |||
| Total | 8 (7.0) | 2 (3.1) | 0.24 |
| Bleeding | 1 (0.9) | 0 | 0.64 |
| PEP | 7 (6.1) | 2 (3.1) | 0.31 |
| Mild disease | 6 (5.2) | 1 (1.6) | 0.39 |
| Moderate disease | 1 (0.9) | 1 (1.6) | 0.64 |
| Severe disease | 0 | 0 | - |
In this study, we explored the usefulness of bile duct cannulation using a novel catheter in ERCP. Selective bile duct cannulation is an important step in ERCP, as it serves as a gateway to subsequent interventions. Moreover, patients with difficult bile duct cannulation are at high risk for PEP[8], underscoring the importance of facilitating this aspect of the procedure.
Our investigation revealed that the use of the novel catheter improved the rate of bile duct cannulation using the standard technique. This improvement could potentially be attributed to the catheter’s chamfered tip and softness, facilitating its alignment with the bile duct axis. This finding was supported by the fact that no cases of sphincterotome conversion were noted in the novel catheter group. The sphincterotome catheter can be adjusted by stretching the knife in the direction of the catheter, making it easier to look up and align with the bile duct axis, with a study reporting that the rate of bile duct cannulation was higher with the sphincterotome than with a conventional contrast catheter[20]. However, the characteristics of the new catheter suggest that it can be aligned with the bile duct axis without using a sphincterotome.
The rate of bile duct cannulation was higher with the novel catheter using the standard technique than with existing catheters; however, the overall rate showed a trend toward a lower incidence of difficult cannulations, but the difference was not statistically significant. Difficult cannulation is considered a risk factor for PEP[19]; therefore, reducing the frequency is important to reduce the risk of PEP and perform safe ERCP. To examine the results of this study in detail, we determined whether the participating physicians were experts or non-experts. No significant differences were observed between the novel and the existing catheter groups. Meanwhile, the use of novel catheters in the expert group decreased the frequency of difficult cannulation and increased the bile duct cannulation rate using the standard technique compared with the use of existing catheters. However, the incidence of AE was similar between the two groups. These results suggest that using the novel catheter facilitated bile duct cannulation in the expert group. This may be because the experts could understand the characteristics of the novel catheter and orient it toward the bile duct axis. Consequently, treatment outcomes may be more favorable.
Furthermore, rescue techniques such as the double- GW technique with a GW placed in the pancreatic duct and pre-cut have been reported to increase the risk of PEP[19,24,25]. Therefore, our study’s results hold significance, as a higher rate of bile duct cannulation using only the standard technique may reduce the risk of PEP. The incidences of AE were 5.2% in the existing catheter group and 4.5% in the novel; however, this difference was not significant. The incidences of pancreatitis after ERCP decreased to 4.3% and 2.7% in the existing and novel catheter groups, respectively. However, there was a trend toward fewer cases reported in both groups, although the difference was not significant[17]. No serious complications were observed in either of the groups. Reportedly, the incidence of AE increased when ERCP was performed by non-experts or at institutions with limited experience. However, in this study, even when non-experts performed ERCP, the incidences of incidental injury were 3.5% in the existing catheter group and 6.3% in the novel catheter group, with a low incidence in both groups. The incidences of pancreatitis after ERCP were 2.6% in the existing catheter group and 2.1% in the novel catheter group, even when non-experts performed catheterization. In this study, non-experts were assisted by an expert in the supervisory position when performing ERCP. As a result, the procedure could be performed safely, and the incidence of accidental injury was low in both groups.
In recent years, endoscopic ultrasonography-guided biliary drainage has gained popularity as an alternative in patients who have difficulty with ERCP[26-28]. The treatment results were excellent and comparable with those of ERCP[29]. However, there are cases in which EUS-guided biliary drainage cannot be performed, such as in patients with very narrow bile ducts or large amounts of ascites. Therefore, improving the success rate of ERCP is important. Our study highlights the efficacy of the novel catheter in improving the rate of bile duct cannulation using the conventional method, thus filling a notable gap in existing literature.
This study has some limitations. First, this was a single-center retrospective study, with a small sample size. Second, because there were multiple surgeons, the choice of the ERCP technique was not constant and depended on the choice of the endoscopist, which may have led to bias. In the future, it would be desirable to study a larger number of cases considering all these factors. In addition to a larger sample size, performing a randomized controlled trial to compare the efficacy and safety of new and conventional catheters would be helpful.
This novel catheter improved the success rate of bile duct cannulation using the conventional method. Further, its application by experts has shown promise in reducing the frequency of difficult cannulation, underscoring its utility in clinical practice.
| 1. | Moss AC, Morris E, Mac Mathuna P. Palliative biliary stents for obstructing pancreatic carcinoma. Cochrane Database Syst Rev. 2006;CD004200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 92] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 2. | Inamdar S, Slattery E, Bhalla R, Sejpal DV, Trindade AJ. Comparison of Adverse Events for Endoscopic vs Percutaneous Biliary Drainage in the Treatment of Malignant Biliary Tract Obstruction in an Inpatient National Cohort. JAMA Oncol. 2016;2:112-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 125] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 3. | Mukai S, Itoi T, Baron TH, Takada T, Strasberg SM, Pitt HA, Ukai T, Shikata S, Teoh AYB, Kim MH, Kiriyama S, Mori Y, Miura F, Chen MF, Lau WY, Wada K, Supe AN, Giménez ME, Yoshida M, Mayumi T, Hirata K, Sumiyama Y, Inui K, Yamamoto M. Indications and techniques of biliary drainage for acute cholangitis in updated Tokyo Guidelines 2018. J Hepatobiliary Pancreat Sci. 2017;24:537-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 135] [Article Influence: 15.0] [Reference Citation Analysis (1)] |
| 4. | DeBenedet AT, Elmunzer BJ, McCarthy ST, Elta GH, Schoenfeld PS. Intraprocedural quality in endoscopic retrograde cholangiopancreatography: a meta-analysis. Am J Gastroenterol. 2013;108:1696-704; quiz 1705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Pécsi D, Farkas N, Hegyi P, Balaskó M, Czimmer J, Garami A, Illés A, Mosztbacher D, Pár G, Párniczky A, Sarlós P, Szabó I, Szemes K, Szűcs Á, Vincze Á. Transpancreatic sphincterotomy has a higher cannulation success rate than needle-knife precut papillotomy - a meta-analysis. Endoscopy. 2017;49:874-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Tse F, Liu J, Yuan Y, Moayyedi P, Leontiadis GI. Guidewire-assisted cannulation of the common bile duct for the prevention of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis. Cochrane Database Syst Rev. 2022;3:CD009662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Williams EJ, Taylor S, Fairclough P, Hamlyn A, Logan RF, Martin D, Riley SA, Veitch P, Wilkinson M, Williamson PR, Lombard M; BSG Audit of ERCP. Are we meeting the standards set for endoscopy? Results of a large-scale prospective survey of endoscopic retrograde cholangio-pancreatograph practice. Gut. 2007;56:821-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 183] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 8. | Haraldsson E, Kylänpää L, Grönroos J, Saarela A, Toth E, Qvigstad G, Hult M, Lindström O, Laine S, Karjula H, Hauge T, Sadik R, Arnelo U. Macroscopic appearance of the major duodenal papilla influences bile duct cannulation: a prospective multicenter study by the Scandinavian Association for Digestive Endoscopy Study Group for ERCP. Gastrointest Endosc. 2019;90:957-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 77] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 9. | Shi HX, Ye YQ, Zhao HW, Kong DC, Huang SZ, Yan Q, Chen YB, Zhang P, Chen S, Hou BH, Zhang CZ. A new classification of periampullary diverticulum: cannulation of papilla on the inner margins of the diverticulum (Type IIa) is more challenging. BMC Gastroenterol. 2023;23:252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 10. | Watanabe M, Okuwaki K, Kida M, Imaizumi H, Yamauchi H, Kaneko T, Iwai T, Hasegawa R, Miyata E, Masutani H, Tadehara M, Adachi K, Koizumi W. Transpapillary Biliary Cannulation is Difficult in Cases with Large Oral Protrusion of the Duodenal Papilla. Dig Dis Sci. 2019;64:2291-2299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 11. | Teles de Campos S, Papaefthymiou A, Florou T, Facciorusso A, Arvanitakis M, Devière J, Gkolfakis P. Impact of center and endoscopist ERCP volume on ERCP outcomes: a systematic review and meta-analysis. Gastrointest Endosc. 2023;98:306-315.e14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 12. | Siegel JH, Pullano W. Two new methods for selective bile duct cannulation and sphincterotomy. Gastrointest Endosc. 1987;33:438-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Binmoeller KF, Seifert H, Gerke H, Seitz U, Portis M, Soehendra N. Papillary roof incision using the Erlangen-type pre-cut papillotome to achieve selective bile duct cannulation. Gastrointest Endosc. 1996;44:689-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 75] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Herreros de Tejada A, Calleja JL, Díaz G, Pertejo V, Espinel J, Cacho G, Jiménez J, Millán I, García F, Abreu L; UDOGUIA-04 Group. Double-guidewire technique for difficult bile duct cannulation: a multicenter randomized, controlled trial. Gastrointest Endosc. 2009;70:700-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 103] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 15. | Fujita N, Noda Y, Kobayashi G, Kimura K, Yago A. ERCP for intradiverticular papilla: two-devices-in-one-channel method. Endoscopic Retrograde Cholangiopancreatography. Gastrointest Endosc. 1998;48:517-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 66] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | Klair JS, Zafar Y, Ashat M, Bomman S, Murali AR, Jayaraj M, Law J, Larsen M, Singh DP, Rustagi T, Irani S, Ross A, Kozarek R, Krishnamoorthi R. Effectiveness and Safety of EUS Rendezvous After Failed Biliary Cannulation With ERCP: A Systematic Review and Proportion Meta-analysis. J Clin Gastroenterol. 2023;57:211-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 31] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 17. | ASGE Standards of Practice Committee; Chandrasekhara V, Khashab MA, Muthusamy VR, Acosta RD, Agrawal D, Bruining DH, Eloubeidi MA, Fanelli RD, Faulx AL, Gurudu SR, Kothari S, Lightdale JR, Qumseya BJ, Shaukat A, Wang A, Wani SB, Yang J, DeWitt JM. Adverse events associated with ERCP. Gastrointest Endosc. 2017;85:32-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 589] [Article Influence: 65.4] [Reference Citation Analysis (0)] |
| 18. | Mutneja HR, Vohra I, Go A, Bhurwal A, Katiyar V, Palomera Tejeda E, Thapa Chhetri K, Baig MA, Arora S, Attar B. Temporal trends and mortality of post-ERCP pancreatitis in the United States: a nationwide analysis. Endoscopy. 2021;53:357-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 64] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 19. | Freeman ML, DiSario JA, Nelson DB, Fennerty MB, Lee JG, Bjorkman DJ, Overby CS, Aas J, Ryan ME, Bochna GS, Shaw MJ, Snady HW, Erickson RV, Moore JP, Roel JP. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001;54:425-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 801] [Cited by in RCA: 852] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 20. | Laasch HU, Tringali A, Wilbraham L, Marriott A, England RE, Mutignani M, Perri V, Costamagna G, Martin DF. Comparison of standard and steerable catheters for bile duct cannulation in ERCP. Endoscopy. 2003;35:669-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 32] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Kawakami H, Maguchi H, Mukai T, Hayashi T, Sasaki T, Isayama H, Nakai Y, Yasuda I, Irisawa A, Niido T, Okabe Y, Ryozawa S, Itoi T, Hanada K, Kikuyama M, Arisaka Y, Kikuchi S; Japan Bile Duct Cannulation Study Group. A multicenter, prospective, randomized study of selective bile duct cannulation performed by multiple endoscopists: the BIDMEN study. Gastrointest Endosc. 2012;75:362-372, 372.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 22. | Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71:446-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1238] [Cited by in RCA: 2016] [Article Influence: 126.0] [Reference Citation Analysis (1)] |
| 23. | Maruta S, Sugiyama H, Ogasawara S, Sugihara C, Ouchi M, Kan M, Yamada T, Miura Y, Nagashima H, Takahashi K, Kusakabe Y, Ohyama H, Okitsu K, Ohno I, Mikata R, Sakai Y, Tsuyuguchi T, Kato J, Kato N. "Salvage techniques" are the key to overcome difficult biliary cannulation in endoscopic retrograde cholangiopancreatography. Sci Rep. 2022;12:13627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 24. | Guzmán-Calderón E, Martinez-Moreno B, Casellas JA, Aparicio JR. Transpancreatic precut papillotomy versus double-guidewire technique in difficult biliary cannulation: a systematic review and meta-analysis. Endosc Int Open. 2021;9:E1758-E1767. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 25. | Facciorusso A, Ramai D, Gkolfakis P, Khan SR, Papanikolaou IS, Triantafyllou K, Tringali A, Chandan S, Mohan BP, Adler DG. Comparative efficacy of different methods for difficult biliary cannulation in ERCP: systematic review and network meta-analysis. Gastrointest Endosc. 2022;95:60-71.e12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 74] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 26. | Dhindsa BS, Mashiana HS, Dhaliwal A, Mohan BP, Jayaraj M, Sayles H, Singh S, Ohning G, Bhat I, Adler DG. EUS-guided biliary drainage: A systematic review and meta-analysis. Endosc Ultrasound. 2020;9:101-109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 71] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 27. | van der Merwe SW, van Wanrooij RLJ, Bronswijk M, Everett S, Lakhtakia S, Rimbas M, Hucl T, Kunda R, Badaoui A, Law R, Arcidiacono PG, Larghi A, Giovannini M, Khashab MA, Binmoeller KF, Barthet M, Perez-Miranda M, van Hooft JE. Therapeutic endoscopic ultrasound: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2022;54:185-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 400] [Cited by in RCA: 334] [Article Influence: 83.5] [Reference Citation Analysis (3)] |
| 28. | Kaneko T, Kida M, Kitahara G, Uehara K, Koyama S, Tachikawa S, Watanabe M, Kusano C. Introduction of endoscopic ultrasound-guided hepaticoenterostomy - experience from a general hospital in Japan. Endosc Int Open. 2022;10:E1364-E1370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 29. | Kakked G, Salameh H, Cheesman AR, Kumta NA, Nagula S, DiMaio CJ. Primary EUS-guided biliary drainage versus ERCP drainage for the management of malignant biliary obstruction: A systematic review and meta-analysis. Endosc Ultrasound. 2020;9:298-307. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 50] [Article Influence: 8.3] [Reference Citation Analysis (1)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/