Published online Mar 16, 2024. doi: 10.4253/wjge.v16.i3.112
Peer-review started: January 2, 2024
First decision: January 16, 2024
Revised: January 16, 2024
Accepted: February 6, 2024
Article in press: February 6, 2024
Published online: March 16, 2024
Processing time: 71 Days and 15.1 Hours
Anal pruritus is a common anorectal symptom that can significantly impair a patient’s quality of life, including their mental health. It can be one of the most difficult proctological conditions to treat. Patients often delay seeking medical attention, since it is an embarrassing but non-life-threatening situation. Pruritus ani can be associated with idiopathic and secondary causes, such as anorectal diseases, cancer (anal or colorectal), dermatological and sexually transmitted diseases, fungal infections and systemic diseases. If patients are referred for a colonoscopy, this can sometimes provide the first opportunity to evaluate the perianal area. Classifications of anal pruritus are based on the abnormalities of the perianal skin, one of the most commonly used being the Washington classification. A proper digital anorectal examination is important, as well as an anoscopy to help to exclude anorectal diseases or suspicious masses. Endoscopists should be aware of the common etiologies, and classification of the perianal area abnormalities should be provided in the colonoscopy report. Information on treatment possibilities and follow-up can also be provided. The treatment normally consists of a triple approach: proper hygiene, elimination of irritants, and skin care and protection. Several topical therapies have been described as possible treatments, including steroids, capsaicin, tacrolimus and methylene blue intradermal injections.
Core Tip: Anal pruritus is a common anorectal symptom that can significantly impair a patient’s quality of life. Endoscopists should be aware of the possible etiologies, including anorectal diseases and anal or colorectal cancer. Classifications of anal pruritus are based on the abnormalities of the perianal skin. It is important to carry out a proper digital anorectal examination and an anoscopy in these patients.
- Citation: Albuquerque A. Anal pruritus: Don’t look away. World J Gastrointest Endosc 2024; 16(3): 112-116
- URL: https://www.wjgnet.com/1948-5190/full/v16/i3/112.htm
- DOI: https://dx.doi.org/10.4253/wjge.v16.i3.112
Anal pruritus is a common anorectal condition, and it is estimated that it affects between 1% to 5% of the population at some point in their lives[1]. It is an embarrassing condition, which can impair a patient’s quality of life[2,3]. Anal pruritus can also have a negative effect on a patient’s mental health[4].
Idiopathic pruritus is generally considered to be associated with fecal contamination of the skin, which initiates a vicious cycle of itching and scratching[3,5]. This results in skin maceration and a decrease in thickness of the fatty skin layer with hypertrophy and lichenification[3,5]. There are also several secondary causes that might be associated with anal pruritus[6]. Benign and malignant anorectal conditions such as hemorrhoids, fissures, fistulas, rectal prolapse, condylomas, Crohn’s disease, squamous cell carcinoma, colorectal cancer, Paget’s disease and melanoma are all possible secondary causes[6,7]. Hemorrhoids and anal fissures are the most common anorectal diseases associated with pruritus[8]. Dermatological and sexually transmitted diseases, fungal infections and systemic diseases such as diabetes mellitus, lymphoma, renal failure, hyperthyroidism disorders or iron deficiency anemia can also be associated[6,7].
A prospective two-year study, including 109 patients with anal pruritus as the only presenting complaint[8], showed that 35% of the patients had an abnormal proctosigmoidoscopy or colonoscopy. In total, 11% of patients had rectal cancer, while 5% had anal cancer and 2% had colon cancer. The duration of the pruritic symptoms and an age greater than 50 years were risk factors for a diagnosis of a neoplasm[8].
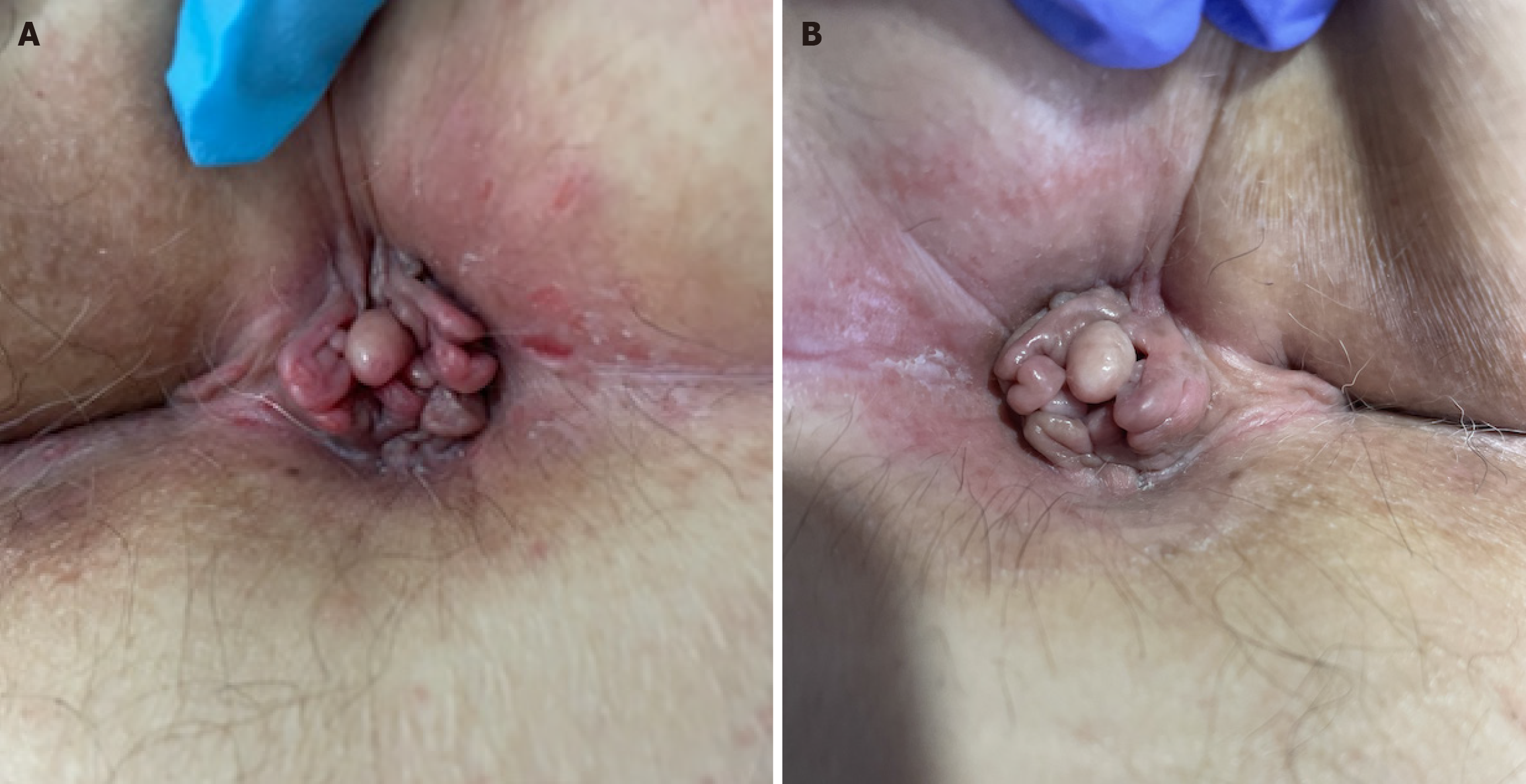
Patients with anal pruritis may be referred for a colonoscopy for several reasons, some unrelated to this condition, or to exclude a possible secondary cause. Endoscopists should start by conducting a proper examination of the perianal area, looking for erythema, fissures, ulceration or lichenified skin. The Washington classification is based on the appearance of the perianal area and can be provided in the examination report: stage 0 is normal skin; stage 1 is erythematous and inflamed skin (Figure 1); stage 2 is lichenified skin (Figure 2); and stage 3 is lichenified, coarse skin often with ulcerations (Figure 3)[9]. Endoscopists should also look for other conditions that might be associated, such as hemorrhoids or fissures. A proper anorectal digital examination should then be performed, with a search for suspicious masses. If possible, this should be followed by an anoscopy[7]. This detailed examination of the perianal area, combined with digital anorectal examination and an anoscopy, will allow a correct evaluation and classification of the situation, and should exclude anorectal diseases that might be associated with anal pruritis. It should be carried out before colonoscopy.
Treatment normally consists of a triple approach: Proper hygiene, elimination of irritants, and skin care and protection[6]. The area should be always clean and dry, avoiding overwiping, soaps, lotions and wet wipes that cause irritation[6]. Some foods and drinks should be avoided, such as coffee, tea, beer, chocolate, citrus fruits, cola, dairy products, and spicy foods (Figure 4A and B)[6].
A randomized control trial of 1% hydrocortisone ointment or placebo for 2 wk followed by the opposite treatment for a further 2-wk period, with a washout period of 2 wk between treatments, showed that treatment with 1% hydrocortisone ointment resulted in a 68% reduction in a visual analogue score compared with placebo[10]. Long-term topical steroids should be avoided as they cause skin atrophy and rebound symptoms after withdrawal[3,5].
A randomized control trial compared topical capsaicin 0.006% and placebo for idiopathic intractable pruritus ani for four weeks 3 times a day and showed that 31 of the 44 patients improved with capsaicin[11]. There were 4 patients who dropped out of capsaicin treatment because of side effects, three patients due to perianal burning and one due to urticaria. This substance seems to act by reducing the synthesis, storage, transport, and release of substance P, a neuropeptide that is a mediator of itching[11].
A recent meta-analysis and systematic review has evaluated the efficacy and safety of methylene blue injection for intractable idiopathic pruritus ani and included 7 studies with 225 patients[12]. This seemed to be a relatively efficacious therapy, but higher quality studies are necessary, including randomized control trials. Methylene blue destroys the intra
A randomized, double-blind, placebo-controlled clinical trial, including 21 patients with intractable idiopathic pruritus ani treated with tacrolimus 0.1% ointment, showed a significant positive effect of tacrolimus in reducing pruritus intensity and frequency, with symptom reduction in 68% of the patients 2 wk after treatment[14].
A case report has also described a case of a man with long-term anogenital pruritus that was refractory to multiple therapies and that responded to dupilumab, an interleukin-4 receptor alpha blocker[15].
Anal pruritus is a common anorectal condition that can either be idiopathic or have secondary etiologies, including anorectal diseases or even malignancies. It is important to conduct a detailed examination of the perianal area, a proper digital anorectal examination and an anoscopy. For treatment it is important to promote correct hygiene, the elimination of irritants and skin care. Several topical therapies have been described, including steroids, capsaicin, tacrolimus and methylene blue intradermal injections.
| 1. | Hanno R, Murphy P. Pruritus ani. Classification and management. Dermatol Clin. 1987;5:811-816. [PubMed] |
| 2. | Parés D, Abcarian H. Management of Common Benign Anorectal Disease: What All Physicians Need to Know. Am J Med. 2018;131:745-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (3)] |
| 3. | Schubert MC, Sridhar S, Schade RR, Wexner SD. What every gastroenterologist needs to know about common anorectal disorders. World J Gastroenterol. 2009;15:3201-3209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 60] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 4. | Hadasik K, Arasiewicz H, Brzezińska-Wcisło L. Assessment of the anxiety and depression among patients with idiopathic pruritus ani. Postepy Dermatol Alergol. 2021;38:689-693. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 5. | Ortega AE, Delgadillo X. Idiopathic Pruritus Ani and Acute Perianal Dermatitis. Clin Colon Rectal Surg. 2019;32:327-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Nasseri YY, Osborne MC. Pruritus ani: diagnosis and treatment. Gastroenterol Clin North Am. 2013;42:801-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Jakubauskas M, Dulskas A. Evaluation, management and future perspectives of anal pruritus: a narrative review. Eur J Med Res. 2023;28:57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (1)] |
| 8. | Daniel GL, Longo WE, Vernava AM 3rd. Pruritus ani. Causes and concerns. Dis Colon Rectum. 1994;37:670-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 40] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Gordon PH, Nivatvongs S. Perianal dermatologic disease. In: Gordon PH, editor. Principles and practice of surgery for the colon, rectum, and anus. 3rd edition. New York: Informa Healthcare. 2007;247-73. |
| 10. | Al-Ghnaniem R, Short K, Pullen A, Fuller LC, Rennie JA, Leather AJM. 1% hydrocortisone ointment is an effective treatment of pruritus ani: a pilot randomized controlled crossover trial. Int J Colorectal Dis. 2007;22:1463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Lysy J, Sistiery-Ittah M, Israelit Y, Shmueli A, Strauss-Liviatan N, Mindrul V, Keret D, Goldin E. Topical capsaicin--a novel and effective treatment for idiopathic intractable pruritus ani: a randomised, placebo controlled, crossover study. Gut. 2003;52:1323-1326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 85] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Jia W, Li Q, Ni J, Zhang Y, Wu L, Xu L. Efficacy and safety of methylene blue injection for intractable idiopathic pruritus ani: a single-arm metaanalysis and systematic review. Tech Coloproctol. 2023;27:813-825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Eusebio EB, Graham J, Mody N. Treatment of intractable pruritus ani. Dis Colon Rectum. 1990;33:770-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 42] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Suys E. Randomized study of topical tacrolimus ointment as possible treatment for resistant idiopathic pruritus ani. J Am Acad Dermatol. 2012;66:327-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (2)] |
| 15. | Yang EJ, Murase JE. Recalcitrant anal and genital pruritus treated with dupilumab. Int J Womens Dermatol. 2018;4:223-226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Portugal
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Nakamura K, Japan S-Editor: Liu JH L-Editor: A P-Editor: Zhao YQ