Published online Apr 16, 2023. doi: 10.4253/wjge.v15.i4.309
Peer-review started: December 29, 2022
First decision: January 20, 2023
Revised: February 9, 2023
Accepted: April 4, 2023
Article in press: April 4, 2023
Published online: April 16, 2023
Processing time: 106 Days and 4.3 Hours
Endoscopic placement of a self-expandable metal stent (SEMS) is a minimally invasive treatment for use in malignant and benign colonic obstruction. However, their widespread use is still limited with a nationwide analysis showing only 5.4% of patients with colon obstruction undergoing stent placement. This underuti
To review long- and short-term clinical success of SEMS use for colonic obstruction at our center.
We retrospectively reviewed all the patients who underwent colonic SEMS placement over a eighteen year period (August 2004 through August 2022) at our academic center. Demographics including age, gender, indication (malignant and benign), technical success, clinical success, complications (perforation, stent migration), mortality, and outcomes were recorded.
Sixty three patients underwent colon SEMS over an 18-year period. Fifty-five cases were for malignant indications, 8 were for benign conditions. The benign strictures included diverticular disease stricturing (n = 4), fistula closure (n = 2), extrinsic fibroid compression (n = 1), and ischemic stricture (n = 1). Forty-three of the malignant cases were due to intrinsic obstruction from primary or recurrent colon cancer; 12 were from extrinsic compression. Fifty-four strictures occurred on the left side, 3 occurred on the right and the rest in transverse colon. The total malignant case (n = 55) procedural success rate was 95% vs 100% for benign cases (P = 1.0, NS). Overall complication rate was significantly higher for benign group: Four complications were observed in the malignant group (stent migration, restenosis) vs 2 of 8 (25%) for benign obstruction (1-perforation, 1-stent migration) (P = 0.02). When stratifying complications of perforation and stent migration there was no significant difference between the two groups (P = 0.14, NS).
Colon SEMS remains a worthwhile option for colonic obstruction related to malignancy and has a high procedural and clinical success rate. Benign indications for SEMS placement appear to have similar success to malignant. While there appears to be a higher overall complication rate in benign cases, our study is limited by sample size. When evaluating for perforation alone there does not appear to be any significant difference between the two groups. SEMS placement may be a practical option for indications other that malignant obstruction. Interventional endoscopists should be aware and discuss the risk for complications in setting of benign conditions. Indications in these cases should be discussed in a multi-disciplinary fashion with colorectal surgery.
Core Tip: Endoscopic self-expandable metal stent placement remains an underutilized option for malignant and benign colonic obstruction. We retrospectively evaluated sixty three patients with colon malignant obstruction. Fifty five patients had malignant obstruction and 8 had benign colonic obstruction. Procedural success rate was 95% for benign and 100% for malignant obstruction. No difference in complications were noted between and malignant obstruction.
- Citation: Walayat S, Johannes AJ, Benson M, Nelsen E, Akhter A, Kennedy G, Soni A, Reichelderfer M, Pfau P, Gopal D. Outcomes of colon self–expandable metal stents for malignant vs benign indications at a tertiary care center and review of literature. World J Gastrointest Endosc 2023; 15(4): 309-318
- URL: https://www.wjgnet.com/1948-5190/full/v15/i4/309.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i4.309
Self-expandable metal stent (SEMS) placement offers a minimally invasive management option for use in malignant colonic obstruction. SEMS placement can be used both, as definitive therapy for palliation in end stage disease as well as for preoperative management as a bridge to primary surgical anastomosis. In a nationwide analysis of patients with large bowel obstruction only 42.6% of patients underwent prompt intervention, colon stent placement was performed only in 5.4% of patients[1,2]. Multiple previous studies have shown significant success with placement of SEMS for malignant obstruction. A recent meta-analysis of 36 studies showed technical success of 92%, clinical success of 82% in left sided malignant colonic obstruction[3]. Smaller studies have shown similar success rate for right sided lesions with technical and clinical success rates of 92.7% and 90.2%[4-8]. Currently, the European Society of Gastroenterology, SEMS are the preferred therapy for malignant colonic obstructions[9]. The American Society of colon and Rectal surgery also recommend that in patients with incurable disease and obstruction, decompressive stent is preferable to colectomy or diversion while in patients with curable disease stent can be used as a bridge to surgery after discussion of risks and benefits with the patient[10].
While some studies have shown that SEMS can reduce surgical complications including need for stoma formation, length of hospital stay and mortality[11,12]. Others have reported no difference in overall survival, time to progression and disease free survival when compared to emergent surgery[13]. Risk of technical failure has been shown to be higher for longer strictures, strictures in the splenic flexure, extracolonic obstruction and complete obstruction[14]. A randomized controlled trial (RCT) comparing SEMS to surgery found a significantly higher rate of perforation in the SEMS group (60%) and was terminated early[15]. A Cochrane review looking at SEMS placement for malignant obstruction found the procedure to have a perforation rate of 5.88%[16].
Despite all the above supporting data, colon stents continued to remain underutilized as shown in the above mentioned nationwide inpatient sample analysis (performed only in 5.4% of patients)[1]. The aim of this study was to review the procedural and clinical success of both benign and malignant colonic stenting at a tertiary care academic center as well as review the available literature on this topic.
Patients who underwent colonic stenting over an eighteen-year period (August 2004 through August 2022) were identified using an endoscopy database. Internal review board approval was obtained for chart review. Patients were retrospectively reviewed and pertinent information including age, gender, indication (malignant and benign), technical success, clinical success, complications, follow-up length, death and type of surgical procedure and outcomes were recorded.
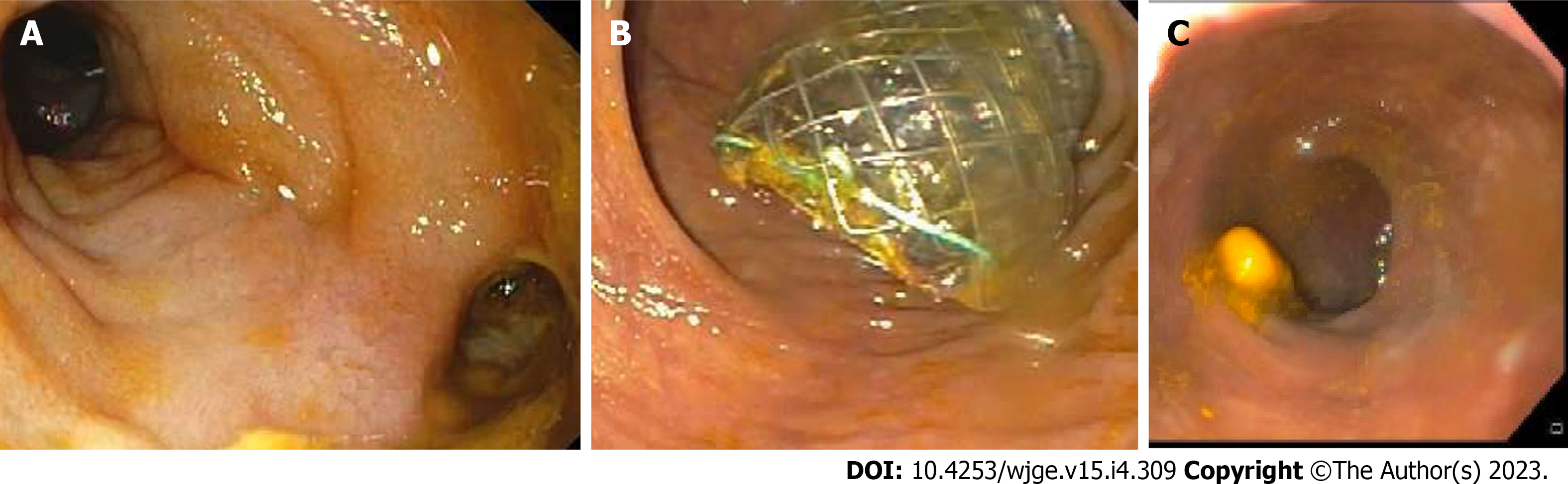
SEMS were all placed under fluoroscopic guidance by one of five interventional advanced endoscopists. Each interventionist in the group had been in practice for at least 5 years. Stents on the left side were placed with Therapeutic Upper Endoscope (GIF 1TH190 series, Olympus America TM) and for those on the right side adult colonoscope was used. For right sided and transverse colon obstruction patients were sedated with the help of anesthesia services using propofol. For left sided obstruction procedures were performed using moderate conscious sedation. For moderate conscious sedation, low dose diphenhydramine (25-50 mg) fentanyl and versed were used. Fluroscopic guidance was used for all procedures. An endoscope was inserted into the rectum and advanced to the point of obstruction. Contrast was injected using a balloon proximal to the tumor to determine the length of the stricture, guide wire was then passed through stricture. The SEMS was then deployed across the stricture over the guide wire under fluoroscopic guidance (Figure 1). Sixty three of the cases were done with Wallflex (Boston Scientific™) stents. Fifty five with a 22 by 90 mm stent and eight with a 22 by 60 mm stent. In one case, an esophageal covered stent was used for an anastomotic fistula (Figure 2) and the distal end was “clipped” to the mucosa to secure its position and prevent migration.
Technical success was defined as endoscopically successful placement of SEMS with evidence of traversing stricture fluoroscopically, and the presence of immediate stool passage. Clinical success was defined as clinical evidence of obstruction relief with passage of stool. Patients with benign strictures who underwent stent placement were felt to be poor surgical candidates, stent placement was performed after review of the case with surgical services. Preoperative bridging success was defined as ability of surgery to be done via laparoscopic approach. Palliative stent success was defined as patients not going on to require a surgical diversion. Major complications including perforations, stent migration and death were recorded. Continuous data are described by mean, standard deviation, and range. Categorical data are presented as numbers and percentages.
Sixty three patients underwent colonic stenting with SEMS over the fourteen-year period. Average age was 65 years old with 66% being female patients. Seventy one percent of colon stents were placed in the sigmoid colon or rectum (Table 1). Fifty five cases were for malignant indications: 23 cases for preoperative bridging and 32 for palliation. Malignant case procedural success was 95% and clinical success was 95%. Complication rate was 1.8% in malignant group. Both the patients with complications had rectal cancer. Complications were related to stent migration in one case, necessitating repeat stenting 7 mo later followed by repeat migration needing stent removal and loop colostomy 7 mo later. Two other patients with rectal cancer needed repeat stent placements in 4-6 mo due to recurrent obstruction secondary to tumor ingrowth. Both of these had sustained clinical remission thereafter. The one patient that did not immediately improve with stent placement, clinically improved that same admission with radiation therapy. Four patients of the 32 patients treated with palliative intent ultimately needed surgery (Table 2). Fifteen of the 23 patient’s treated for preoperative bridging were able to have primary laparoscopic operative resections (Table 3). Of the eight benign indications, four were for diverticular disease associated strictures, two stents were placed for fistula closure, one was for extrinsic fibroid compression, and one stent was placed for ischemic stricture. All benign diseases had procedural success and clinical success. Two of the eight patients had stent migration with one of the patients having a bowel perforation; this was in a patient with a recent PEA arrest who was not a surgical candidate (Table 4).
| Malignant | Benign | Pvalue | |
| Number of cases (total n = 63) | 55 | 8 | |
| Mean age | 63.7 | 67.6 | 0.54 |
| Gender (Male:Female) | 27:36 | 2:6 | |
| Intrinsic vs Extrinsic | 43 vs 12 | 7 vs 1 | |
| Procedure success | 95% | 100% | 1.0 |
| Complication rate | 1.8% | 25% | 0.02 |
| Perforation rate | 0% | 13% | 0.14 |
| Migration rate | 1.8% | 13% | 0.14 |
| Patient | Age | Sex | Tumor location | Technical success | Clincial success | Complications or surgery | Suvival (days) |
| 1 | 77 | M | Sigmoid | Yes | Yes | None | 14 |
| 2 | 71 | M | Sigmoid | Yes | Yes | None | NA |
| 3 | 54 | F | Sigmoid | Yes | Yes | None | 50 |
| 4 | 42 | F | Sigmoid | Yes | Yes | Eventual diversion | NA |
| 5 | 62 | F | Splenic | Yes | Yes | None | NA |
| 6 | 47 | F | Rectum | Yes | Yes | None | 33 |
| 7 | 43 | M | Sigmoid | Yes | Yes | None | 47 |
| 8 | 87 | F | Sigmoid | Yes | Yes | None | NA |
| 9 | 57 | F | Sigmoid | Yes | Yes | None | 85 |
| 10 | 67 | F | Sigmoid | Yes | Yes | None | 354 |
| 11 | 70 | M | Splenic | Yes | Yes | None | 84 |
| 12 | 62 | M | Sigmoid | Yes | Yes | Eventual diversion | NA |
| 13 | 75 | F | Sigmoid | Yes | Yes | None | NA |
| 14 | 54 | M | Rectum | Yes | Yes | None | NA |
| 15 | 42 | F | Splenic | Yes | No | Improved w/XRT | 38 |
| 16 | 54 | F | Sigmoid | No | NA | NA | NA |
| 17 | 46 | M | Sigmoid | Yes | Yes | None | 7 |
| 18 | 43 | M | Sigmoid | Yes | Yes | Repeat stent 12 mo | 689 |
| 19 | 61 | F | Sigmoid | Yes | Yes | None | 21 |
| 20 | 64 | F | Splenic | Yes | Yes | None | 76 |
| 21 | 62 | F | Splenic | Yes | Yes | None | 64 |
| 22 | 52 | F | Sigmoid | Yes | Yes | None | 271 |
| 23 | 87 | M | Sigmoid | Yes | Yes | None | 306 |
| 24 | 44 | M | Sigmoid | Yes | Yes | None | 50 |
| 25 | 61 | F | Rectum | Yes | Yes | Repeat stent 6 mo | 235 |
| 26 | 80 | M | Ascending | Yes | Yes | None | 326 |
| 27 | 66 | M | Transverse | Yes | Yes | None | 454 |
| 28 | 68 | M | Transverse | Yes | Yes | None | 345 |
| 29 | 76 | M | Sigmoid | No | No | None | NA |
| 30 | 76 | M | Ascending | No | No | None | NA |
| 31 | 62 | F | Rectal | Yes | Yes | Repeat stent 4 mo | Open |
| 32 | 64 | M | Rectal | Yes | Yes | Repeat stent in 7 mo, stent migration after 7 mo-removed | 420 |
| Patient | Age | Sex | Tumor location | Technical success | Clincial success | Complications | Surgery type |
| 1 | 86 | M | Sigmoid | Yes | Yes | None | Open |
| 2 | 52 | F | Sigmoid | Yes | Yes | None | Laproscopic |
| 3 | 50 | F | Decending | Yes | Yes | None | Laproscopic |
| 4 | 66 | F | Sigmoid | Yes | Yes | None | Laproscopic |
| 5 | 74 | F | Sigmoid | Yes | Yes | None | Laproscopic |
| 6 | 96 | F | Sigmoid | Yes | Yes | None | Laproscopic |
| 7 | 83 | M | Sigmoid | Yes | Yes | None | Laproscopic |
| 8 | 50 | F | Transverse | Yes | Yes | None | Laproscopic |
| 9 | 48 | M | Sigmiod | Yes | Yes | None | Open |
| 10 | 72 | M | Sigmoid | Yes | Yes | None | Laprascopic |
| 11 | 61 | M | Sigmoid | Yes | Yes | None | Laprascopic |
| 12 | 72 | M | Rectum | Yes | Yes | None | Open |
| 13 | 49 | M | Sigmoid | Yes | Yes | None | Open |
| 14 | 81 | F | Sigmoid | Yes | Yes | None | Open |
| 15 | 68 | F | Rectal | Yes | Yes | None | Open |
| 16 | 81 | M | Transverse | Yes | Yes | None | Laprascopic |
| 17 | 72 | M | Transverse | Yes | Yes | None | Laprascopic |
| 18 | 53 | F | Trasnverse | Yes | Yes | None | Laprascopic |
| 19 | 65 | F | Sigmoid | Yes | Yes | None | Laprascopic |
| 20 | 40 | M | Sigmoid | Yes | Yes | None | Open |
| 21 | 61 | F | Sigmoid | Yes | Yes | None | Laproscopic |
| 22 | 66 | F | Decending | Yes | Yes | None | Open |
| 23 | 86 | M | Splenic | Yes | Yes | None | Laproscopic |
| Patient | Age | Sex | Lesion | Location | Technical success | Clincial success | Complications |
| 1 | 55 | F | Fistula | Sigmoid | Yes | Yes | Migration |
| 2 | 78 | F | Extrinisic compression | Sigmoid | Yes | Yes | Perforation |
| 3 | 76 | F | Diverticular | Sigmoid | Yes | Yes | None |
| 4 | 65 | F | Fistula | Ileocolonic | Yes | Yes | None |
| 5 | 56 | F | Ischemic stricture | Rectum | Yes | Yes | None |
| 6 | 58 | F | Diverticular | Sigmoid | Yes | Yes | None |
| 7 | 66 | M | Diverticular | Sigmoid | Yes | Yes | None |
| 8 | 86 | F | Diverticular | Sigmoid | Yes | Yes | None |
SEMS remain a viable option for colonic obstruction related to malignancy, with our series confirming high technical and clinical success (90.7% and 87.5% respectively). Our clinical and technical success appears to be much higher, a recent review reported risk of technical and clinical failure as high as 25%[2]. Our clinical success is also higher than previously reported by Aerozoo in their RCT (78.6%)[13]. The higher technical and clinical success noted in our case series could be related to colon stent placements being performed only by advanced endoscopist with all of them having five plus years of experience (range 6–30 years of experience) in the field of advanced endoscopy.
In preoperative bridging for malignant obstruction, colonic stenting improves primary surgical outcomes with the majority of these cases performed via a laparoscopic approach (65% of cases). Minimally invasive approaches were considered in 41% of patients by Arezzo et al[13] with laparoscopic success being completed only in 30% of SEMS placement cases[13]. Rate of adverse events, colostomy formation were all higher in the surgery group as compared to anastomotic group in their study[13]. Multiple other studies including a systematic review and a meta-analysis of 7 RCTs have also showed stenting as a bridge to surgery to be beneficial in terms of higher rates or primary anastomosis and decreased rates of stoma formation[17,18]. A recent observational cohort looking 345 patients with acute presentations for CRC, found that when comparing outcomes between stoma formation and stenting, patients undergoing stenting had shorter hospital stays, were able to be discharged home and had similar or fewer complications[19]. There were no complications noted in the patients who underwent stent placement as a bridge to surgery in our cohort.
In patients undergoing stent placement for palliative purposes our technical and clinical success was slightly lower than those previously reported. Our technical and clinical success rate was 90.7%. In three patients with malignant obstruction, we were unable to safely deploy a stent. The reason for this fail deployment were multifactorial including complete obstruction leading to inability to pass the guide wire, tortuosity of colon at the point of obstruction limiting guide wire passage, failure to reach the area of obstruction in the setting of poor prep. One patient had technical success with failed improvement of symptoms initially however later symptoms improved with radiation therapy. There are multiple studies showing the success and safety of colonic SEMS for palliation of stage IV colon cancer. One of the largest series had a technical and clinical success rates of 96% and 99%, respectively[20]. Our study demonstrated good technical and clinical success rates and few patients went on to require diversion surgeries (2/32). More recently a meta-analysis of palliative stenting showed shorter time to chemotherapy and lower 30 day mortality[21]. Quality of life has been shown to be improved following colonic stenting for palliative intent[22]. While survival may depend on multiple factor including stage of the disease at time of diagnosis, patient ECOG status, tolerance and response to chemotherapies and other comorboidities. Data for survival was available in 21 patients. The mean survival post stenting was 189 days in our cohort (ranging from 7-689 d). Four patients needed repeat stent placement, 3 of these had rectal tumor while one had sigmoid tumor.
Colonic perforation remains of high concern when placing SEMS. While our series only included one perforation (1.7% perforation rate) other studies have shown a much higher rate. The perforation noted in our cohort was in the group who underwent stent placement for benign indication. One RCT comparing SEMS to surgery found a significantly higher rate of perforation in the SEMS group (60%) and was terminated early[15]. However, another RCT was also terminated early due to a higher mortality in the surgical group compared to the stent group[23]. The majority of studies looking at SEMS placement for malignant obstruction found the procedure to be safe and highly effective with a Cochrane review showing a perforation rate of 5.88%[16]. More recently a meta-analysis looking at perforation risk showed the rate to be 7.4%[24]. Providers should be aware of this risk and be able to provide appropriate informed consent. One particular risk is that of patients on bevacizumab. One study showed that bevacizumab therapy nearly tripled the risk of perforation[20]; while another study showed that bevacizumab therapy increased the risk of perforation by 19.6-fold[25]. More recently a meta-analysis confirmed the risk of perforation for patients on bevacizumab[24]. Chemotherapy agents should be reviewed prior to stent placement for palliation and bevacizumab should be considered a contraindication to SEMS placement. Other than perforation and re-obstruction risks, providers should be aware of other side effects including pain, tenesmus, incontinence and fistula formation[23].
While per literature review the indications and outcomes for malignant obstruction seem clearer, data on benign indications seems limited. Our series had only 8 patients who underwent stent placement for benign indications. In our series, benign indications for SEMS placement appears to have similar success as malignant, however there are significantly higher rates of complication when compared to malignant group (25% in benign group vs 1.8% in malignant group (P = 0.02). One patient had stent migration while one had perforation. This risk of migration has also been shown in other series that included benign disease[8,25,26]. A systematic review showed that complication rates are high for benign disease with a perforation rate of 12% and a re-obstruction rate of 14%[27]. Complications for benign indications seem to occur more often if surgical interventions are delayed with one study showing the risk significantly higher if surgery was not performed within 7 d of stent placement[16,28]. Another series showed similarly high risk of complication, especially in diverticular strictures; authors recommended surgery within a month to avoid such complications[29]. Currently there is not enough data to support routine placement of SEMS for benign indications. If SEMS are placed for bridging, surgery should be done within a week to avoid serious complications[30]. Our series included successful treatment of an anastomotic fistula with use of a fully covered esophageal stent. This was after an attempt at fistula closer with over and thru the scope clips which were unsuccessful given likely post-surgical anastomotic fibrosis. Other series have used covered esophageal stents for fistulas with success. This use is off label, and providers should be aware of the migration risk. More recently, a larger retrospective study of 126 patients found that colonic stenting in acute large-bowel obstruction was more likely to be successful in shorter, malignant strictures than with longer, benign strictures which were associated with an increased risk of perforation[31].
The limitations of this study are inherent to its retrospective nature and small sample size especially for benign disease. Despite this study being completed at a tertiary center, there were only sixty three cases completed over an eighteen-year period. This also reflects the likely underutilization of colon stenting in cases of malignant obstruction. Our results show that the colonic stenting can be performed with high success even in centers with low number of cases per year. Larger multi center studies are needed especially regarding the use of colon stents for benign colonic strictures and their outcomes.
Gastroenterologists, internists and surgeons should remain aware that colon stent is a safe and effective option for malignant obstruction and may improve surgical outcomes. They remain a worthwhile option for both palliative and preoperative indications in patients with malignant obstructions. Preoperative bridging needs further investigation into the long term risk of recurrence of disease. Benign indications for SEMS placement appear to have similar success however there was a high rate of stent migration and perforation, our study was however limited by sample size to draw further concrete conclusions. Further larger prospective multi center trails are needed to shed light on the use of colon stent placement especially for benign indications.
Colon obstruction due to benign and malignant etiologies at our tertiary care center is a fairly common problem however the wide spread use of colon stent is limited nationally with a nationwide analysis showing only 5.4% of patients with colon obstruction undergoing stent placement.
This under-utilization of colon stents for patient with colon obstruction prompted us to study the outcomes of patient undergoing colon stent placement for malignant and benign etiologies.
The objective of this study was to review long- and short-term clinical success of self-expandable metal stent (SEMS) use for colonic obstruction at a tertiary care center.
We retrospectively reviewed all the patients who underwent colonic SEMS placement over an eighteen year period (August 2004 through August 2022) at our academic center.
Sixty three patients underwent colon SEMS over an 18-year period. Fifty-five cases were for malignant indications, 8 were for benign conditions. The total malignant case (n = 55) procedural success rate was 95% vs 100% for benign cases (P = 1.0, NS). Overall complication rate was significantly higher for benign group: Four complications were observed in the malignant group (stent migration, restenosis) vs 2 of 8 (25%) for benign obstruction (1-perforation, 1-stent migration) (P = 0.02).
SEMS remain a worthwhile option for both palliative and preoperative indications in patients with malignant obstructions. Benign indications for SEMS placement appear to have similar success however there was a high rate of stent migration and perforation, our study was however limited by sample size to draw further concrete conclusions.
Preoperative bridging needs further investigation into the long term risk of recurrence of disease. Further larger prospective multi center trails are needed to shed light on the use of colon stent placement especially for benign indications.
| 1. | Kwaan MR, Wu Y, Ren Y, Xirasagar S. Prompt intervention in large bowel obstruction management: A Nationwide Inpatient Sample analysis. Am J Surg. 2022;224:1262-1266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 2. | Lueders A, Ong G, Davis P, Weyerbacher J, Saxe J. Colonic stenting for malignant obstructions-A review of current indications and outcomes. Am J Surg. 2022;224:217-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 3. | Neo VSQ, Jain SR, Yeo JW, Ng CH, Gan TRX, Tan E, Chong CS. Controversies of colonic stenting in obstructive left colorectal cancer: a critical analysis with meta-analysis and meta-regression. Int J Colorectal Dis. 2021;36:689-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Amelung FJ, Draaisma WA, Consten ECJ, Siersema PD, Ter Borg F. Self-expandable metal stent placement versus emergency resection for malignant proximal colon obstructions. Surg Endosc. 2017;31:4532-4541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M. Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol. 2004;99:2051-2057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 504] [Cited by in RCA: 413] [Article Influence: 18.8] [Reference Citation Analysis (1)] |
| 6. | Meisner S, Hensler M, Knop FK, West F, Wille-Jørgensen P. Self-expanding metal stents for colonic obstruction: experiences from 104 procedures in a single center. Dis Colon Rectum. 2004;47:444-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 112] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 7. | Bielawska B, Hookey LC, Jalink D. Large-diameter self-expanding metal stents appear to be safe and effective for malignant colonic obstruction with and without concurrent use of chemotherapy. Surg Endosc. 2010;24:2814-2821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Saida Y, Enomoto T, Takabayashi K, Otsuji A, Nakamura Y, Nagao J, Kusachi S. Outcome of 141 cases of self-expandable metallic stent placements for malignant and benign colorectal strictures in a single center. Surg Endosc. 2011;25:1748-1752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | van Hooft JE, van Halsema EE, Vanbiervliet G, Beets-Tan RG, DeWitt JM, Donnellan F, Dumonceau JM, Glynne-Jones RG, Hassan C, Jiménez-Perez J, Meisner S, Muthusamy VR, Parker MC, Regimbeau JM, Sabbagh C, Sagar J, Tanis PJ, Vandervoort J, Webster GJ, Manes G, Barthet MA, Repici A; European Society of Gastrointestinal Endoscopy. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2014;46:990-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 223] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 10. | Vogel JD, Eskicioglu C, Weiser MR, Feingold DL, Steele SR. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Treatment of Colon Cancer. Dis Colon Rectum. 2017;60:999-1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 239] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 11. | Tilney HS, Lovegrove RE, Purkayastha S, Sains PS, Weston-Petrides GK, Darzi AW, Tekkis PP, Heriot AG. Comparison of colonic stenting and open surgery for malignant large bowel obstruction. Surg Endosc. 2007;21:225-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 150] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 12. | Xinopoulos D, Dimitroulopoulos D, Theodosopoulos T, Tsamakidis K, Bitsakou G, Plataniotis G, Gontikakis M, Kontis M, Paraskevas I, Vassilobpoulos P, Paraskevas E. Stenting or stoma creation for patients with inoperable malignant colonic obstructions? Surg Endosc. 2004;18:421-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 142] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 13. | Arezzo A, Forcignanò E, Bonino MA, Balagué C, Targarona E, Borghi F, Giraudo G, Ghezzo L, Passera R, Morino M; collaborative ESCO study group. Long-term Oncologic Results After Stenting as a Bridge to Surgery Versus Emergency Surgery for Malignant Left-sided Colonic Obstruction: A Multicenter Randomized Controlled Trial (ESCO Trial). Ann Surg. 2020;272:703-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 14. | Köhler G, Antoniou SA, Lechner M, Mayer F, Mair J, Emmanuel K. Stenting for Emergency Colorectal Obstruction: An Analysis of 204 Patients in Relation to Predictors of Failure and Complications. Scand J Surg. 2015;104:146-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | van Hooft JE, Fockens P, Marinelli AW, Timmer R, van Berkel AM, Bossuyt PM, Bemelman WA; Dutch Colorectal Stent Group. Early closure of a multicenter randomized clinical trial of endoscopic stenting versus surgery for stage IV left-sided colorectal cancer. Endoscopy. 2008;40:184-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 213] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 16. | Sagar J. Colorectal stents for the management of malignant colonic obstructions. Cochrane Database Syst Rev. 2011;2011:CD007378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 86] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 17. | Cirocchi R, Farinella E, Trastulli S, Desiderio J, Listorti C, Boselli C, Parisi A, Noya G, Sagar J. Safety and efficacy of endoscopic colonic stenting as a bridge to surgery in the management of intestinal obstruction due to left colon and rectal cancer: a systematic review and meta-analysis. Surg Oncol. 2013;22:14-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 143] [Article Influence: 11.0] [Reference Citation Analysis (2)] |
| 18. | Ye GY, Cui Z, Chen L, Zhong M. Colonic stenting vs emergent surgery for acute left-sided malignant colonic obstruction: a systematic review and meta-analysis. World J Gastroenterol. 2012;18:5608-5615. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 39] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Abelson JS, Yeo HL, Mao J, Milsom JW, Sedrakyan A. Long-term Postprocedural Outcomes of Palliative Emergency Stenting vs Stoma in Malignant Large-Bowel Obstruction. JAMA Surg. 2017;152:429-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 20. | Small AJ, Coelho-Prabhu N, Baron TH. Endoscopic placement of self-expandable metal stents for malignant colonic obstruction: long-term outcomes and complication factors. Gastrointest Endosc. 2010;71:560-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 209] [Article Influence: 13.1] [Reference Citation Analysis (2)] |
| 21. | Zhao XD, Cai BB, Cao RS, Shi RH. Palliative treatment for incurable malignant colorectal obstructions: a meta-analysis. World J Gastroenterol. 2013;19:5565-5574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 111] [Cited by in RCA: 104] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 22. | Nagula S, Ishill N, Nash C, Markowitz AJ, Schattner MA, Temple L, Weiser MR, Thaler HT, Zauber A, Gerdes H. Quality of life and symptom control after stent placement or surgical palliation of malignant colorectal obstruction. J Am Coll Surg. 2010;210:45-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 62] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 23. | Alcántara M, Serra-Aracil X, Falcó J, Mora L, Bombardó J, Navarro S. Prospective, controlled, randomized study of intraoperative colonic lavage versus stent placement in obstructive left-sided colonic cancer. World J Surg. 2011;35:1904-1910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 155] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 24. | van Halsema EE, van Hooft JE, Small AJ, Baron TH, García-Cano J, Cheon JH, Lee MS, Kwon SH, Mucci-Hennekinne S, Fockens P, Dijkgraaf MG, Repici A. Perforation in colorectal stenting: a meta-analysis and a search for risk factors. Gastrointest Endosc. 2014;79:970-82.e7; quiz 983.e2, 983.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 109] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 25. | Manes G, de Bellis M, Fuccio L, Repici A, Masci E, Ardizzone S, Mangiavillano B, Carlino A, Rossi GB, Occhipinti P, Cennamo V. Endoscopic palliation in patients with incurable malignant colorectal obstruction by means of self-expanding metal stent: analysis of results and predictors of outcomes in a large multicenter series. Arch Surg. 2011;146:1157-1162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 90] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 26. | Suzuki N, Saunders BP, Thomas-Gibson S, Akle C, Marshall M, Halligan S. Colorectal stenting for malignant and benign disease: outcomes in colorectal stenting. Dis Colon Rectum. 2004;47:1201-1207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 99] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 27. | Currie A, Christmas C, Aldean H, Mobasheri M, Bloom IT. Systematic review of self-expanding stents in the management of benign colorectal obstruction. Colorectal Dis. 2014;16:239-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (1)] |
| 28. | Small AJ, Young-Fadok TM, Baron TH. Expandable metal stent placement for benign colorectal obstruction: outcomes for 23 cases. Surg Endosc. 2008;22:454-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 102] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 29. | Keränen I, Lepistö A, Udd M, Halttunen J, Kylänpää L. Outcome of patients after endoluminal stent placement for benign colorectal obstruction. Scand J Gastroenterol. 2010;45:725-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 30. | Bonin EA, Baron TH. Update on the indications and use of colonic stents. Curr Gastroenterol Rep. 2010;12:374-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 31. | Boyle DJ, Thorn C, Saini A, Elton C, Atkin GK, Mitchell IC, Lotzof K, Marcus A, Mathur P. Predictive factors for successful colonic stenting in acute large-bowel obstruction: a 15-year cohort analysis. Dis Colon Rectum. 2015;58:358-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Nakaji K, Japan; Tan Y, China S-Editor: Fan JR L-Editor: A P-Editor: Cai YX