Published online Aug 16, 2024. doi: 10.4253/wjge.v16.i8.489
Revised: June 30, 2024
Accepted: July 5, 2024
Published online: August 16, 2024
Processing time: 64 Days and 2.1 Hours
Interventional endoscopic ultrasound is clinically used for the treatment of isolated gastric varices (IGVs) owing to its precise visualization.
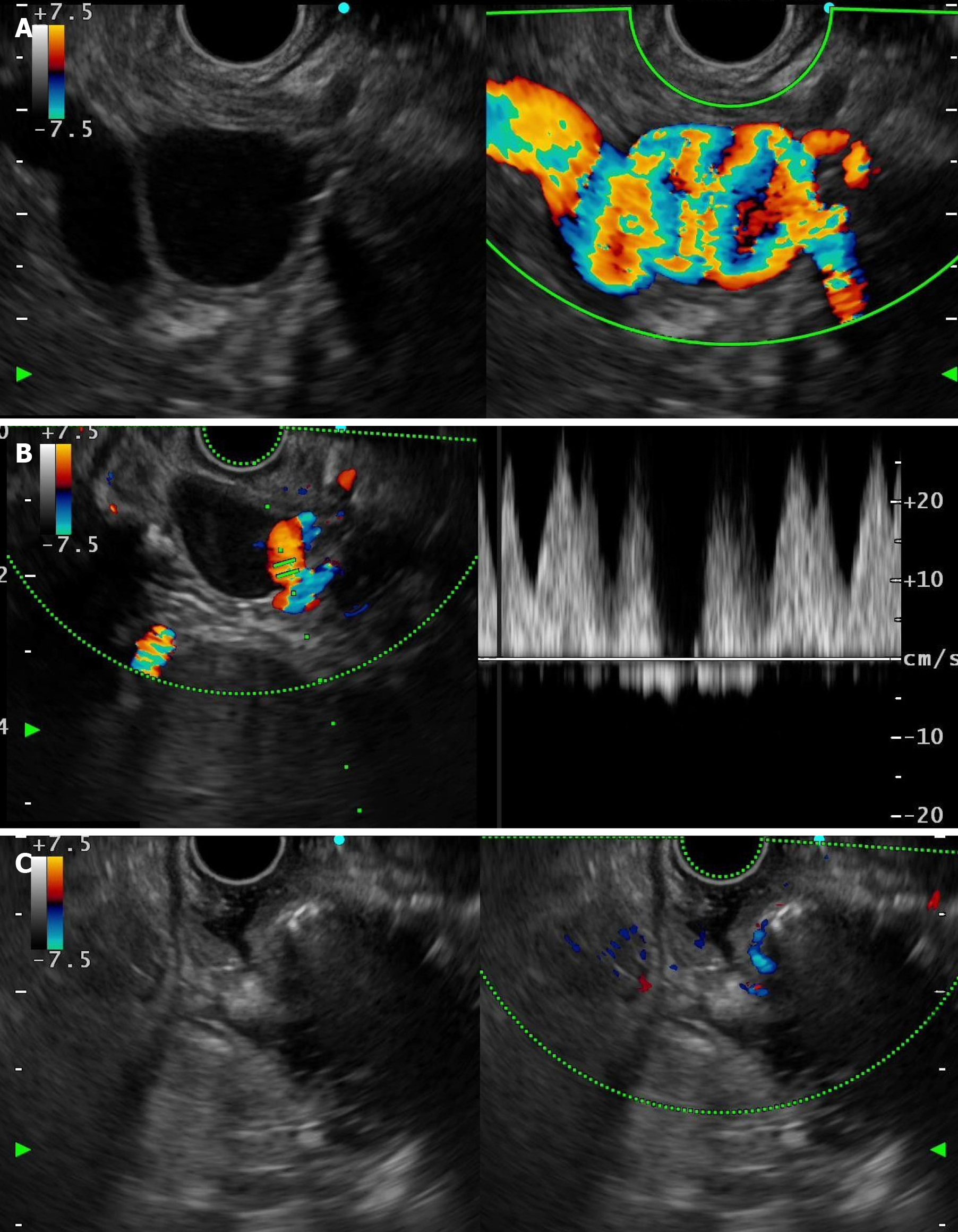
A 39-year-old man was diagnosed with a large IGV during a routine physical examination. Endoscopic ultrasonography showed gastric varices entwined with an artery, which greatly increased the difficulty of treatment. We successfully treated the patient with endoscopic ultrasonography-guided coil embolization combined with cyanoacrylate injection.
Endoscopic ultrasonography-guided coil embolization combined with cyanoacrylate injection was safe and effective for the treatment of an IGV entwined with an artery.
Core Tip: Isolated gastric varices (IGVs) are potentially fatal, and endoscopic treatment is the main treatment. Endoscopic ultrasound (EUS)-guided therapy is more precise than conventional endoscopic therapy. In this case, we successfully treated an IGV entwined with an artery by EUS-guided coil embolization combined with cyanoacrylate injection. This was an effective treatment of an IGV entwined with an artery.
- Citation: Zhang HY, He CC, Zhong DF. Endoscopic ultrasound-guided treatment of isolated gastric varices entwined with arteries: A case report. World J Gastrointest Endosc 2024; 16(8): 489-493
- URL: https://www.wjgnet.com/1948-5190/full/v16/i8/489.htm
- DOI: https://dx.doi.org/10.4253/wjge.v16.i8.489
Gastric varices (GVs) have a 65% risk of bleeding within 2 years and a mortality rate of up to 20%[1]. Endoscopic ultrasound (EUS)-guided therapy has recently become a cutting-edge treatment for GVs[2]. A relevant meta-analysis revealed an effectiveness rate of 93.7%, an occlusion rate of 84.4%, a recurrence rate of 9.1%, and a rebleeding rate of 18.6% for EUS-guided therapy of GVs, which were superior to direct injection during gastroscopy[3]. Ultrasound enables real-time visualization of the injection of cyanoacrylate into varicose veins, thus achieving a precision that is not possible with conventional endoscopic therapy. In addition, coil embolization combined with endoscopic cyanoacrylate injection reduces the risk of ectopic embolism. In this study, we report, for the first time, a case of an isolated GV (IGV) entwined with an artery that was successfully treated by EUS-guided coil embolization combined with cyanoacrylate injection.
This case involved a 39-year-old man who was admitted to the hospital with an IGV.
The patient was admitted to the hospital for endoscopic treatment of a large submucosal bulge in the gastric fundus that was approximately 4 cm × 5 cm in size and found during routine gastroscopy 2 wk previously. EUS examination revealed that the mucosal bulge was a varicose vein. There was no abdominal discomfort or gastrointestinal bleeding.
The patient had a history of hyperthyroidism, had been taking methimazole for a long time, and was a hepatitis B virus carrier.
The patient was allergic to the iodine contrast agent.
Physical examination was unremarkable.
Blood biochemistry test results, coagulation function, and immunoglobulin level were normal. Antinuclear antibody was weakly positive at a 1:80 dilution.
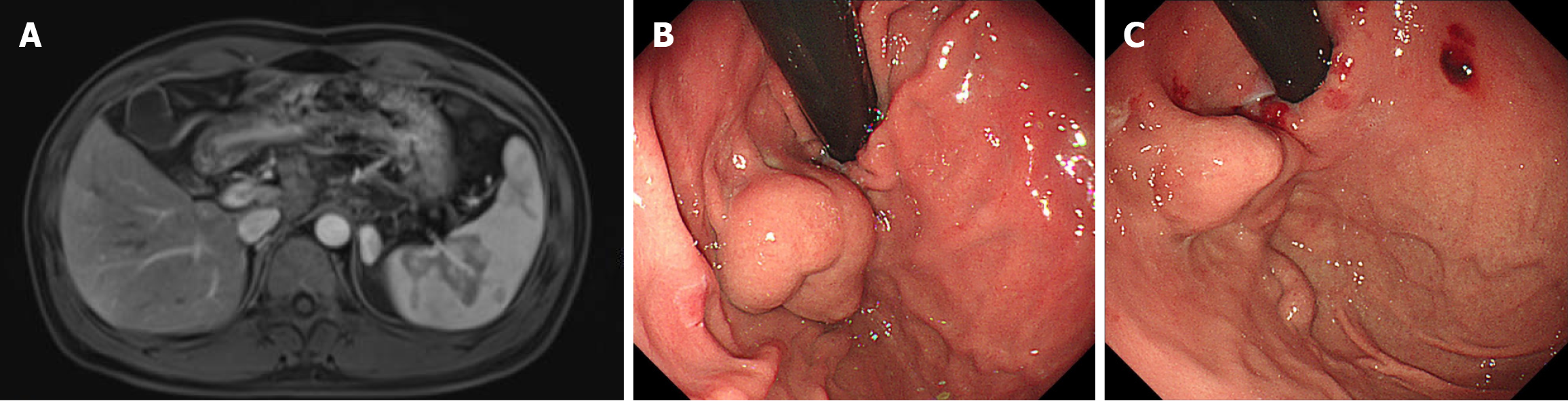
Colour ultrasound of the portal vein system showed no obvious abnormalities. Magnetic resonance imaging (MRI) en
The final diagnosis was an IGV entwined with an artery.
EUS guidance allowed precise avoidance of the entwined artery and successful coil embolization by cyanoacrylate injection (Figure 2C). The IGV subsided after treatment (Figure 1C).
The patient had no abdominal pain, gastrointestinal bleeding, fever, or ectopic embolism and was discharged 3 d after the procedure. There was no obvious discomfort at the 1-year follow-up.
IGVs occur less frequently than oesophageal varices, but they are associated with higher morbidity and mortality rates[4]. The Sarin classification includes two types of GV. IGV1 are in the fundus of the stomach, and IGV2 are located anywhere other than the fundus[5]. IGVs are observed in cirrhotic and noncirrhotic patients with portal hypertension (PHT)[6]. The aetiology of IGV can be divided into three categories from the perspective of anatomy and pathophy
Most IGVs are asymptomatic, are found incidentally, and are usually diagnosed by endoscopy. EUS is more accurate than endoscopy for observing IGVs and evaluating splenic venous patency. Contrast-enhanced computed tomography (CECT) and magnetic resonance angiography detect not only many gastric varicose veins but also reveal portal collateral circulation[7]. This patient had a history of chronic liver disease, but there was no diagnostic basis for PHT or a history of pancreatic disease. MRI enhancement revealed no obvious anatomical abnormalities. Unfortunately, the vascular ana
GV treatment has changed in recent decades. Transjugular intrahepatic portosystemic shunts are considered effective for reducing portal pressure and the risk of bleeding from oesophageal varices. However, the effectiveness of GV treatment is decreased if bleeding occurs when the portal vein pressure is low[9]. Study results show a 76.9%-100% success of balloon retrograde transvenous obliteration treatment for acute GVs. However, it was used only for treating GVs with a gastrorenal or gastro-vena cava shunt, which is limited to centres with advanced radiological capability[10]. EUS-guided coil deployment for treating IGVs is a novel intervention that has recently attracted considerable attention, and it can be combined with injection of cyanoacrylate given to embolize the IGV and feeders to prevent recurrence. EUS-guided coil deployment with cyanoacrylate injection/sclerotherapy has a reported success rate of 87.5%-94% for the treatment of IGVs[1,11]. A meta-analysis found that EUS-guided therapy was effective and safe for treating GVs, with an overall technical success rate, of 100%, a clinical success rate of 97%, and an adverse event rate of 14%. Compared with cyanoacrylate injection alone or coil embolization alone, EUS-guided coil embolization combined with cyanoacrylate injection was reported to be the preferred strategy for the treatment of GVs[12]. This patient had no signs of gas
EUS-guided interventional therapy was used to successfully treat an IGV entwined with arteries. because of the small sample size, its efficacy and safety need further evaluation in prospective studies.
The authors would like to thank the participants for their help.
| 1. | Kozieł S, Pawlak K, Błaszczyk Ł, Jagielski M, Wiechowska-Kozłowska A. Endoscopic Ultrasound-Guided Treatment of Gastric Varices Using Coils and Cyanoacrylate Glue Injections: Results after 1 Year of Experience. J Clin Med. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 2. | Thiruvengadam SS, Sedarat A. The Role of Endoscopic Ultrasound (EUS) in the Management of Gastric Varices. Curr Gastroenterol Rep. 2021;23:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (1)] |
| 3. | Mohan BP, Chandan S, Khan SR, Kassab LL, Trakroo S, Ponnada S, Asokkumar R, Adler DG. Efficacy and safety of endoscopic ultrasound-guided therapy versus direct endoscopic glue injection therapy for gastric varices: systematic review and meta-analysis. Endoscopy. 2020;52:259-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 93] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 4. | Goral V, Yılmaz N. Current Approaches to the Treatment of Gastric Varices: Glue, Coil Application, TIPS, and BRTO. Medicina (Kaunas). 2019;55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343-1349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 789] [Cited by in RCA: 870] [Article Influence: 25.6] [Reference Citation Analysis (42)] |
| 6. | Sarin SK, Jain AK, Lamba GS, Gupta R, Chowdhary A. Isolated gastric varices: prevalence, clinical relevance and natural history. Dig Surg. 2003;20:42-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Li X, Wu J, Fang F, Liu Y, Jiang W, Li G, Song J. Isolated gastric varices associated with antiphospholipid syndrome and protein S deficiency: a case report and review of the literature. J Int Med Res. 2024;52:3000605241240579. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Köklü S, Yüksel O, Arhan M, Coban S, Başar O, Yolcu OF, Uçar E, Ibiş M, Ertugrul I, Sahin B. Report of 24 left-sided portal hypertension cases: a single-center prospective cohort study. Dig Dis Sci. 2005;50:976-982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 52] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Tripathi D, Therapondos G, Jackson E, Redhead DN, Hayes PC. The role of the transjugular intrahepatic portosystemic stent shunt (TIPSS) in the management of bleeding gastric varices: clinical and haemodynamic correlations. Gut. 2002;51:270-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 163] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 10. | Kobayakawa M, Ohnishi S, Suzuki H. Recent development of balloon-occluded retrograde transvenous obliteration. J Gastroenterol Hepatol. 2019;34:495-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Irisawa A, Shibukawa G, Hoshi K, Yamabe A, Sato A, Maki T, Yoshida Y, Yamamoto S, Obara K. Endoscopic ultrasound-guided coil deployment with sclerotherapy for isolated gastric varices: Case series of feasibility, safety, and long-term follow-up. Dig Endosc. 2020;32:1100-1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | McCarty TR, Bazarbashi AN, Hathorn KE, Thompson CC, Ryou M. Combination therapy versus monotherapy for EUS-guided management of gastric varices: A systematic review and meta-analysis. Endosc Ultrasound. 2020;9:6-15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 95] [Article Influence: 15.8] [Reference Citation Analysis (1)] |