Published online Mar 16, 2023. doi: 10.4253/wjge.v15.i3.84
Peer-review started: October 27, 2022
First decision: December 12, 2022
Revised: January 15, 2023
Accepted: February 8, 2023
Article in press: February 8, 2023
Published online: March 16, 2023
Processing time: 139 Days and 14.4 Hours
Gastroesophageal reflux (GER) in children is very common and refers to the in
Core Tip: Gastroesophageal reflux disease (GERD) is a pathologic process requiring prompt assessment and treatment. The manifestations of GERD, especially in young children vary making it a challenge to diagnose. Combined esophageal pH-MII manometry has increased the diagnostic accuracy of GERD and helped explain its pathogenesis. Medication should be targeted to the underlying GERD pathogenesis, if known, and to minimize complications.
- Citation: Sintusek P, Mutalib M, Thapar N. Gastroesophageal reflux disease in children: What’s new right now? World J Gastrointest Endosc 2023; 15(3): 84-102
- URL: https://www.wjgnet.com/1948-5190/full/v15/i3/84.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i3.84
A combined guideline of the European and the North American Societies for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN and NAPSPGHAN respectively)[1], defined gastroesophageal reflux (GER) as the passage of gastric contents into the esophagus with or without regurgitation and vomiting and GER disease (GERD) where GER leads to troublesome symptoms that affect daily functioning and/or leads to clinical complications within the esophagus or other systems. As the clinical symptoms and signs of GERD are variable and nonspecific especially in infants and young children, it is often difficult to make a diagnosis on the basis of history or physical examination alone. Furthermore, other significant disorders that mimic GERD may need urgent attention and will need to be considered and excluded.
The prevalence of GERD varies across studies depending on the diagnostic criteria used and the study design. A systematic review published in 2019 demonstrated that the overall pooled prevalence of GERD symptoms from 4 cross-sectional studies, was 26.9% [95% confidence interval (CI) 20.1-33.7, I2: 6.83][2]; However, the prevalence of GERD in infants, across a number of prospective studies, tends to decrease with time from 25.5%[3] at the age of 1 mo and 26.5%[4] at the age of 6 wk to 7.7%[4] at age 3 mo, 2.6%[4] and 2.9%[3] at the age of 6 mo to only 1.1%[4] and 1.6%[5] at the age of 12 mo. An ex
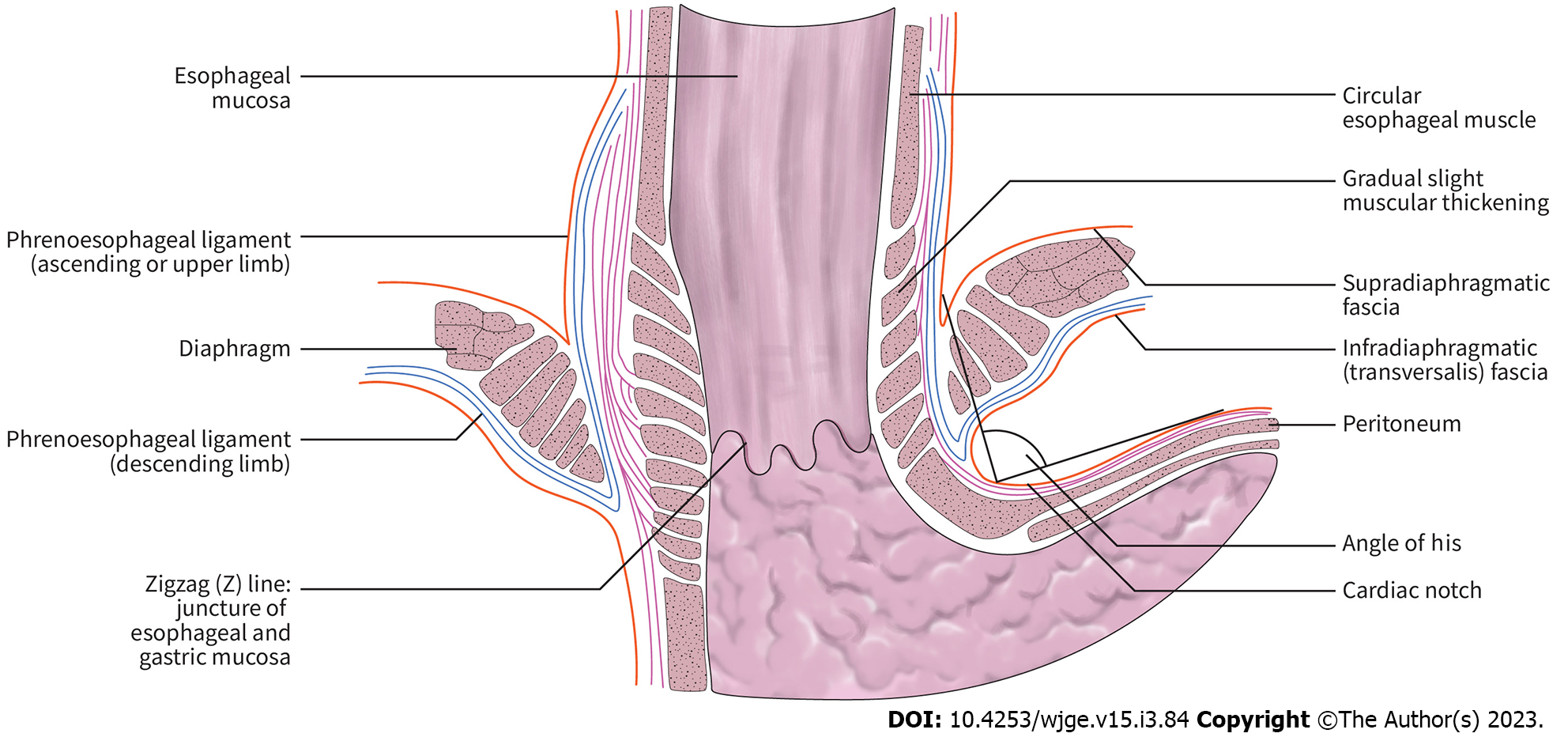
The main pathogenesis of GERD in children, as in adults, is abnormal transient lower esophageal sphincter relaxation (TLESR). Other factors implicated in the pathogenesis of GERD[16] include the anatomy and integrity of the antireflux barrier, as well as those affecting esophageal peristalsis and clearance (Table 1 and Figure 1).
| Main underlying mechanism | Associated conditions | Mechanism of GERD |
| Anatomical defect | Hiatus hernia, immature esophageal anti-relux barrier, e.g., infants, surgical pull up for esophageal atresia | Increased risk of GER |
| Esophageal or gastric hypomotility/dysmotility | Esophageal disorders associated with dysmotility, e.g., esophageal atresia, achalasia, gastroparesis, cow’s milk protein allergy, sleeping, decreased saliva secretion, supine position | Impaired esophageal clearance of refluxate by peristalsis and/or production of neutralizing secretions |
| Esophageal mucosal defect | Eosinophilic esophagitis, esophageal infection | Impaired esophageal sensation |
| UES dysfunction | Extraesophageal or respiratory manifestations | Allows refluxate to access airways |
The lower esophageal sphincter (LES) pressure tends to increase in infants with increasing gestational age[17-19]. In normality, LES relaxation follows swallowing or primary peristalsis of the esophagus. However, TLESR or a relaxation of the LES that is not preceded by swallowing can also occur leading to pathologic reflux. TLESR can be stimulated by increasing intraesophageal pressure as a result of crying, gastric distension and respiratory diseases. TLESR can be demonstrated in infants from the gestational age of 28 wks[18,19]. Interestingly, many studies have shown that TLESR do not occur more in patients with GERD compared to healthy persons[18,20]. Patients with GERD are more likely to have acid reflux compared to normal persons, which might explain this finding[21,22]. In addition, the failure of one or more of several protective mechanisms, detailed below, can also contribute to the pathogenesis of GERD.
The antireflux barrier consists of the LES, the diaphragmatic pinchcock and angle of His (Figure 1). The LES a 1-2 cm high pressure zone located at the junction between the esophagus and the stomach and is comprised of intrinsic (lower esophageal muscle fibers) and extrinsic components (oblique sling muscle fibers from the stomach and musculofacial sling from the diaphragm). This is further supported by a short length of intra-abdominal esophagus as well as the angle of His or esophagogastric angle, the acute angle formed between the cardia and abdominal part of LES[23]. This composite anti-reflux barrier acts in normality as a physiologic sphincter between the high stomach (intra-abdominal) pressure compared to the lower pressure in the esophagus (intra-thoracic) and thus to prevent the regurgitation of gastric contents along the pressure gradient into the esophagus.
In infants, alongside TLESRs, underdevelopment of the abdominal part of the LES and angle of His are likely to explain the high prevalence of GERD in the infantile period[24,25]. Where a hiatal hernia is present in patients, the separation of the LES and the crural diaphragm acts to significantly impair the antireflux barrier and contribute to the increase in acid exposure of the esophagus and GERD.
To prevent esophageal mucosal injury from the movement of gastric contents into esophagus after LES relaxation, secondary esophageal peristalsis with clearance of the refluxate back into the stomach is considered a main protective mechanism. Moreover, an upright position can further help volume clearance by gravity. Apart from mechanical clearance, the acid content of any refluxate can be neutralized by both swallowed saliva and esophageal secretions. In infants, volume clearance is less effective due to their mostly recumbent position. During sleep, the reduced frequency of primary and secondary esophageal peristalsis may contribute to precipitate GERD[1,16]. Any disorder that primarily (e.g., esophageal atresia, achalasia) or secondarily (esophagitis) affects oesophageal motility may increase the predisposition to GERD[26-29]. Moreover, delayed gastric emptying or gastroparesis, often a transient phenomenon in children after infection, can cause postprandial reflux from gastric distension stimulating LES relaxation[30].
Interestingly, a postprandial acid pocket phenomenon has been well described by Fletcher et al[31] They describe a floating “pocket” of an unbuffered reservoir of gastric acid that may become exposed to the esophagus during LES relaxation. The role of the acid pocket in the pathogenesis of GERD has been reported but limited to adult studies[32,33].
In addition, esophageal mucosal defense may be compromised in a number of conditions such as esophagitis from eosinophilic or other inflammatory diseases as well as infections. A defect in esophageal mucosal defense can lead to esophageal dysmotility and reflux esophagitis can be superimposed. As the esophageal mucosa contains receptors sensitive to acid, temperature and volume, their destruction in severe esophagitis might explain the hyposensitivity with reflux injury in children with Barrett esophagus and corrected esophageal atresia[34]. A high index of suspicion and intensive evaluation and monitoring, including with histopathology of esophagus, are needed in such patients.
In extraesophageal manifestation of GERD, such as upper airway diseases or ENT problems, there are many proposed pathways such as GER induced vagally mediated aspiration or insufficiency of upper esophageal sphincter (UES) function[24,34-38].
The manifestations of GERD can vary from an asymptomatic presentation or non-specific symptoms such as irritability in infants, frequent vomiting, failure to thrive, unexplained anemia, difficult to treat respiratory symptoms through to more specific ones such as heartburn in older children. However, a high index of suspicion or the presence of alarm features, may require early investigation to either exclude other mimickers or confirm the diagnosis of GERD (Table 2).
| Symptoms | Signs | Red flags from other serious conditions that may underlie or mimic GERD |
| General | General | General |
| Irritability | Dental erosion, not dental caries (Figure 2) | Excessive irritability |
| Failure to thrive | Anemia | Weight loss |
| Feeding refusal | Fever | |
| Sandifer syndrome | Lethargy | |
| Gastrointestinal | Gastrointestinal | Gastrointestinal |
| Recurrent regurgitation | Esophagitis | Onset of regurgitation at > 6 mo of age |
| Recurrent vomiting | Esophageal stricture | Persistent or progressive regurgitation at > 1 yr of age |
| Heartburn | Barrett esophagus | Vomiting: Persistent forceful, nocturnal or bilious vomiting |
| Dysphagia/odynophagia | Hematemesis | |
| Epigastric pain | Marked abdominal distension | |
| Airway | Airway | Neurological |
| Difficult to treat wheezing | Apnea | Bulging fontanelle |
| Unexplained stridor | Recurrent pneumonia | Seizure |
| Chronic cough | Recurrent otitis media | Macro/microcephaly |
| Hoarseness of voice | Neurological abnormalities | |
| Papilledema |
There has been no single gold standard tool to diagnose GERD in children. In practice, therapeutic trials of medication and follow-up can be considered in older children with a typical presentation of GERD such as heartburn but these may not reliable in infants[39]. If there is no response after an 8-week trial of PPI or in the presence of alarm features, investigations are necessary to confirm or rule out GERD. The major limitation of all diagnostic tools is that the normal values for each parameter are not well established in infants and children. A number of investigations have been used to distinguish GERD from other worrisome disorders that mimic GERD.
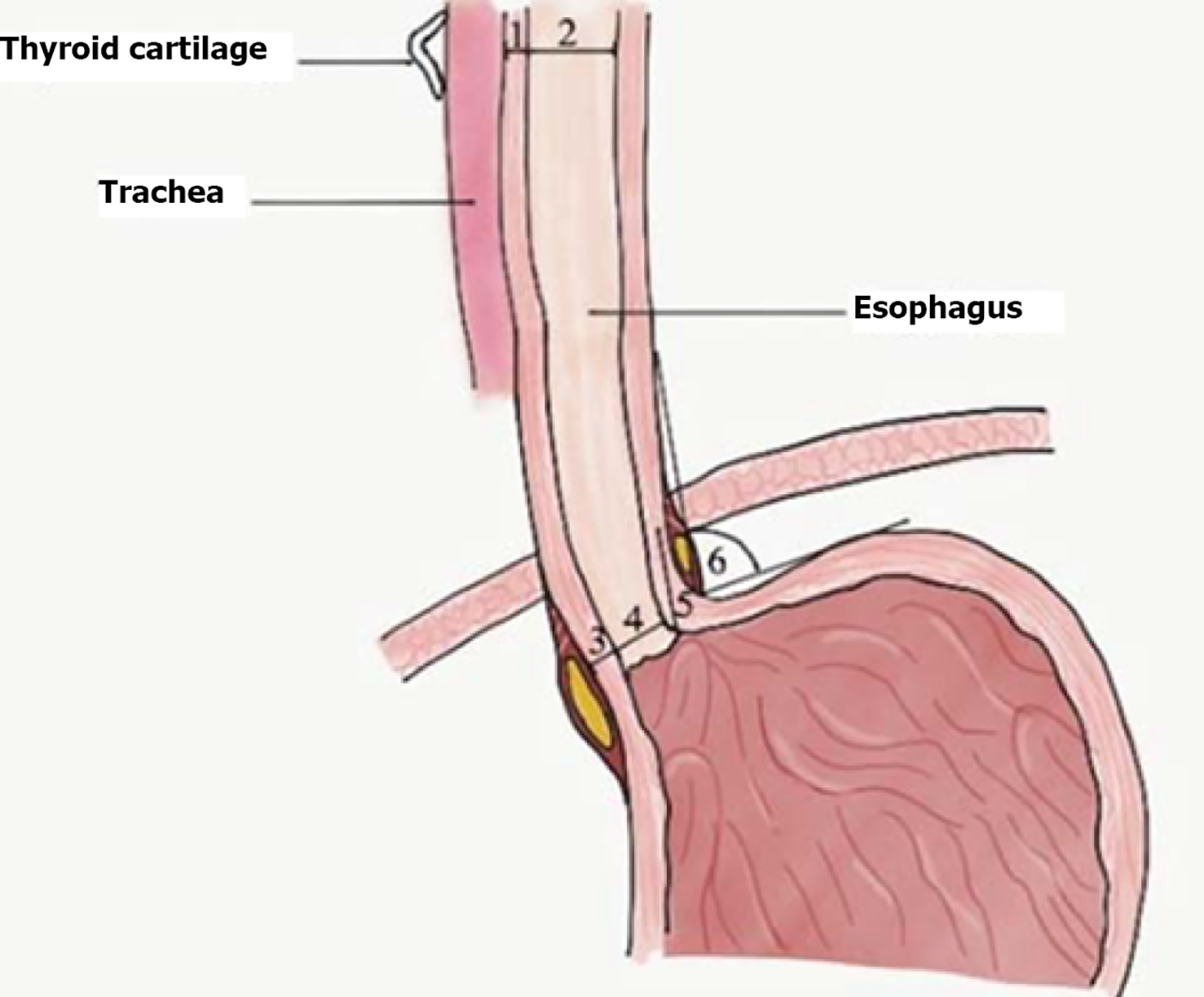
Ultrasound has high sensitivity and positive predictive value for GERD as it can assess both the anatomy of the esophagus and real-time reflux. It is a non-invasive tool with some evidence-based studies supporting its fair sensitivity (76%-100%) and specificity (50%-100%) compared to pH studies[40-43]. A study noted the presence of a shorter abdominal esophageal length, increased cervical and abdominal esophageal wall thickness, diameter and angle of His in Thai children diagnosed with GERD (n = 22, median age of 1.6 years) compared with healthy children (n = 23), however, these differences failed to reach statistical significance[44] (Figure 3). Moreover, the reliability of the test depends on the individual experience of the radiologist[45].
Barium (contrast) swallow and upper gastrointestinal studies (meal ± follow through) are used to evaluate anatomical abnormalities of esophagus, stomach and proximal small bowel such as tracheoesophageal fistula, achalasia, hiatus hernia, midgut malrotation ± intermittent volvulus. Furthermore, the barium study can roughly evaluate the transit time of esophagus and stomach but lacks standardized protocols and normal values. Although, episodes of reflux are commonly observed during these procedures, there is poor correlation with an abnormal reflux index from a 24-h pH study[46]. Overall, such contrast studies are neither sensitive nor specific tests for GER or GERD and should not be used for diagnosis.
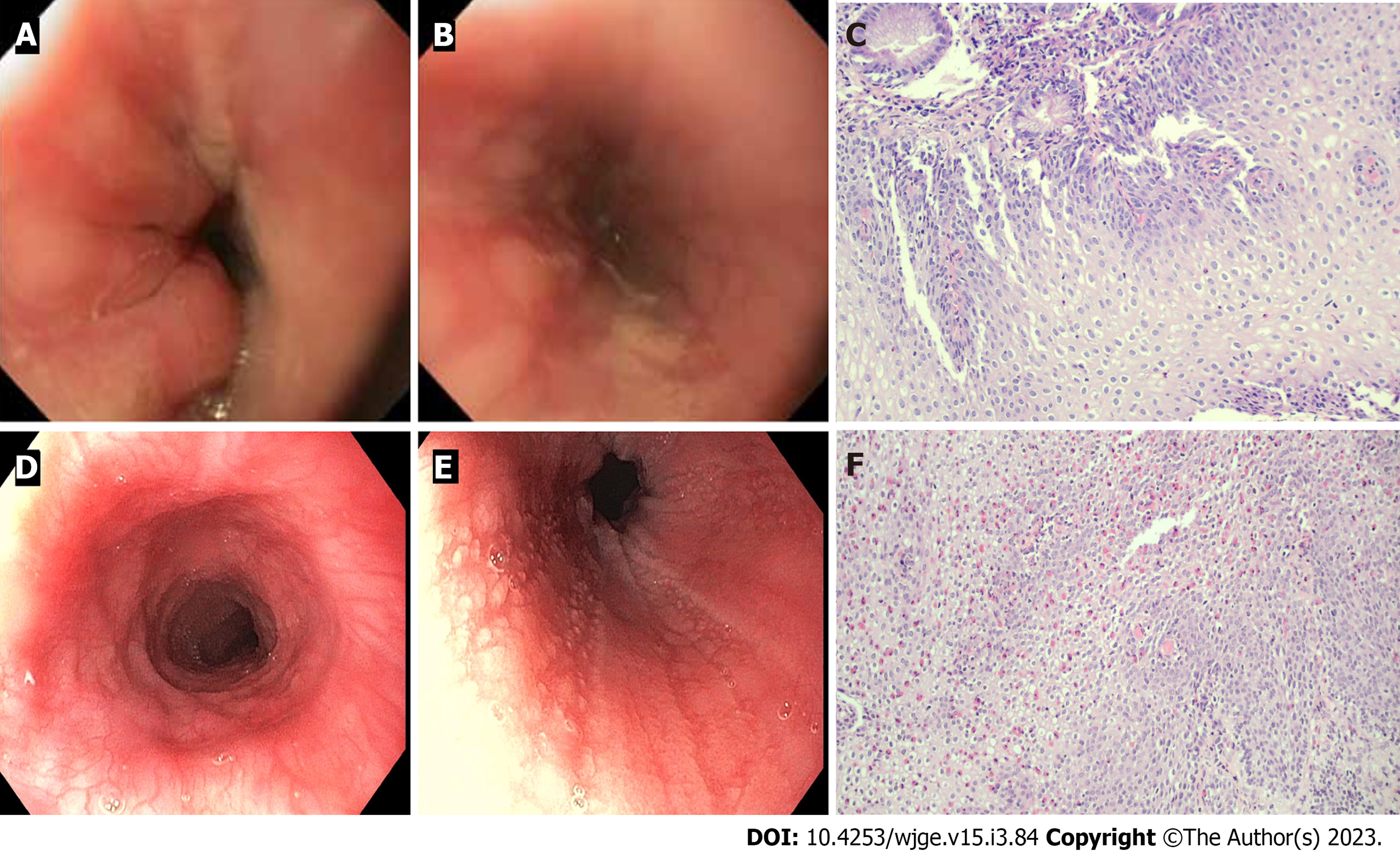
Endoscopy is generally utilized where esophagitis is suspected in patients with significant clinical issues such as recurrent vomiting, unexplained anemia, hematemesis, positive stool occult blood or high-risk groups (corrected esophageal atresia, eosinophilic esophagitis, immunocompromised hosts that are prone to have esophageal infection). Eosinophilic esophagitis and eosinophilic gastrointestinal disease can present with symptoms and signs similar to that of GERD and its diagnosis requires histopathology of esophageal tissue (Figure 4). Clinicians should be aware that severe esophagitis in GERD rarely presents with pain[34] and there is a poor correlation between the severity of symptoms and presence or severity of esophagitis. In children with extraesophageal symptoms such as cough and wheezing, up to one third had microscopic esophagitis[47], suggesting endoscopy may also have a role in children with extraesophageal symptoms.
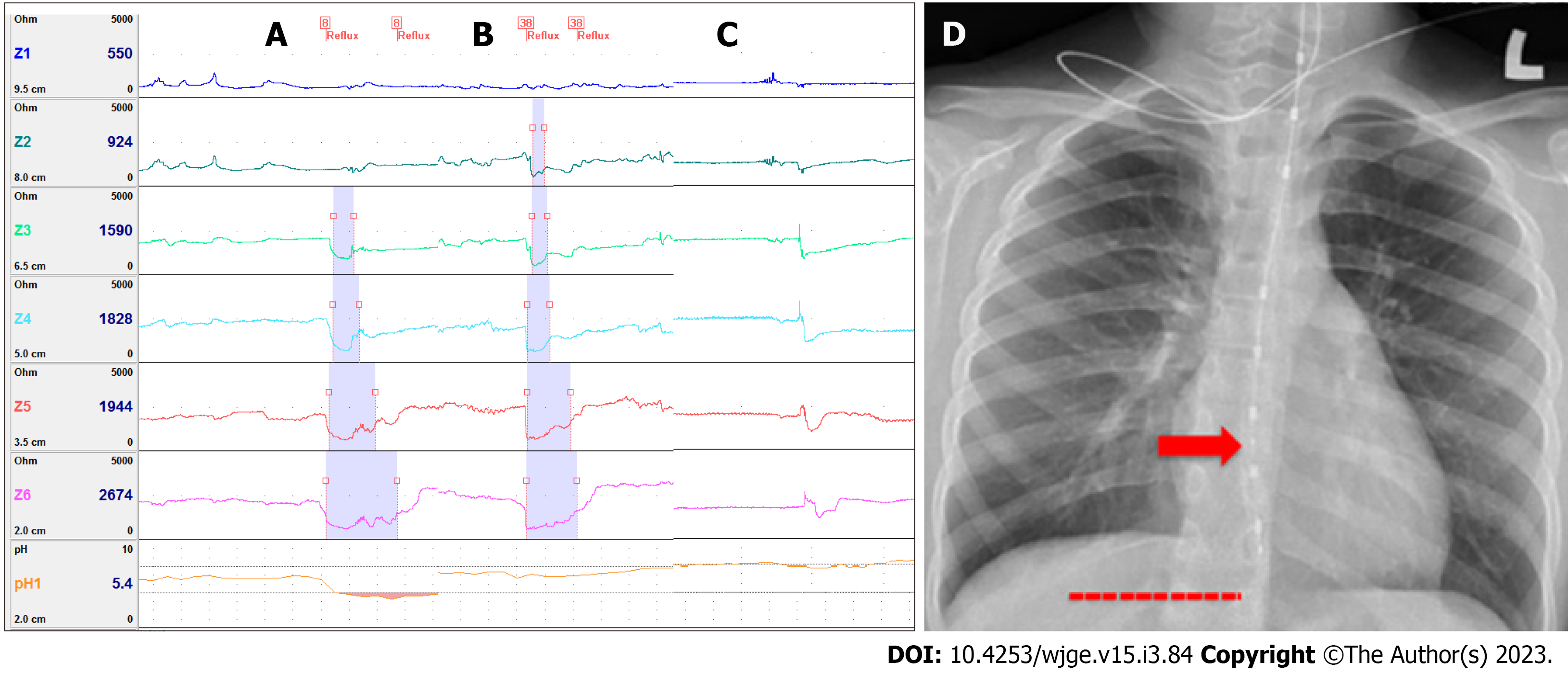
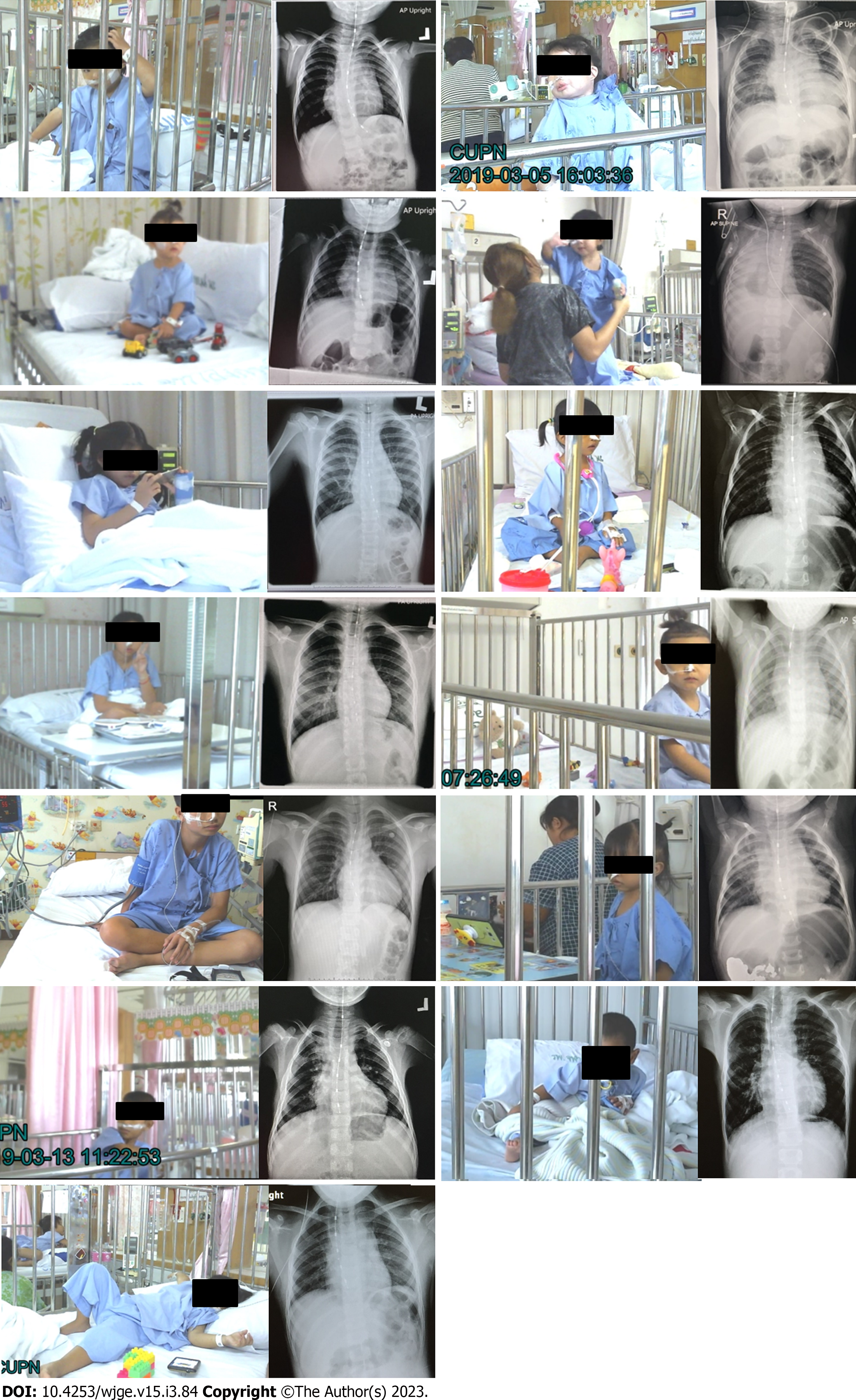
The pH-monitoring test has largely been replaced with MII-pH monitoring that can provide more data not only of acid reflux but also of other types (weakly acid, nonacid, liquid or air) as well as the proximal extent of reflux (Figure 5). However, pH-monitoring does retain value especially with regards to wireless pH recording, that minimizes disruption of patients during monitoring and allows for prolonged assessment of up to 5 days[48,49]. Similar to other diagnostic tools for GERD in children, there remains a lack of normal values hence the results of the test should be interpreted with caution. The most recent combined ESPGHAN- NAPSPGHAN guidelines recommend using the MII-pH study to correlate persistent troublesome symptoms with reflux episodes[1]. Recently, researchers have reported enhancements of the technique such as the use of combined VDO-MII-pH studies (Figure 6) in high-risk children with corrected esophageal atresia. Many children with corrected esophageal atresia may develop reflux esophagitis without specific symptoms or signs, however, Maholarnkij et al[6] found a trend of specific symptom that associated with reflux by using real-time Video recording and MII-pH monitoring. In this study, vomiting, irritability or unexplained crying and cough were the most common symptoms associated with reflux during combined Video-MII-pH monitoring. Hence, this novel tool might help the clinicians to diagnose GERD by increasing the symptom association index from MII-pH monitoring.
UES dysfunction is thought to represent a major factor underlying the pathogenesis of the extraesophageal symptoms of GERD. Oropharyngeal pH monitoring should, in theory, detect abnormal acid reflux in this area and thus the cause of such symptoms. However, studies to date report conflicting results regarding the correlation of oropharyngeal pH monitoring and full-column reflux episodes detected by pH-impedance monitoring[50-56]. These studies were limited by small numbers of participants as well as equipment available to measure the pH above the LES and at the UES in children. The linkage of acid reflux from below the LES to that above the UES may have been impacted by the longer frequency used to detect acid in the proximally implanted Dx-pH probe (every 0.50 s) compared to the distal MII-pH recording (every 0.02 s)[52]. There is no connection between oropharyngeal pH events and pH-impedance events, according to a systematic review in adults[53]. Moreover, there were no significant differences in oropharyngeal acid exposure between PPI responders, partial responders and nonresponders in adult patients with laryngeal symptoms[54-56].
Esophageal manometry can help clarify the role of esophageal dysmotility leading to ineffective esophageal clearance in the pathophysiology of reflux. It is, however, an invasive test that relies on cooperation from children undergoing the studies[57-59].
In a study by van Lennep et al[60], even though esophageal manometry with or without 24-h pH impedance study was successfully completed in children (> 90%), complete interpretation is limited in children under the age of 4.
Esophageal manometry with pH-MII monitoring has a potential role in the assessment of extraesophageal symptoms such as aspiration pneumonia from esophageal stasis[1], or to improve the cough-reflux correlation[61].
Electrogastrography (EGG) is a noninvasive test to study the electrophysiology of stomach, and in turn assess for the presence of gastroparesis or gastric hypomotility as potential pathogenic factors for GERD[59,62]. Studies suggest significantly higher pooled prevalences of EGG abnormalities in GERD patients compared to healthy adults[63] and children[64]. However, the protocol and techniques for EGG studies are quite variable between centers.
Due to the limitations of current investigative procedures used to diagnose extraesophageal manifestations of GERD, biomarkers have been proposed for use in diagnosing this type of GERD. Studies have suggested using of pepsin, lipid-laden macrophages and, bilirubin[65-71]. However, their diagnostic efficacy has not been established, and most call for invasive procedures like bronchoscopy to get the necessary samples, which restricts their application.
Studies to support the role of diagnostic trials of PPI and transpyloric feeding in children are scarce[72,73]. Trials of transpyloric feeding to confirm GERD are not specific given improvements in symptoms of vomiting or feeding intolerance may also be seen in mimickers of GERD such as severe gastroparesis[74].
In GER, non-pharmacological treatments and close follow-up are often sufficient whilst in GERD more therapeutic options are usually needed with careful consideration of treatments that balance optimal symptom resolution with predictable side effects.
Non-pharmacological treatments are recommended in infants suspected of GER and include the following.
Head and body position after meals: So far there is no recommendation for prone, right lateral position in infants as it may increase the risk of sudden infant death syndrome[34]. One study has demonstrated the effectiveness of a supine 40 degree anti-Trendelenburg position using a “Multicare-AR Bed” in decreasing symptoms and acid reflux detected with MII-pH monitoring[75]. However, a retrospective study demonstrated more reflux episodes in the upright position compared to the supine position in children and infants, probably as a result of frequent TLESRs while they were awake[76]. Nocturnal reflux has, however, been associated with prolonged esophageal acid exposure due to decreasing esophageal clearance from gravity, which may support the rationale of upright head position after feeding in infants.
Diet: Extensively hydrolysed protein or amino acid formulas should be considered in infants suspected of GERD. Nonspecific signs and symptoms, however, provide a challenge for the diagnosis of cow’s milk protein allergy (CMPA). The Cow Milk Symptom Score (CoMiSS) might be used to evaluate infants before and after treatment of CMPA, but it is not considered as a diagnostic tool[77]. If there is no clinical improvement after a 4-8 wk trial of dietary cow’s milk protein exclusion, CMPA is unlikely. Recently CoMiSS was modified in which a score of more than 10 (previously more than 12) in infants supported a diagnosis of CMPA[78]. The stool pattern was also changed from the Bristol Stool Scale to the Brussels Infant and Toddlers Stool Scale as a more user-friendly tool for non-toilet trained children. The updated CoMiss score is shown in Table 3.
| Symptom | Characteristics and frequency | Score |
| Crying assessed by parents and without any obvious cause ≥ 1 wk, and not related to infection | ≤ 1 h/d | 0 |
| 1.0-1.5 h/d | 1 | |
| 1.5-2.0 h/d | 2 | |
| 2-3 h/d | 3 | |
| 3-4 h/d | 4 | |
| 4-5 h/d | 5 | |
| ≥ 5 h/d | 6 | |
| Regurgitation ≥ 1 wk | 0-2 episodes/d | 0 |
| 3-5 episodes (volume < 5 mL)/d | 1 | |
| > 5 episodes of volume > 5 mL | 2 | |
| > 5 episodes (volume < 50% of feeds)/d | 3 | |
| Small volume and happens > 30 min after each feed | 4 | |
| Regurgitation of ≥ 50% volume of a feed in ≥ 50% of total feeds | 5 | |
| Regurgitation of the complete feed after each feeding | 6 | |
| Stool: Brussels Infant and Toddlers Stool Scale (BITSS); no change ≥ 1 wk | Hard stools | 4 |
| Formed stools | 0 | |
| Loose stools not related to infection | 4 | |
| Watery stools not related to infection | 6 | |
| Skin symptoms not related to infection | Atopic eczema ≥ 1/wk | |
| Absent | 0 | |
| Mild | 1 | |
| Moderate | 2 | |
| Severe | 3 | |
| Acute urticaria/angioedema that directly related to cow’s milk | ||
| No | 0 | |
| Yes | 1 | |
| Respiratory symptoms not related to infection ≥ 1 wk | No respiratory symptoms | 0 |
| Slight symptoms | 1 | |
| Mild symptoms | 2 | |
| Severe symptoms | 3 |
Thickened formula use is associated with a significant decrease of visual regurgitation but not of acid reflux monitored by MII-pH[34]. Hence, thickening products have been recommended for use in infants with GER[1]. However, there has been rising concern about the safety of thickeners; for example inorganic arsenic in rice cereal[1], and the risk of necrotizing enterocolitis from xanthum gum and carob bean[79,80]. Moreover, rice cereal can be digested by amylase in breast milk limiting its use with breast milk.
If GERD symptoms in infants and children are not resolved with non-pharmacological treatment, medication can be considered. The most common medications include drugs that promote esophageal and gastric motility, tighten the LES, and acid suppressants to reduce esophageal mucosal injury (Table 4).
| Medication | Dose | Adverse effect | Approved age (FDA indicated) |
| PPI1 | |||
| Omeprazole | 1-4 mg/kg/d od | Diarrhea, abdominal pain, flatulence, headache, enteric infection, respiratory infection, rebound hypersecretion | > 1 yr old |
| Lansoprazole | 0.7-2 mg/kg/d od | 1Esomeprazole: Tarry stool, darkened urine | > 1 yr old |
| Esomeprazole | 3-5 kg: 2.5 mg od | 1Rabeprazole: Light-colored stool | > 1 mo old |
| > 5-7 kg: 5 mg od | |||
| > 7.5 kg, < 20 kg: 10 mg od | |||
| 20 kg: 20 mg od | |||
| Pantoprazole | 1-2 mg/kg/d od | > 5 yr old | |
| Rabeprazole | 0.5-1.0 mg/kg/d od | > 1 yr old | |
| Pro-motility | |||
| Metoclopramide | 0.4-0.9 mg/kg/d tid | Extrapyramidal side effect (1%), diarrhea, drowsiness | > 1 yr old |
| Domperidone | 0.8-0.9 mg/kg/d tid | Dry mouth, QT prolongation (rare) Abdominal pain, diarrhea, (rare) HPS in infants, QT prolongation (rare) | > 12 yr old |
| Erythromycin | 5 mg/kg/dose qid | Dizziness, diarrhea, dry mouth | All ages |
| Baclofen | 0.5 mg/kg/d tid | All ages | |
| Esophageal mucosal protection | |||
| Alginate antacid | Flatulence, diarrhea, nausea and vomiting | Younger than 12 yr of age is not generally recommended | |
| Magnesium alginate plus simethicone | Infant: 1-2 mL/kg/dose after feeding | ||
| Sodium alginate (225.00 mg sodium alginate, 87.25 mg magnesium alginate per sachet) | Child: 2.5-5.0 mL oral tid after meal | ||
| Sucralfate (sucrose, polyaluminium hydroxide) | 40-80 mg/kg/d qid | Constipation, aluminum toxicity in long-term use | In adult |
| Esoxx (sodium hyaluronate, sodium chondroitin sulfate, poloxamer 407, povidone K30, xylitol, potassium sorbate, sodium benzoate, red grape aroma, purified water) (10 mL/sachet) | 1-2 sachet/d after main meal and bedtime | No serious adverse effect because of the poor absorption, however, no data of long-term adverse effect | In Italy, it is approval for adolescents age > 12 yr old |
| Probiotics | |||
| Lactobacillus reuteri DSM 17938 | > 1 × 108 colony-forming units/d od | None | All ages |
Acid suppressant agents: Proton pump inhibitors (PPI)[81,82] and H2-receptor antagonists (H2RA)[83] are used as the gold standard of GERD treatment[1]. PPIs are more effective than H2RAs for acid suppression[84] and there is no tachyphylaxis with prolonged used. However, they may not be effective in non-acid or weakly acid reflux and their prolonged use can cause side effects especially increased rates of respiratory and gastrointestinal infection[85-88]. In addition, some H2RAs were withdrawn from the market because of the increased risk of malignancy from nitrosamine contamination[89]. It should also be noted that acid suppression has potential effects on the integrity of gut microbiota[90] with worsening of GI symptoms, although the concomitant use of probiotics have been suggested to mitigate this issue[91-93].
Prokinetic agents: The effectiveness of prokinetic agents was evidenced in adult populations but much less so in children. Common prokinetics used in infants and children include domperidone[94], metoclopramide[95] and erythromycin. Domperidone and metoclopramide act as 5HT4 agonists in the stomach and gut while erythromycin stimulates motilin receptors in the antral area of stomach[96]. These medications are therefore believed to be useful in children and infants who have GERD secondary to gastroparesis and to speed up upper GI transit time. Limitations for the use of domperidone and metoclopramide include significant potential side effects of QT prolongation[97] and extrapyramidal symptoms[98], respectively. When administered for a prolonged period, erythromycin can potentially cause tachyphylaxis[99]. There is little available information on other prokinetic drugs such as mosapride, itopride, prucalopride and renzapride in children. Another prokinetic agent with direct effects on the LES is baclofen. Baclofen is a gamma-aminobutyric acid (GABA)-B receptor agonist and appear to act by reducing TLESRs. Baclofen has also been shown to accelerate gastric emptying[100-103]. However, the adverse effects of dyspepsia, drowsiness and dizziness[104] can limit its use in infants and children.
Alginate antacids: Since the late 1990s, compound alginate preparations were changed to become aluminum-free and safe for infants. A Cochrane review in 2014 indicated moderate evidence of this agent for the improvement of GER in infants in short term follow-up[105-108]. Alginate antacids act by creating a barrier and appear effective for rapid symptom resolution regardless of the stimulus (acid, pepsin, bile, or mixed)[109]. Evidence for their use in GERD is limited[110].
Esophageal mucosal protectants: Sucralfate is a well-known mucosal protective drug that is composed of sucrose sulfate and aluminum hydroxide. It acts by inhibiting peptic digestion, providing mucosal protection and stimulating tissue growth and healing[111]. Recently, the novel medical device, EsoxxTM, was developed and mainly composed of two mucopolysaccharides, mixed to a mucoadhesive gelling agent and a viscosity regulator compound to form a mucoadhesive formulation. It adheres to the esophageal mucosa and act as barrier against refluxed gastric content[112-115]. However, EsoxxTM was originally developed for use in adults[114,116], and there is a rising concern about applying it in children[117]. A recent publication has demonstrated the efficacy and safety of EsoxxTM in adolescents[118] but the data in younger children is scarce.
Probiotics: Because of the safety profiles of probiotics, this agent has been used worldwide in infants and children for many purposes such as acute diarrhea, colic, and regurgitation. A large RCT study in 589 term infants demonstrated significant efficacy of Lactobacillus reuteri DSM 17938 in preventing colic. In the same RCT, the author also demonstrated the efficacy of this probiotic in decreasing the mean number of regurgitations per day[119]. Hence, probiotics are prescribed widely in clinical practice to prevent or treat GER. However, in GERD, there has been no strong evidence for their use and further research is warranted.
These are reserved for a minority of children suffering severe GERD non responsive to medical treatments.
Transpyloric feeding is often considered in GERD that might subside with time for example; in severe gastroparesis from medications such as opioids, preterm infants[72,73] or from critical illness such as children in intensive care units[120]. There is, however, increasing data supporting its use as a viable alternative therapeutic strategy to surgery (fundoplication) even for high-risk patients, such as those with neurological impairment, given their similar overall efficacy and rates of complications[121,122]. For transpyloric feeding recurrent tube dislodgement provides one of most common complications.
In the highest risk patients especially those with severe neurodisability and life-threatening complications of GERD, open surgical or laparoscopic fundoplication has traditionally been considered the therapy of choice[123-126].
They are, however, associated with a significant need for redo-fundoplication and concurrent medication use in the most difficult to treat patients[34]. In addition, transoral incisionless fundoplication (TIF) procedures have been increasingly performed in patients with severe GERD[127-130]. Even though the recurrence rate in long term follow-up in children with severe neurological impairment was high[131], the complications from TIF were minimal[132]. As a result, some selective cases with GERD might benefit from this low-risk procedure.
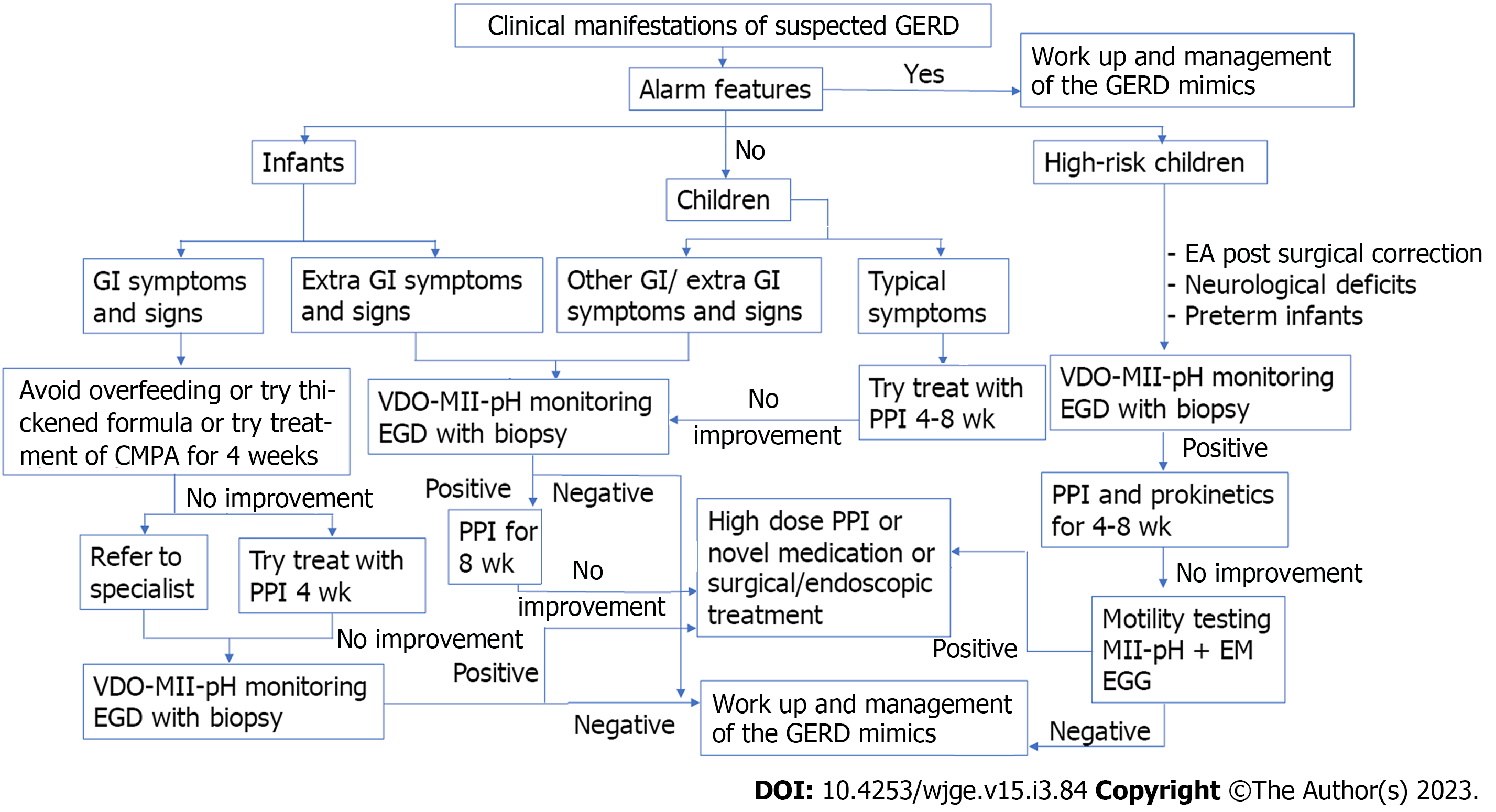
The recognition, diagnosis and treatment of GERD, especially in young children remains challenging. It requires to be differentiated from GER as well as GERD mimics, which is best approached using careful clinical assessment, especially in high-risk groups, paying attention to alarm features and the selective use of investigations, where necessary. There remains, however a lack of a gold standard tool for the diagnosis of GERD. Management should aim to target underlying aetiopathology and minimize complications. These may be managed through a variety of non-pharmacological and pharmacological strategies with surgery limited to very selected indications. Further studies to optimize the diagnosis and management of GERD are still needed. Table 5 summarize the updated diagnostic investigations and treatments for children with suspected GERD and Figure 7 proposes the steps of diagnosis and management in children with suspected GERD.
| Novel diagnosis tools | Treatment |
| Combined Video-MII-pH monitoring test to increase the detection of symptom associated reflux | Non-pharmacological treatment |
| Supine 40-degree anti-Trendelenburg position | |
| Using the updated Cow Milk Symptom Score (CoMiSS) before and after therapeutic trial for CMPA | |
| Esophageal manometry with pH-MII monitoring | Pharmacological treatment |
| Novel prokinetics ex. mosapride, itopride, prucalopride and renzapride | |
| Electrogastrography | Alginate antacid |
| Esophageal mucosal protection: sucralfate, EsoxxTM | |
| Probiotics | |
| Therapeutic trial with transpyloric feeding | Endoscopic treatment |
| Transoral incisionless fundoplication |
The authors are very grateful to Miss Alisara Pittiyayon at the Electricity Generating Authority of Thailand for preparing Figure 1, and Assistant Professor Anapat Sanpavat at division of Pathology, Chulalongkorn University for providing Figure 4C and F. And Settachote Maholarnkij at Department of Pediatrics, Chulalongkorn University for providing Figure 6.
| 1. | Rosen R, Vandenplas Y, Singendonk M, Cabana M, DiLorenzo C, Gottrand F, Gupta S, Langendam M, Staiano A, Thapar N, Tipnis N, Tabbers M. Pediatric Gastroesophageal Reflux Clinical Practice Guidelines: Joint Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2018;66:516-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 610] [Cited by in RCA: 578] [Article Influence: 72.3] [Reference Citation Analysis (1)] |
| 2. | Singendonk M, Goudswaard E, Langendam M, van Wijk M, van Etten-Jamaludin F, Benninga M, Tabbers M. Prevalence of Gastroesophageal Reflux Disease Symptoms in Infants and Children: A Systematic Review. J Pediatr Gastroenterol Nutr. 2019;68:811-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 3. | Van Howe RS, Storms MR. Gastroesophageal reflux symptoms in infants in a rural population: longitudinal data over the first six months. BMC Pediatr. 2010;10:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | McLoughlin VZY, Suaini NHA, Siah K, Loo EXL, Pang WW, Chong YS, Godfrey KM, Tan KH, Chan JKY, Goh AEN, Lee BW, Shek LP, Eriksson JG, Aw MM, Tham EH. Prevalence, risk factors and parental perceptions of gastroesophageal reflux disease in Asian infants in Singapore. Ann Acad Med Singap. 2022;51:263-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Chen PL, Soto-Ramírez N, Zhang H, Karmaus W. Association Between Infant Feeding Modes and Gastroesophageal Reflux: A Repeated Measurement Analysis of the Infant Feeding Practices Study II. J Hum Lact. 2017;33:267-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Maholarnkij S, Sanpavat A, Decharun K, Dumrisilp T, Tubjareon C, Kanghom B, Patcharatrakul T, Chaijitraruch N, Chongsrisawat V, Sintusek P. Detection of reflux-symptom association in children with esophageal atresia by video-pH-impedance study. World J Gastroenterol. 2020;26:4159-4169. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 7. | Lauriti G, Lisi G, Lelli Chiesa P, Zani A, Pierro A. Gastroesophageal reflux in children with neurological impairment: a systematic review and meta-analysis. Pediatr Surg Int. 2018;34:1139-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 8. | Kawahara H, Tazuke Y, Soh H, Usui N, Okuyama H. Characteristics of gastroesophageal reflux in pediatric patients with neurological impairment. Pediatr Surg Int. 2017;33:1073-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Hrabovsky EE, Mullett MD. Gastroesophageal reflux and the premature infant. J Pediatr Surg. 1986;21:583-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 33] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Golski CA, Rome ES, Martin RJ, Frank SH, Worley S, Sun Z, Hibbs AM. Pediatric specialists' beliefs about gastroesophageal reflux disease in premature infants. Pediatrics. 2010;125:96-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Omari TI, Barnett C, Snel A, Goldsworthy W, Haslam R, Davidson G, Kirubakaran C, Bakewell M, Fraser R, Dent J. Mechanisms of gastroesophageal reflux in healthy premature infants. J Pediatr. 1998;133:650-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 80] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Iacono G, Carroccio A, Cavataio F, Montalto G, Kazmierska I, Lorello D, Soresi M, Notarbartolo A. Gastroesophageal reflux and cow's milk allergy in infants: a prospective study. J Allergy Clin Immunol. 1996;97:822-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 127] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 13. | Farahmand F, Najafi M, Ataee P, Modarresi V, Shahraki T, Rezaei N. Cow's Milk Allergy among Children with Gastroesophageal Reflux Disease. Gut Liver. 2011;5:298-301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Garzi A, Messina M, Frati F, Carfagna L, Zagordo L, Belcastro M, Parmiani S, Sensi L, Marcucci F. An extensively hydrolysed cow's milk formula improves clinical symptoms of gastroesophageal reflux and reduces the gastric emptying time in infants. Allergol Immunopathol (Madr). 2002;30:36-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Borrelli O, Mancini V, Thapar N, Giorgio V, Elawad M, Hill S, Shah N, Lindley KJ. Cow's milk challenge increases weakly acidic reflux in children with cow's milk allergy and gastroesophageal reflux disease. J Pediatr. 2012;161:476-481.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Vandenplas Y, Hassall E. Mechanisms of gastroesophageal reflux and gastroesophageal reflux disease. J Pediatr Gastroenterol Nutr. 2002;35:119-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 77] [Article Influence: 3.2] [Reference Citation Analysis (1)] |
| 17. | Jadcherla SR, Parks VN, Peng J, Dzodzomenyo S, Fernandez S, Shaker R, Splaingard M. Esophageal sensation in premature human neonates: temporal relationships and implications of aerodigestive reflexes and electrocortical arousals. Am J Physiol Gastrointest Liver Physiol. 2012;302:G134-G144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Omari TI, Miki K, Davidson G, Fraser R, Haslam R, Goldsworthy W, Bakewell M, Dent J. Characterisation of relaxation of the lower oesophageal sphincter in healthy premature infants. Gut. 1997;40:370-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 69] [Article Influence: 2.4] [Reference Citation Analysis (2)] |
| 19. | Pena EM, Parks VN, Peng J, Fernandez SA, Di Lorenzo C, Shaker R, Jadcherla SR. Lower esophageal sphincter relaxation reflex kinetics: effects of peristaltic reflexes and maturation in human premature neonates. Am J Physiol Gastrointest Liver Physiol. 2010;299:G1386-G1395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 20. | Salvia G, De Vizia B, Manguso F, Iula VD, Terrin G, Spadaro R, Russo G, Cucchiara S. Effect of intragastric volume and osmolality on mechanisms of gastroesophageal reflux in children with gastroesophageal reflux disease. Am J Gastroenterol. 2001;96:1725-1732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 39] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 21. | Mittal RK, McCallum RW. Characteristics and frequency of transient relaxations of the lower esophageal sphincter in patients with reflux esophagitis. Gastroenterology. 1988;95:593-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 176] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 22. | Sifrim D, Holloway R, Silny J, Xin Z, Tack J, Lerut A, Janssens J. Acid, nonacid, and gas reflux in patients with gastroesophageal reflux disease during ambulatory 24-hour pH-impedance recordings. Gastroenterology. 2001;120:1588-1598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 274] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 23. | Fiorino KN, Nurko S. Developmental Anatomy and Physiology of the Esophagus. Pedia Gastrointest and Liver Dis. 2021;194-201.e192. |
| 24. | Jadcherla SR, Hogan WJ, Shaker R. Physiology and pathophysiology of glottic reflexes and pulmonary aspiration: from neonates to adults. Semin Respir Crit Care Med. 2010;31:554-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 25. | Jadcherla SR, Hoffmann RG, Shaker R. Effect of maturation of the magnitude of mechanosensitive and chemosensitive reflexes in the premature human esophagus. J Pediatr. 2006;149:77-82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 68] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 26. | Crookes PF, Corkill S, DeMeester TR. Gastroesophageal reflux in achalasia. When is reflux really reflux? Dig Dis Sci. 1997;42:1354-1361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 81] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Shoenut JP, Duerksen D, Yaffe CS. A prospective assessment of gastroesophageal reflux before and after treatment of achalasia patients: pneumatic dilation versus transthoracic limited myotomy. Am J Gastroenterol. 1997;92:1109-1112. [PubMed] |
| 28. | Mittal R, Vaezi MF. Esophageal Motility Disorders and Gastroesophageal Reflux Disease. N Engl J Med. 2020;383:1961-1972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 72] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 29. | Kountouras J, Zavos C, Chatzopoulos D, Katsinelos P. Helicobacter pylori and gastro-oesophageal reflux disease. Lancet. 2006;368:986; author reply 986-986; author reply 987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 30. | Kuiken S, Van Den Elzen B, Tytgat G, Bennink R, Boeckxstaens G. Evidence for pooling of gastric secretions in the proximal stomach in humans using single photon computed tomography. Gastroenterology. 2002;123:2157-8; author reply 2158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 31. | Fletcher J, Wirz A, Young J, Vallance R, McColl KE. Unbuffered highly acidic gastric juice exists at the gastroesophageal junction after a meal. Gastroenterology. 2001;121:775-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 227] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 32. | Hila A, Bouali H, Xue S, Knuff D, Castell DO. Postprandial stomach contents have multiple acid layers. J Clin Gastroenterol. 2006;40:612-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 33. | Simonian HP, Vo L, Doma S, Fisher RS, Parkman HP. Regional postprandial differences in pH within the stomach and gastroesophageal junction. Dig Dis Sci. 2005;50:2276-2285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 103] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 34. | Vandenplas Y. Gastroesophageal Reflux. Pediat Gastrointest and Liver Dis. 2021;212-229.e216. |
| 35. | Blake K, Teague WG. Gastroesophageal reflux disease and childhood asthma. Curr Opin Pulm Med. 2013;19:24-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 36. | Lenderking WR, Hillson E, Crawley JA, Moore D, Berzon R, Pashos CL. The clinical characteristics and impact of laryngopharyngeal reflux disease on health-related quality of life. Value Health. 2003;6:560-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 37. | Becker V, Drabner R, Graf S, Schlag C, Nennstiel S, Buchberger AM, Schmid RM, Saur D, Bajbouj M. New aspects in the pathomechanism and diagnosis of the laryngopharyngeal reflux-clinical impact of laryngeal proton pumps and pharyngeal pH metry in extraesophageal gastroesophageal reflux disease. World J Gastroenterol. 2015;21:982-987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 38. | Kilic M, Ozturk F, Kirmemis O, Atmaca S, Guner SN, Caltepe G, Sancak R, Kalayci AG. Impact of laryngopharyngeal and gastroesophageal reflux on asthma control in children. Int J Pediatr Otorhinolaryngol. 2013;77:341-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 39. | van der Pol RJ, Smits MJ, van Wijk MP, Omari TI, Tabbers MM, Benninga MA. Efficacy of proton-pump inhibitors in children with gastroesophageal reflux disease: a systematic review. Pediatrics. 2011;127:925-935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 145] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 40. | Westra SJ, Derkx HH, Taminiau JA. Symptomatic gastroesophageal reflux: diagnosis with ultrasound. J Pediatr Gastroenterol Nutr. 1994;19:58-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 41. | Riccabona M, Maurer U, Lackner H, Uray E, Ring E. The role of sonography in the evaluation of gastro-oesophageal reflux--correlation to pH-metry. Eur J Pediatr. 1992;151:655-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 42. | Farina R, Pennisi F, La Rosa M, Puglisi C, Mazzone G, Riva G, Foti PV, Ettorre GC. Contrast-enhanced colour-Doppler sonography versus pH-metry in the diagnosis of gastro-oesophageal reflux in children. Radiol Med. 2008;113:591-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 43. | Matrunola M, Grandin A, Mazza ML, Panetta A, Giardini V, Corrado G. Role of radiography and ultrasonography in the diagnosis of the pediatric gastro-esophageal reflux disease. Eur Rev Med Pharmacol Sci. 2003;7:147-149. [PubMed] |
| 44. | Charoenwat B, Sintusek P, Chaijitraruch N, Mahayosnond A, Suksri S, Patcharatrakul T, Chongsrisawat V. Transcutaneous esophageal ultrasonography in children with suspected gastroesophageal reflux disease. J Med Asso Thai. 2018;101:S1-S745. |
| 45. | Minella R, Minelli R, Rossi E, Cremone G, Tozzi A. Gastroesophageal and gastric ultrasound in children: the state of the art. J Ultrasound. 2021;24:11-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 46. | Aksglaede K, Pedersen JB, Lange A, Funch-Jensen P, Thommesen P. Gastro-esophageal reflux demonstrated by radiography in infants less than 1 year of age. Comparison with pH monitoring. Acta Radiol. 2003;44:136-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 47. | Rosen R, Amirault J, Johnston N, Haver K, Khatwa U, Rubinstein E, Nurko S. The utility of endoscopy and multichannel intraluminal impedance testing in children with cough and wheezing. Pediatr Pulmonol. 2014;49:1090-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 48. | Rao NM, Campbell DI, Rao P. Two years' experience of using the Bravo wireless oesophageal pH monitoring system at a single UK tertiary centre. Acta Paediatr. 2017;106:312-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 49. | Croffie JM, Fitzgerald JF, Molleston JP, Gupta SK, Corkins MR, Pfefferkorn MD, Lim JR, Steiner SJ, Dadzie SK. Accuracy and tolerability of the Bravo catheter-free pH capsule in patients between the ages of 4 and 18 years. J Pediatr Gastroenterol Nutr. 2007;45:559-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 50. | Chiou E, Rosen R, Jiang H, Nurko S. Diagnosis of supra-esophageal gastric reflux: correlation of oropharyngeal pH with esophageal impedance monitoring for gastro-esophageal reflux. Neurogastroenterol Motil. 2011;23:717-e326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 51. | Ummarino D, Vandermeulen L, Roosens B, Urbain D, Hauser B, Vandenplas Y. Gastroesophageal reflux evaluation in patients affected by chronic cough: Restech versus multichannel intraluminal impedance/pH metry. Laryngoscope. 2013;123:980-984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 52. | Plocek A, Gębora-Kowalska B, Białek J, Fendler W, Toporowska-Kowalska E. Esophageal Impedance-pH Monitoring and Pharyngeal pH Monitoring in the Diagnosis of Extraesophageal Reflux in Children. Gastroenterol Res Pract. 2019;2019:6271910. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 53. | Joniau S, Bradshaw A, Esterman A, Carney AS. Reflux and laryngitis: a systematic review. Otolaryngol Head Neck Surg. 2007;136:686-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 49] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 54. | Yadlapati R, Adkins C, Jaiyeola DM, Lidder AK, Gawron AJ, Tan BK, Shabeeb N, Price CP, Agrawal N, Ellenbogen M, Smith SS, Bove M, Pandolfino JE. Abilities of Oropharyngeal pH Tests and Salivary Pepsin Analysis to Discriminate Between Asymptomatic Volunteers and Subjects With Symptoms of Laryngeal Irritation. Clin Gastroenterol Hepatol. 2016;14:535-542.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (1)] |
| 55. | Ramaiah RN, Stevenson M, McCallion WA. Hypopharyngeal and distal esophageal pH monitoring in children with gastroesophageal reflux and respiratory symptoms. J Pediatr Surg. 2005;40:1557-1561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 56. | Ayazi S, Lipham JC, Hagen JA, Tang AL, Zehetner J, Leers JM, Oezcelik A, Abate E, Banki F, DeMeester SR, DeMeester TR. A new technique for measurement of pharyngeal pH: normal values and discriminating pH threshold. J Gastrointest Surg. 2009;13:1422-1429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 118] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 57. | Shin MS. Esophageal pH and Combined Impedance-pH Monitoring in Children. Pediatr Gastroenterol Hepatol Nutr. 2014;17:13-22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 58. | Wenzl TG, Benninga MA, Loots CM, Salvatore S, Vandenplas Y; ESPGHAN EURO-PIG Working Group. Indications, methodology, and interpretation of combined esophageal impedance-pH monitoring in children: ESPGHAN EURO-PIG standard protocol. J Pediatr Gastroenterol Nutr. 2012;55:230-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 118] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 59. | Riezzo G, Russo F, Indrio F. Electrogastrography in adults and children: the strength, pitfalls, and clinical significance of the cutaneous recording of the gastric electrical activity. Biomed Res Int. 2013;2013:282757. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 60. | van Lennep M, Leijdekkers ML, Oors JM, Benninga MA, van Wijk MP, Singendonk MMJ. Clinical Experience With Performing Esophageal Function Testing in Children. J Pediatr Gastroenterol Nutr. 2021;72:226-231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 61. | Rosen R, Amirault J, Giligan E, Khatwa U, Nurko S. Intraesophageal pressure recording improves the detection of cough during multichannel intraluminal impedance testing in children. J Pediatr Gastroenterol Nutr. 2014;58:22-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 62. | Carson DA, Bhat S, Hayes TCL, Gharibans AA, Andrews CN, O'Grady G, Varghese C. Abnormalities on Electrogastrography in Nausea and Vomiting Syndromes: A Systematic Review, Meta-Analysis, and Comparison to Other Gastric Disorders. Dig Dis Sci. 2022;67:773-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 63. | Bhat S, Varghese C, Carson DA, Hayes TCL, Gharibans AA, Andrews CN, O'Grady G. Gastric dysrhythmia in gastroesophageal reflux disease: a systematic review and meta-analysis. Esophagus. 2021;18:425-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 64. | Bhat S, Varghese C, Carson DA, Hayes TCL, Andrews CN, Mousa H, O'Grady G, Gharibans AA. Electrogastrography Abnormalities in Pediatric Gastroduodenal Disorders: A Systematic Review and Meta-analysis. J Pediatr Gastroenterol Nutr. 2021;73:9-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 65. | Dy F, Amirault J, Mitchell PD, Rosen R. Salivary Pepsin Lacks Sensitivity as a Diagnostic Tool to Evaluate Extraesophageal Reflux Disease. J Pediatr. 2016;177:53-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 66. | Fortunato JE, D'Agostino RB Jr, Lively MO. Pepsin in saliva as a biomarker for oropharyngeal reflux compared with 24-hour esophageal impedance/pH monitoring in pediatric patients. Neurogastroenterol Motil. 2017;29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 67. | Rosen R, Johnston N, Hart K, Khatwa U, Nurko S. The presence of pepsin in the lung and its relationship to pathologic gastro-esophageal reflux. Neurogastroenterol Motil. 2012;24:129-133, e84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 68. | Farrell S, McMaster C, Gibson D, Shields MD, McCallion WA. Pepsin in bronchoalveolar lavage fluid: a specific and sensitive method of diagnosing gastro-oesophageal reflux-related pulmonary aspiration. J Pediatr Surg. 2006;41:289-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 93] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 69. | Rosen R, Fritz J, Nurko A, Simon D, Nurko S. Lipid-laden macrophage index is not an indicator of gastroesophageal reflux-related respiratory disease in children. Pediatrics. 2008;121:e879-e884. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 70. | Barrett MW, Myers JC, Watson DI, Jamieson GG. Detection of bile reflux: in vivo validation of the Bilitec fibreoptic system. Dis Esophagus. 2000;13:44-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 71. | Orel R, Brecelj J, Homan M, Heuschkel R. Treatment of oesophageal bile reflux in children: the results of a prospective study with omeprazole. J Pediatr Gastroenterol Nutr. 2006;42:376-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 72. | Malcolm WF, Smith PB, Mears S, Goldberg RN, Cotten CM. Transpyloric tube feeding in very low birthweight infants with suspected gastroesophageal reflux: impact on apnea and bradycardia. J Perinatol. 2009;29:372-375. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 73. | Misra S, Macwan K, Albert V. Transpyloric feeding in gastroesophageal-reflux-associated apnea in premature infants. Acta Paediatr. 2007;96:1426-1429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 74. | Rosen R, Hart K, Warlaumont M. Incidence of gastroesophageal reflux during transpyloric feeds. J Pediatr Gastroenterol Nutr. 2011;52:532-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 75. | Vandenplas Y, De Schepper J, Verheyden S, Devreker T, Franckx J, Peelman M, Denayer E, Hauser B. A preliminary report on the efficacy of the Multicare AR-Bed in 3-week-3-month-old infants on regurgitation, associated symptoms and acid reflux. Arch Dis Child. 2010;95:26-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 76. | Quitadamo P, Tambucci R, Alessandrella A, Andreozzi M, Malamisura M, Isoldi S, Caldaro T, Zenzeri L, Verrotti A, De Angelis P, Siani P, Staiano A. Association between body positioning and gastroesophageal reflux in paediatric age. Acta Paediatr. 2020;109:1033-1039. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 77. | Vandenplas Y, Dupont C, Eigenmann P, Host A, Kuitunen M, Ribes-Koninckx C, Shah N, Shamir R, Staiano A, Szajewska H, Von Berg A. A workshop report on the development of the Cow's Milk-related Symptom Score awareness tool for young children. Acta Paediatr. 2015;104:334-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 78. | Vandenplas Y, Bajerova K, Dupont C, Eigenmann P, Kuitunen M, Meyer R, Ribes-Koninckx C, Salvatore S, Shamir R, Szajewska H. The Cow's Milk Related Symptom Score: The 2022 Update. Nutrients. 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 79. | Beal J, Silverman B, Bellant J, Young TE, Klontz K. Late onset necrotizing enterocolitis in infants following use of a xanthan gum-containing thickening agent. J Pediatr. 2012;161:354-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 80. | Woods CW, Oliver T, Lewis K, Yang Q. Development of necrotizing enterocolitis in premature infants receiving thickened feeds using SimplyThick®. J Perinatol. 2012;32:150-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 81. | Gold BD, Gunasekaran T, Tolia V, Wetzler G, Conter H, Traxler B, Illueca M. Safety and symptom improvement with esomeprazole in adolescents with gastroesophageal reflux disease. J Pediatr Gastroenterol Nutr. 2007;45:520-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 82. | Shakhnovich V, Brian Smith P, Guptill JT, James LP, Collier DN, Wu H, Livingston CE, Zhao J, Kearns GL, Cohen-Wolkowiez M; Best Pharmaceuticals for Children Act–Pediatric Trials Network. A Population-Based Pharmacokinetic Model Approach to Pantoprazole Dosing for Obese Children and Adolescents. Paediatr Drugs. 2018;20:483-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 83. | van der Pol R, Langendam M, Benninga M, van Wijk M, Tabbers M. Efficacy and safety of histamine-2 receptor antagonists. JAMA Pediatr. 2014;168:947-954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 84. | Lin PC, Chang CH, Hsu PI, Tseng PL, Huang YB. The efficacy and safety of proton pump inhibitors vs histamine-2 receptor antagonists for stress ulcer bleeding prophylaxis among critical care patients: a meta-analysis. Crit Care Med. 2010;38:1197-1205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 109] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 85. | Giuliano C, Wilhelm SM, Kale-Pradhan PB. Are proton pump inhibitors associated with the development of community-acquired pneumonia? Expert Rev Clin Pharmacol. 2012;5:337-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 85] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 86. | Nguyen PA, Islam M, Galvin CJ, Chang CC, An SY, Yang HC, Huang CW, Li YJ, Iqbal U. Meta-analysis of proton pump inhibitors induced risk of community-acquired pneumonia. Int J Qual Health Care. 2020;32:292-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 87. | Chen Y, Liu B, Glass K, Du W, Banks E, Kirk M. Use of Proton Pump Inhibitors and the Risk of Hospitalization for Infectious Gastroenteritis. PLoS One. 2016;11:e0168618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 88. | Wang YH, Wintzell V, Ludvigsson JF, Svanström H, Pasternak B. Association Between Proton Pump Inhibitor Use and Risk of Asthma in Children. JAMA Pediatr. 2021;175:394-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 89. | Perisetti A, Goyal H, Tharian B. The 'burn' of ranitidine recall: current insights and mitigation strategies. Eur J Gastroenterol Hepatol. 2021;33:e1013-e1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 90. | Shi YC, Cai ST, Tian YP, Zhao HJ, Zhang YB, Chen J, Ren RR, Luo X, Peng LH, Sun G, Yang YS. Effects of Proton Pump Inhibitors on the Gastrointestinal Microbiota in Gastroesophageal Reflux Disease. Genomics Proteomics Bioinformatics. 2019;17:52-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 91. | Belei O, Olariu L, Dobrescu A, Marcovici T, Marginean O. Is It Useful to Administer Probiotics Together With Proton Pump Inhibitors in Children With Gastroesophageal Reflux? J Neurogastroenterol Motil. 2018;24:51-57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 92. | Hegar B, Hutapea EI, Advani N, Vandenplas Y. A double-blind placebo-controlled randomized trial on probiotics in small bowel bacterial overgrowth in children treated with omeprazole. J Pediatr (Rio J). 2013;89:381-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 93. | Liang S, Xu L, Zhang D, Wu Z. Effect of probiotics on small intestinal bacterial overgrowth in patients with gastric and colorectal cancer. Turk J Gastroenterol. 2016;27:227-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 94. | Pritchard DS, Baber N, Stephenson T. Should domperidone be used for the treatment of gastro-oesophageal reflux in children? Br J Clin Pharmacol. 2005;59:725-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 56] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 95. | Craig WR, Hanlon-Dearman A, Sinclair C, Taback S, Moffatt M. Metoclopramide, thickened feedings, and positioning for gastro-oesophageal reflux in children under two years. Cochrane Database Syst Rev. 2004;CD003502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 35] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 96. | Tack J. Prokinetics and fundic relaxants in upper functional GI disorders. Curr Opin Pharmacol. 2008;8:690-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 96] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 97. | Ngoenmak T, Treepongkaruna S, Buddharaksa Y, Khositseth A. Effects of Domperidone on QT Interval in Children with Gastroesophageal Reflux Disease. Pediatr Neonatol. 2016;57:60-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 98. | Lau Moon Lin M, Robinson PD, Flank J, Sung L, Dupuis LL. The Safety of Metoclopramide in Children: A Systematic Review and Meta-Analysis. Drug Saf. 2016;39:675-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 99. | Peeters TL. Erythromycin and other macrolides as prokinetic agents. Gastroenterology. 1993;105:1886-1899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 162] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 100. | Omari TI, Benninga MA, Sansom L, Butler RN, Dent J, Davidson GP. Effect of baclofen on esophagogastric motility and gastroesophageal reflux in children with gastroesophageal reflux disease: a randomized controlled trial. J Pediatr. 2006;149:468-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 91] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 101. | Kawai M, Kawahara H, Hirayama S, Yoshimura N, Ida S. Effect of baclofen on emesis and 24-hour esophageal pH in neurologically impaired children with gastroesophageal reflux disease. J Pediatr Gastroenterol Nutr. 2004;38:317-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 35] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 102. | Wiersma HE, van Boxtel CJ, Butter JJ, van Aalderen WM, Omari T, Benninga MA. Pharmacokinetics of a single oral dose of baclofen in pediatric patients with gastroesophageal reflux disease. Ther Drug Monit. 2003;25:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 103. | Vadlamudi NB, Hitch MC, Dimmitt RA, Thame KA. Baclofen for the treatment of pediatric GERD. J Pediatr Gastroenterol Nutr. 2013;57:808-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 104. | Bell RC, Barnes WE, Carter BJ, Sewell RW, Mavrelis PG, Ihde GM, Hoddinott KM, Fox MA, Freeman KD, Gunsberger T, Hausmann MG, Dargis D, DaCosta Gill B, Wilson E, Trad KS. Transoral incisionless fundoplication: 2-year results from the prospective multicenter U.S. study. Am Surg. 2014;80:1093-1105. [PubMed] |
| 105. | Mahant S. Pharmacological treatment of children with gastro-oesophageal reflux. Paediatr Child Health. 2017;22:30-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 106. | Buts JP, Barudi C, Otte JB. Double-blind controlled study on the efficacy of sodium alginate (Gaviscon) in reducing gastroesophageal reflux assessed by 24 h continuous pH monitoring in infants and children. Eur J Pediatr. 1987;146:156-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 52] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 107. | Argüelles-Martín F, González-Fernández F, Gentles MG, Navarro-Merino M. Sucralfate in the treatment of reflux esophagitis in children. Preliminary results. Scand J Gastroenterol Suppl. 1989;156:43-47. [PubMed] |
| 108. | Tytgat GN. Clinical efficacy of sucralfate in reflux oesophagitis. Scand J Gastroenterol Suppl. 1987;140:29-31. [PubMed] |
| 109. | Salvatore S, Ripepi A, Huysentruyt K, van de Maele K, Nosetti L, Agosti M, Salvatoni A, Vandenplas Y. The Effect of Alginate in Gastroesophageal Reflux in Infants. Paediatr Drugs. 2018;20:575-583. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 110. | Bor S, Kalkan İH, Çelebi A, Dinçer D, Akyüz F, Dettmar P, Özen H. Alginates: From the ocean to gastroesophageal reflux disease treatment. Turk J Gastroenterol. 2019;30:109-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 111. | Scarpignato C, Hongo M, Wu JCY, Lottrup C, Lazarescu A, Stein E, Hunt RH. Pharmacologic treatment of GERD: Where we are now, and where are we going? Ann N Y Acad Sci. 2020;1482:193-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 112. | Gaffney J, Matou-Nasri S, Grau-Olivares M, Slevin M. Therapeutic applications of hyaluronan. Mol Biosyst. 2010;6:437-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 79] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 113. | Volpi N, Schiller J, Stern R, Soltés L. Role, metabolism, chemical modifications and applications of hyaluronan. Curr Med Chem. 2009;16:1718-1745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 174] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 114. | Savarino V, Pace F, Scarpignato C; Esoxx Study Group. Randomised clinical trial: mucosal protection combined with acid suppression in the treatment of non-erosive reflux disease - efficacy of Esoxx, a hyaluronic acid-chondroitin sulphate based bioadhesive formulation. Aliment Pharmacol Ther. 2017;45:631-642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 66] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 115. | Di Simone MP, Baldi F, Vasina V, Scorrano F, Bacci ML, Ferrieri A, Poggioli G. Barrier effect of Esoxx(®) on esophageal mucosal damage: experimental study on ex-vivo swine model. Clin Exp Gastroenterol. 2012;5:103-107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 116. | Palmieri B, Merighi A, Corbascio D, Rottigni V, Fistetto G, Esposito A. Fixed combination of hyaluronic acid and chondroitin-sulphate oral formulation in a randomized double blind, placebo controlled study for the treatment of symptoms in patients with non-erosive gastroesophageal reflux. Eur Rev Med Pharmacol Sci. 2013;17:3272-3278. [PubMed] |
| 117. | Huijghebaert S, De Bruyne P, Allegaert K, Vande Velde S, De Bruyne R, Van Biervliet S, Van Winckel M. Medical devices that look like medicines: safety and regulatory concerns for children in Europe. Arch Dis Child. 2020;105:147-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 118. | Romano C, Scarpignato C. Pharmacologic treatment of GERD in adolescents: Is esophageal mucosal protection an option? Therap Adv Gastroenterol. 2022;15:17562848221115319. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 119. | Indrio F, Di Mauro A, Riezzo G, Civardi E, Intini C, Corvaglia L, Ballardini E, Bisceglia M, Cinquetti M, Brazzoduro E, Del Vecchio A, Tafuri S, Francavilla R. Prophylactic use of a probiotic in the prevention of colic, regurgitation, and functional constipation: a randomized clinical trial. JAMA Pediatr. 2014;168:228-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 141] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 120. | Panadero E, López-Herce J, Caro L, Sanchez A, Cueto E, Bustinza A, Moral R, Carrillo A, Sancho L. Transpyloric enteral feeding in critically ill children. J Pediatr Gastroenterol Nutr. 1998;26:43-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 121. | Stone B, Hester G, Jackson D, Richardson T, Hall M, Gouripeddi R, Butcher R, Keren R, Srivastava R. Effectiveness of Fundoplication or Gastrojejunal Feeding in Children With Neurologic Impairment. Hosp Pediatr. 2017;7:140-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 122. | Srivastava R, Downey EC, O'Gorman M, Feola P, Samore M, Holubkov R, Mundorff M, James BC, Rosenbaum P, Young PC, Dean JM. Impact of fundoplication versus gastrojejunal feeding tubes on mortality and in preventing aspiration pneumonia in young children with neurologic impairment who have gastroesophageal reflux disease. Pediatrics. 2009;123:338-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 72] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 123. | Jackson HT, Kane TD. Surgical management of pediatric gastroesophageal reflux disease. Gastroenterol Res Pract. 2013;2013:863527. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 124. | Ceriati E, Marchetti P, Caccamo R, Adorisio O, Rivosecchi F, De Peppo F. Nissen fundoplication and combined procedures to reduce recurrence of gastroesophageal reflux disease in neurologically impaired children. Sci Rep. 2020;10:11618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 125. | Vane DW, Harmel RP Jr, King DR, Boles ET Jr. The effectiveness of Nissen fundoplication in neurologically impaired children with gastroesophageal reflux. Surgery. 1985;98:662-667. [PubMed] |
| 126. | Cheung KM, Tse HW, Tse PW, Chan KH. Nissen fundoplication and gastrostomy in severely neurologically impaired children with gastroesophageal reflux. Hong Kong Med J. 2006;12:282-288. [PubMed] |
| 127. | Haseeb M, Thompson CC. Assessing implementation strategy and learning curve for transoral incisionless fundoplication as a new technique. Clin Endosc. 2022;55:751-752. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 128. | Bell RCW, Freeman K, Heidrick R, Ayazi S. Transoral incisionless fundoplication demonstrates durability at up to 9 years. Therap Adv Gastroenterol. 2021;14:17562848211004827. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 129. | Benias PC. Update on the Use of Transoral Incisionless Fundoplication for the Treatment of Gastroesophageal Reflux Disease. Gastroenterol Hepatol (N Y). 2021;17:333-335. [PubMed] |
| 130. | Bomman S, Malashanka S, Ghafoor A, Sanders DJ, Irani S, Kozarek RA, Ross A, Hubka M, Krishnamoorthi R. Safe implementation of transoral incisionless fundoplication as a new technique in a tertiary care center. Clin Endosc. 2022;55:630-636. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 131. | Mohan N, Matthai J, Bolia R, Agarwal J, Shrivastava R, Borkar VV; For Pediatric Gastroenterology Chapter of Indian Academy of Pediatrics, Indian Society of Pediatric Gastroenterology, Hepatology and Nutrition (ISPGHAN). Diagnosis and Management of Gastroesophageal Reflux Disease in Children: Recommendations of Pediatric Gastroenterology Chapter of Indian Academy of Pediatrics, Indian Society of Pediatric Gastroenterology, Hepatology and Nutrition (ISPGHAN). Indian Pediatr. 2021;58:1163-1170. [PubMed] |
| 132. | Robertson JO, Jarboe MD. Long-Term Outcomes of Transoral Incisionless Fundoplication in a High-Risk Pediatric Population. J Laparoendosc Adv Surg Tech A. 2018;28:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Thailand
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mahmoud S, Egypt; Sumi K, Japan; Tadros M, United States S-Editor: Chen YL L-Editor: A P-Editor: Chen YL