Published online Mar 16, 2023. doi: 10.4253/wjge.v15.i3.153
Peer-review started: November 9, 2022
First decision: November 22, 2022
Revised: November 26, 2022
Accepted: March 1, 2023
Article in press: March 1, 2023
Published online: March 16, 2023
Processing time: 126 Days and 16.9 Hours
Esophageal-gastro varices bleeding (EGVB) is the most widely known cause of mortality in individuals with cirrhosis, with an occurrence rate of 5% to 15%. Among them, gastric varices bleeding (GVB) is less frequent than esophageal varices bleeding (EVB), but the former is a more critical illness and has a higher mortality rate. At present, endoscopic variceal histoacryl injection therapy (EVHT) is safe and effective, and it has been recommended by relevant guidelines as the primary method for the treatment of GVB. However, gastric varices after endo
To assess the efficacy of aluminium phosphate gel (APG) combined with proton pump inhibitor (PPI) in preventing early rebleeding after EVHT in individuals with GVB.
Medical history of 196 individuals with GVB was obtained who were diagnosed using endoscopy and treated with EVHT in Shenzhen People's Hospital from January 2016 to December 2021. Based on the selection criteria, 101 patients were sorted into the PPI alone treatment group, and 95 patients were sorted into the PPI combined with the APG treatment group. The incidences of early rebleeding and corresponding complications within 6 wk after treatment were compared between both groups. Statistical methods were performed by two-sample t-test, Wilcoxon rank sum test and χ2 test.
No major variations were noted between the individuals of the two groups in terms of age, gender, Model for End-Stage Liver Disease score, coagulation function, serum albumin, hemoglobin, type of gastric varices, the dose of tissue glue injection and EV that needed to be treated simultaneously. The early rebleeding rate in PPI + APG group was 3.16% (3/95), which was much lower than that in the PPI group (12.87%, 13/101) (P = 0.013). Causes of early rebleeding: the incidence of gastric ulcer bleeding in the PPI + APG group was 2.11% (2/95), which was reduced in comparison to that in the PPI group (11.88%, 12/101) (P = 0.008); the incidence of venous bleeding in PPI + APG group and PPI group was 1. 05% (1/95) and 0.99% (1/101), respectively, and there was no significant difference between them (0.999). The early mortality rate was 0 in both groups within 6 wk after the operation, and the low mortality rate was related to the timely hospitalization and active treatment of all patients with rebleeding. The overall incidence of complications in the PPI + APG group was 12.63% (12/95), which was not significantly different from 13.86% (14/101) in the PPI group (P = 0.800). of abdominal pain in the PPI + APG group was 3.16% (3/95), which was lower than that in the PPI group (11.88%, 12/101) (P = 0.022). However, due to aluminum phosphate gel usage, the incidence of constipation in the PPI + APG group was 9.47% (9/95), which was higher than that in the PPI group (1.98%, 2/101) (P = 0.023), but the health of the patients could be improved by increasing drinking water or oral lactulose. No patients in either group developed spontaneous peritonitis after taking PPI, and none developed hepatic encephalopathy and ectopic embolism within 6 wk of EVHT treatment.
PPI combined with APG can significantly reduce the incidence of early rebleeding and pos
Core Tip: Gastric varices bleeding (GVB) is a serious life-threatening disease, and endoscopic variceal histoacryl injection therapy (EVHT) can effectively maintain hemostasis during the disease. Nevertheless, complications after EVHT, such as bleeding during drainage and ulceration at the injection site, can lead to early rebleeding. Currently, there are few clinical studies on preventing early rebleeding after EVHT in patients with GVB. We have found that using aluminium phosphate gel combined with proton pump inhibitor after EVHT could significantly reduce early rebleeding after endoscopic treatment in individuals with GVB.
- Citation: Zeng HT, Zhang ZL, Lin XM, Peng MS, Wang LS, Xu ZL. Aluminum phosphate gel reduces early rebleeding in cirrhotic patients with gastric variceal bleeding treated with histoacryl injection therapy. World J Gastrointest Endosc 2023; 15(3): 153-162
- URL: https://www.wjgnet.com/1948-5190/full/v15/i3/153.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i3.153
Cirrhosis is caused by various etiologies (alcoholic fatty liver, hepatitis virus infection, non-alcoholic fatty liver, drugs, genetic metabolic diseases, autoimmune diseases, etc.), characterized by chronic liver inflammation, pseudo-lobular formation, and regenerative nodules[1]. It can be clinically divided into the compensatory and decompensation stages. Patients in the compensatory stage may not have any clinical signs or symptoms, while patients in the decompensation stage are characterized by liver dysfunction and portal hypertension[2-4]. EGVB is the most prevalent cause of death in individuals with cirrhosis, with an annual occurrence rate of about 5% to 15%, a 6-week case fatality rate of 20% and an incidence of rebleeding within 1 year of 60%.
The incidence of GVB is lower than EVB, accounting for about 20% of venous bleeding[5]. However, GVB is more dangerous, and it is difficult to stop bleeding in this condition because GV)are in the submucosa of the stomach and the gastric mucosa is thicker than the esophageal mucosa making it relatively difficult to rupture and bleed under the same or greater blood flow pressure[6]. The bleeding after rupture can be fatal, and hemostasis is difficult.
There are numerous ways to clinically prevent and treat GVB, such as drugs, endoscopic therapy, interventional radiology and traditional surgery. EVHT is safe and effective and has been recommended as the main treatment strategy for GVB, following the relevant guidelines. The success rate of hemostasis can reach 97.1% to 100%[7,8]. Related studies have reported that patients after EVHT still have a rebleeding rate of about 15% to 23.7%[7,9]. Early rebleeding refers to active bleeding events (including melena, hematemesis, or hematochezia; decrease in systolic blood pressure > 20 mmHg or increase in heart rate > 20 beats/min; decrease in hemoglobin > 30 G/L without blood transfusion) in patients with varicose veins within 72 h to 6 wk after initial bleeding control[10]. The occurrence of rebleeding is related to complications such as bleeding of glue discharge ulcer and rebleeding of varicose veins. Current clinical guidelines on the prevention of complications after EVHT are recommended[10-12]. Treatment with a proton pump inhibitor (PPI) may be given. As a mucosal protective agent, aluminium phosphate gel (APG) can increase the pH of the stomach, promote the formation of blood clots at the bleeding site, and promote the healing of gastric mucosa[13].
This study aims to investigate whether PPI combined with APG can lower the occurrence of early rebleeding after endoscopic treatment in patients with GVB and to provide a reference for clinical treatment.
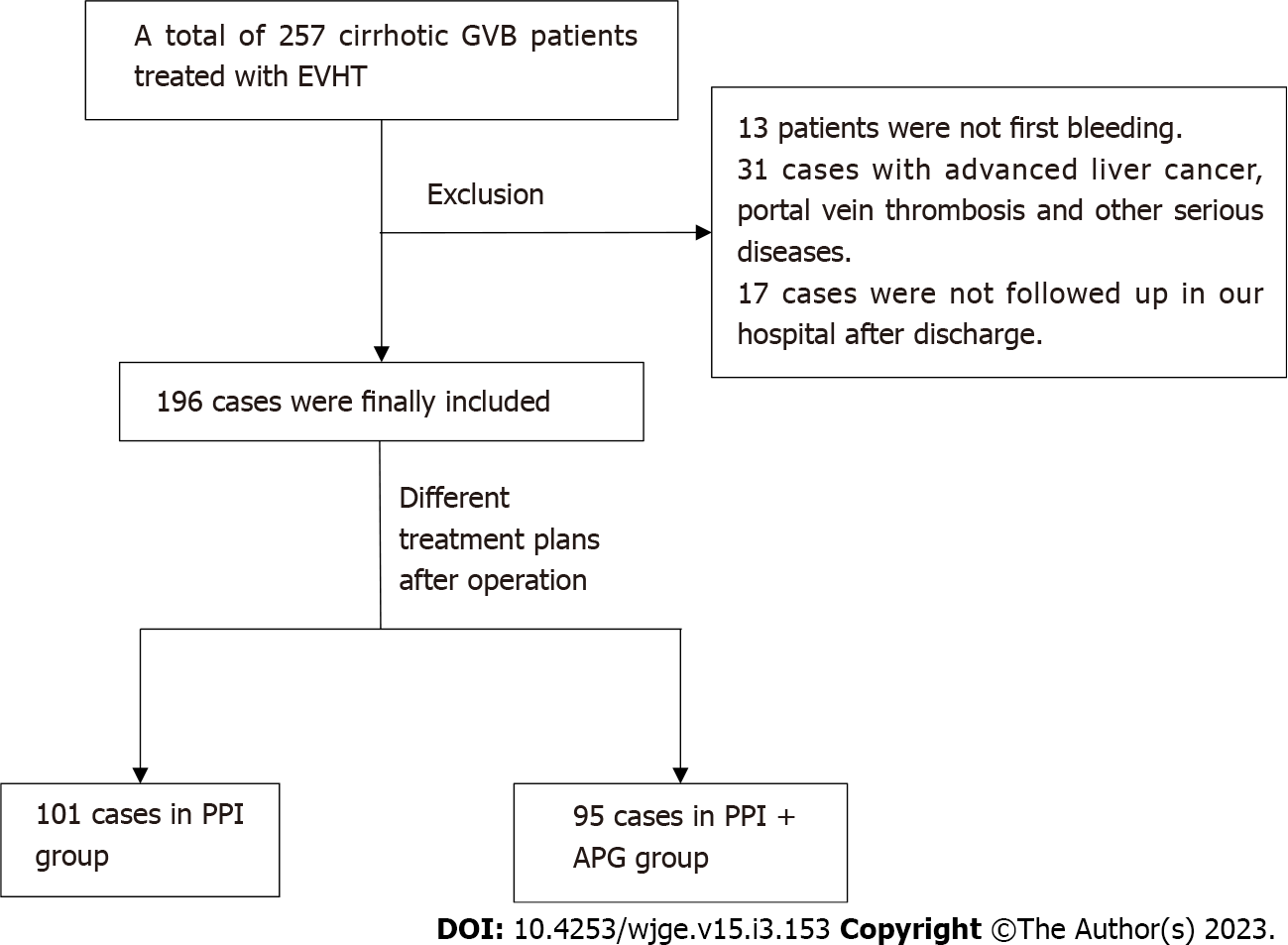
This study was a retrospective analysis of 257 individuals diagnosed with GVB by endoscopy and treated with EVHT in Shenzhen People's Hospital from January 2016 to December 2021. All patients were randomized to receive APG after EVHT. There were 13 patients with non-first bleeding, 31 patients with advanced liver cancer, portal vein thrombosis and other serious diseases and 17 patients discharged from the hospital were excluded. Finally, 196 cases were selected according to the standard. Based on the different postoperative treatment regimens for EVHT, 101 patients were divided into the PPI treatment group and 95 patients into the PPI combined with the APG treatment group, and the medical records of the two groups were collected respectively (the screening flow was shown in Figure 1). The approval for this research was given by the Ethics Committee of Shenzhen People's Hospital, and all patients consented to it.
(1) Individuals aged 18-80 years old, regardless of gender; (2) Individuals with GVB diagnosed by gastroscopy; and (3) Individuals who underwent EVHT were used in all patients.
(1) Individuals with incomplete clinical data; and (2) Individuals with other serious diseases (such as coronary heart disease, chronic renal insufficiency, advanced liver cancer, etc.) at the time of admission significantly affected the patients' prognosis.
All individuals included in this study underwent relevant examinations before the operation to comprehensively assess the patient conditions who signed an informed consent form for treatment. They were treated with EVHT using the "sandwich" method. Initially, 2.0 mL of 50% glucose solution was pre-stored in the injection needle, and then 2.0 mL of 50% glucose solution was injected into the bleeding target vein under endoscopy. According to the degree of varicosity, 0.5-2.0 mL of tissue glue was injected into each site, 2.0 mL 50% glucose was injected afterward, and finally, the injection needle was pulled out.
PPI treatment group: After endoscopic treatment, the patients in this group were given a conventional dose of PPI (rabeprazole 20 mg daily before breakfast) for 4 wk[14]. PPI combined with APG treatment group: Rabeprazole 20 mg daily before breakfast was administered orally for 4 consecutive weeks, and APG 20 g (Boryung Pharmaceutical Co., Ltd. 20 g) was added twice (about 30 min before breakfast and dinner) a day on the postoperative day for 4 consecutive weeks. All individuals were assessed, and those without contraindications were administered with non-elective postoperatively β receptor blockers (propranolol) to prevent rebleeding treatment. All patients were followed up and observed closely, and the patients with suspected rebleeding were re-hospitalized and underwent endoscopy along with immediate treatment.
Signs of early postoperative rebleeding in patients with GVB: Active bleeding events (melena, hematemesis, or hematochezia; decrease in systolic blood pressure > 20 mmHg or increase in heart rate > 20 beats/min; decrease in hemoglobin > 30 g/L without blood transfusion) within 72 h to 6 wk after the initial bleeding control. Early rebleeding was the primary outcome measure in this study. Other complications such as death, abdominal pain, ectopic embolization, and related adverse events were considered secondary outcome measures.
Statistical analyses were carried out using SPSS 25.0. The measurement data with normal distribution were presented as mean ± SD, and a two-sample t-test was utilized to compare the two groups, median (lower quartile, upper quartile) presented the measurement data with skewed distribution and to compare the results of two groups Wilcoxon rank sum test was performed. The number of cases and percentage presented the enumeration data, and the χ2 test was used for comparison between the two groups. A P value of < 0.05 was deemed statistically significant for all the calculated differences.
Table 1 demonstrates the basic conditions of individuals in both groups at the time of discharge after stable bleeding was counted. A comparison of different features of individuals in both groups was carried out; these include age (P = 0.245), gender (P = 0.289), Model for End-Stage Liver Disease score (P = 0.329), prothrombin activity (PTA, P = 0.157), fibrinogen (FIB, P = 0.064) and platelet count (PLT, P < 0.05). Serum albumin (ALB) (P = 0.622) and hemoglobin (Hb) (P = 0.524) were not statistically different. There was no significant difference in the number of patients taking beta blockers after discharge between the two groups (P = 0.586). Table 2 demonstrates categorizing the patients’ GV status according to Sarin Criteria[5]. Statistically significant variations were not observed between the PPI group and the PPI + APG group in terms of the GV type (GOV1 10 patients vs 12 patients, P = 0.545), (GOV2 50 patients vs 41 patients, P = 0.373), (GOV3 34 patients vs 38 patients, P = 0.358) and (IGV1 7 patients vs 4 patients, P = 0.408); in addition, 68 (67.33%) subjects in the PPI group and 69 (72.63%) subjects in the PPI + APG group with severe EV requiring concomitant endoscopic therapy did not differ significantly between both groups (P = 0.418). The mean value of histogel dosage in the PPI group was 2.22 ± 0.80 mL, which was not statistically different from 2.21 ± 0.76 mL in the PPI + APG group (P = 0.875).
| Characteristic | PPI group (n = 101) | PPI + APG group (n = 95) | P value |
| Age (yr) | 51.55 ± 12.23 | 53.57 ± 11.90 | 0.245 |
| Female/Male | 26/75 | 31/64 | 0.289 |
| MELD score | 10.07 ± 3.32 | 9.61 ± 3.24 | 0.329 |
| Prothrombin activity (%) | 68.53 ± 15.48 | 65.63 ± 12.90 | 0.157 |
| Fibrinogen (g/dL) | 2.30 ± 0.76 | 2.09 ± 0.80 | 0.064 |
| Platelet (109/L) | 102.21 ± 83.68 | 111.16 ± 100.57 | 0.498 |
| Albumin (g/dL) | 3.52 ± 0.47 | 3.48 ± 0.58 | 0.622 |
| Hemoglobin (g/dL) | 9.73 ± 2.15 | 9.55 ± 1.88 | 0.524 |
| Patients treated with beta blockers | 89 | 86 | 0.586 |
| Characteristic | PPI group (n = 101) | PPI + APG group (n = 95) | P value |
| GOV1 | 10 (9.90) | 12 (12.63) | 0.545 |
| GOV2 | 50 (49.50) | 41 (43.16) | 0.373 |
| GOV3 | 34 (33.66) | 38 (40.00) | 0.358 |
| IGV1 | 7 (6.93) | 4 (4.21) | 0.408 |
| Combine with EV need treatment | 68 (67.33) | 69 (72.63) | 0.418 |
| Amount of histoacryl (mL) | 2.22 ± 0.80 | 2.21 ± 0.76 | 0.875 |
The patients were followed up closely after the operation and returned to the hospital immediately if they had early rebleeding, and all of them underwent emergency gastroscopy and treatment. The cases of early esophageal rebleeding after EV treatment were excluded, and the cases of early gastric rebleeding after GV treatment were compared (Table 3). The incidence rate of early rebleeding in the PPI + APG group was 3.16% (3/95), which was considerably lower than that in the PPI group (12.87%, 13/101), and the difference was statistically significant (P = 0.013). The incidence of ulcer bleeding in the PPI + APG group was 2.11% (2/95), which was reduced compared to that in the PPI group (11.88%, 12/101) (P = 0.008); The incidence of venous bleeding was 1.05% (1/95) in the PPI + APG group and 0.99% (1/101) in the PPI group, (P > 0.999). There was no significant difference between the two groups. One patient (1.05%) in PPI + APG group needed a blood transfusion, which was lower than that in the PPI group ((9 patients, 8.91%), P = 0.030). Patients with venous bleeding in both groups needed a blood transfusion, and no considerable difference was observed between the two groups (P > 0.999). The re-hospitalization rate of the PPI + APG group was 2.11% (2/95), which was reduced compared to that in the PPI group (9.90%, 10/101), P = 0.023). The early mortality rate was 0 in both groups within 6 wk, and the reason for the low mortality rate was the timely hospitalization and treatment of all patients with early rebleeding.
| Characteristic | PPI group (n = 101) | PPI + APG group (n = 95) | P value |
| Early rebleeding | 13 (12.87) | 3 (3.16) | 0.013 |
| Source of rebleeding | |||
| Glue extrusion ulcer | 12 (11.88) | 2 (2.11) | 0.008 |
| Gastric varice | 1 (0.99) | 1 (1.05) | > 0.999 |
| Transfusion after rebleeding | |||
| Glue extrusion ulcer | 9 (8.91) | 1 (1.05) | 0.030 |
| Gastric varices | 1 (0.99) | 1 (1.05) | > 0.999 |
| Re-hospitalization | 10 (9.90) | 2 (2.11) | 0.023 |
| 6-wk mortality | 0 | 0 | > 0.999 |
As shown in Table 4, the overall complication rate was 13.86% (14/101) in the PPI group and 12.63% (12/95) in PPI + APG group, with no significant difference (P = 0.800). The incidence of abdominal pain in PPI + APG group was 3.16% (3/95); lower than that in PPI group (11.88%, 12/101, P = 0.022). The incidence of constipation in the PPI + APG group was 9.47% (9/95), higher than that in the PPI group (1.98%, 2/101) (P = 0.023). Constipation in PPI + APG group was improved by drinking more water or taking lactulose. There were no cases of spontaneous bacterial peritonitis after taking PPI in both groups and no cases of hepatic encephalopathy and ectopic embolism in both groups within 6 wk after the first EVHT treatment.
| Characteristic | PPI group (n = 101) | PPI + APG group (n = 95) | P value |
| Total complications | 14 (13.86) | 12 (12.63) | 0.800 |
| Abdominal pain | 12 (11.88) | 3 (3.16) | 0.022 |
| Constipation | 2 (1.98) | 9 (9.47) | 0.023 |
| Spontaneous peritonitis | 0 | 0 | > 0.999 |
| Ectopic embolism | 0 | 0 | > 0.999 |
| Hepatic encephalopathy | 0 | 0 | > 0.999 |
The incidence of GV is lower than that of EV because of the difference in the location of varicose veins in GV and EV. The varices of EV are mainly located in the lamina propria and submucosa, while GV is located in the submucosa, and the gastric mucosa is thicker than the esophageal mucosa[15]. Therefore, under the same blood pressure, GV is less likely to form varices on the mucosal surface, but they are usually larger than those formed by EV. This unique pathophysiological structure also determines the treatment difference of GVB from that of EVB. Endoscopic variceal ligation (EVL) is the preferred method for EVB as the first-line treatment and the prevention of rebleeding[16,17]. It is unsuitable for GVB because of the limited effect of ligation on submucosal deep branch veins and larger veins (diameter 2 cm), and gastric peristalsis can cause the ligature to fall off, increasing the risk of bleeding[18]. At present, relevant guidelines recommend EVHT as the preferred treatment for GVB, and the therapeutic effect is better than EVL, which has been confirmed by relevant studies[19,20].
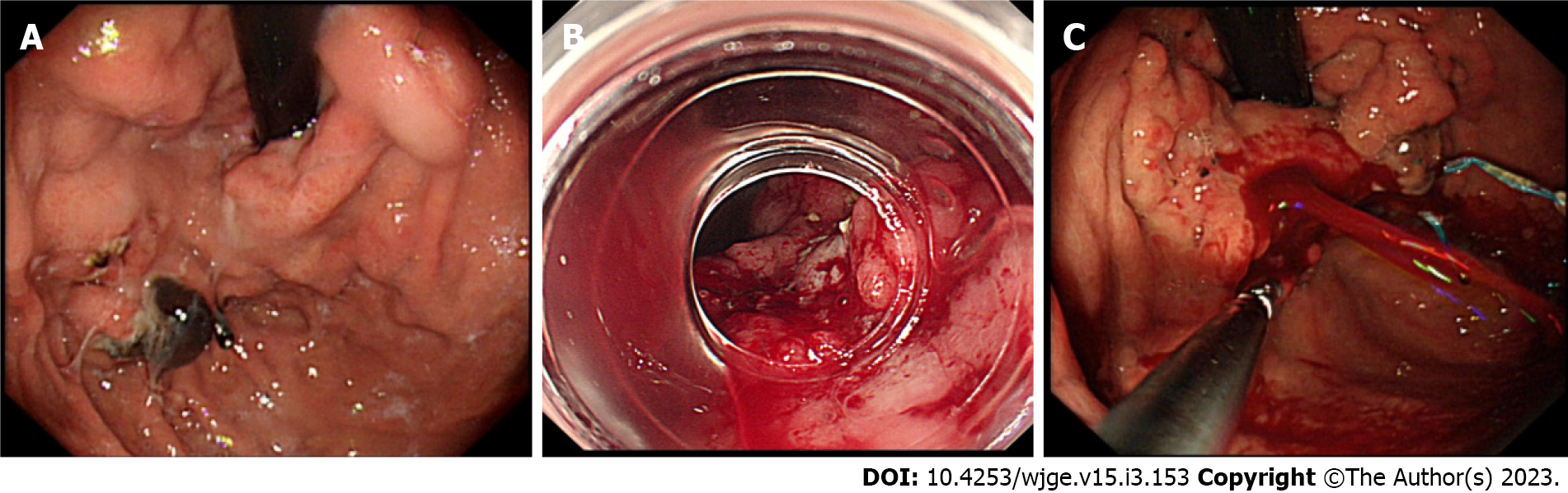
EVHT is primarily hemostatic as it functions by injecting tissue glue into the bleeding vein. Tissue glue is a rapid water-like solidification, which can quickly solidify in the blood in the presence of trace anions, forming a permanent intravascular embolism in a few seconds and blocking the bleeding veins[21]. However, the effect of tissue glue on vascular fibrosis is weak, failing to inhibit the formation of new blood vessels, often resulting in postoperative rebleeding. Currently, the causes of rebleeding are related to glue discharge ulcers and venous bleeding (Figure 2).
Tissue glue, as a foreign body, is rejected by the human body after being injected into blood vessels which are eventually eliminated through the gastric cavity in a process called glue expulsion[22]. Wang et al[23] found that after EVHT, patients began to discharge glue about 1 wk later, and about 4 wk later was the peak period of postoperative glue discharge. At this time, endoscopy could find various colors and forms of glue discharge ulcers, which was also the peak period of glue discharge ulcer bleeding[23]. Draining ulcer bleeding is multifactorial: (1) Bleeding from incomplete fibrosis of the occluding vessel due to inflammatory exudation at the injection site; (2) The histogel mixture did not completely enter the blood vessels and transferred into the extravascular gastric mucosa, causing inflammation and caseous necrosis of the mucosa and the formation of large ulcers; (3) Insufficient amount of tissue glue, which failed to effectively occlude the vessel; and (4) A small number of multisite injections are made, forming multi-site glue lined ulcers. In addition, varices that are not completely obliterated are also an important cause of early rebleeding[24]. In our study, there were 12 cases of bleeding ulcers in the PPI group and 1 in the PPI + APG group, accounting for 87.50% (14/16) of early rebleeding cases.
PPI is a kind of H+-K+-ATP enzyme inhibitor, the most important drug to clinically inhibit gastric acid secretion and treat digestive tract ulcers. It can also promote the healing of glue discharge ulcers [25]. It is also a routine method to prevent postoperative complications. However, some studies have reported that long-term use of PPI may increase the incidence of spontaneous peritonitis and hepatic encephalopathy in patients with cirrhosis[26]. APG is a mucosal protective agent that can neutralize gastric acid and protect the mucosa. Its active ingredient aluminum phosphate, can mix with gastric acid to form a relatively strong buffer system: Phosphate and aluminum ions. The former can combine with H + to rapidly increase the PH value in the stomach, which benefits blood clots' formation and stability in gastrointestinal bleeding patients. Its auxiliary ingredients, pectin and agar, are similar to the structure of natural mucus, which can form a layer of colloidal protective film on the surface of a postoperative ulcer to protect the gastric mucosa from damage after oral administration[27]. The combination of PPI and APG can theoretically promote the stabilization of blood clots at the bleeding site and the rapid healing of glue discharge ulcers in patients with GVB, ultimately reducing the incidence of early rebleeding.
In this retrospective study, the author found that the incidence of early rebleeding after EVHT in GVB patients treated with PPI + APG was 3.16% (3/95), significantly lower than that in the PPI group (12.87%, 13/101). As APG had been shown to promote ulcer healing, the incidence of bleeding from a drained ulcer after EVHT was 2.11% (2/95) in GVB patients treated with PPI + APG, which was significantly lower than the 11.88% (12/101) in PPI group. However, in terms of gastric vein bleeding, no statistical difference was observed between the two groups. The use of APG reduces the incidence of postoperative abdominal pain following EVHT in patients with GVB. Although the use of APG increased constipation in the patients, they improved both by extensive drinking of water and taking lactulose. None of the patients in either group developed spontaneous peritonitis after taking PPI. There were no cases of hepatic encephalopathy, ectopic embolism, or death within 6 wk after EVHT in either group, which was supported by timely endoscopic treatment for all patients with early rebleeding and rapid clearance of the hematochezia intestinalis.
However, this study has some limitations: (1) This study is retrospective; (2) The sample size of this experiments is small, and it is a single-center study. The incidence of early rebleeding in patients is related to the experience of endoscopists, diet along with other factors. There are a lot of confounding factors, and the applicability of the experimental results is limited; and (3) This study has conducted a follow-up period of only 6 wk. It has only investigated the occurrence of early rebleeding and related secondary outcome measures after EVHT in patients. Further studies are lacking regarding some clinical data and long-term indicators (such as survival, number of hospitalizations, long-term treatment costs, etc.) after the end of 6 wk of the follow-up. It is also possible that other mucosal protective agents may reduce the incidence of early rebleeding by promoting ulcer healing after EVHT treatment, but further studies are needed to prove this. Therefore, follow-up clinical randomized controlled experiments with prospective, multi-center large sample with medium and long-term follow-up is also needed.
The combination of APG and PPI therapy after endoscopic EVHT for cirrhotic patients with GVB can promote the healing of gastric glue ulcers and relieve abdominal pain in patients. Moreover, it can significantly reduce the incidence of early rebleeding after EVHT. It is also possible that other mucosal protective agents may reduce the incidence of early rebleeding by promoting ulcer healing after EVHT treatment, but further studies are needed to prove this.
The incidence of early rebleeding after endoscopic variceal histoacryl injection therapy (EVHT) of varicose veins in the fundus of the stomach is high, which may lead to serious consequences. It is very important to reduce the incidence of early rebleeding.
Reducing the incidence of early rebleeding after EVHT treatment reduces the risk of patients and may extend their life expectancy. Proton pump inhibitor (PPI) treatment has been found to reduce the incidence of early rebleeding. Aluminium phosphate gel (APG) can promote the healing of gastric ulcers. Can the combination of APG and PPI further reduce the incidence of early rebleeding?
This study aimed to verify whether the combination of APG and PPI can reduce the incidence of early rebleeding after EVHT.
We randomly divided patients after EVHT into two groups. One group was treated on PPI after EVHT, and the other group took PPI in combination with APG. We statistically analyzed the data of both groups and observed the early rebleeding rates in both groups.
The early rebleeding rate in PPI + APG group was 3.16% (3/95), which was much lower than that in the PPI group (12.87%, 13/101). Causes of early rebleeding: The incidence of gastric ulcer bleeding in the PPI + APG group was 2.11% (2/95), which was reduced in comparison to that in the PPI group (11.88%, 12/101); the incidence of venous bleeding in PPI + APG group and PPI group was 1.05% (1/95) and 0.99% (1/101), respectively, and there was no significant difference between them. The incidence of abdominal pain in the PPI + APG group was 3.16% (3/95), which was lower than that in the PPI group (11.88%, 12/101).
PPI combined with APG can significantly reduce the incidence of early rebleeding and postoperative abdominal pain in cirrhotic patients with GVB after taking EVHT.
The combination of APG with PPI can reduce the bleeding incidence of gastric ulcers after EVHT.
| 1. | Mueller S, Chen C, Mueller J, Wang S. Novel Insights into Alcoholic Liver Disease: Iron Overload, Iron Sensing and Hemolysis. J Transl Int Med. 2022;10:92-124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (1)] |
| 2. | Berzigotti A. Advances and challenges in cirrhosis and portal hypertension. BMC Med. 2017;15:200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 70] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 3. | Tayyem O, Bilal M, Samuel R, Merwat SK. Evaluation and management of variceal bleeding. Dis Mon. 2018;64:312-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Cotrim HP, Parise ER, Figueiredo-Mendes C, Galizzi-Filho J, Porta G, Oliveira CP. Nonalcoholic Fatty Liver Disease Brazilian Society of Hepatology Consensus. Arq Gastroenterol. 2016;53:118-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343-1349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 789] [Cited by in RCA: 873] [Article Influence: 25.7] [Reference Citation Analysis (42)] |
| 6. | Morrison JD, Mendoza-Elias N, Lipnik AJ, Lokken RP, Bui JT, Ray CE Jr, Gaba RC. Gastric Varices Bleed at Lower Portosystemic Pressure Gradients than Esophageal Varices. J Vasc Interv Radiol. 2018;29:636-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Lo GH, Lin CW, Tai CM, Perng DS, Chen IL, Yeh JH, Lin HC. A prospective, randomized trial of thrombin versus cyanoacrylate injection in the control of acute gastric variceal hemorrhage. Endoscopy. 2020;52:548-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 8. | Robles-Medranda C, Oleas R, Valero M, Puga-Tejada M, Baquerizo-Burgos J, Ospina J, Pitanga-Lukashok H. Endoscopic ultrasonography-guided deployment of embolization coils and cyanoacrylate injection in gastric varices versus coiling alone: a randomized trial. Endoscopy. 2020;52:268-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 75] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 9. | Bick BL, Al-Haddad M, Liangpunsakul S, Ghabril MS, DeWitt JM. EUS-guided fine needle injection is superior to direct endoscopic injection of 2-octyl cyanoacrylate for the treatment of gastric variceal bleeding. Surg Endosc. 2019;33:1837-1845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 64] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 10. | Yuan P. The Neural Code of Working Memory Maintenance. J Neurosci. 2019;39:9883-9884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Sung JJ, Chiu PW, Chan FKL, Lau JY, Goh KL, Ho LH, Jung HY, Sollano JD, Gotoda T, Reddy N, Singh R, Sugano K, Wu KC, Wu CY, Bjorkman DJ, Jensen DM, Kuipers EJ, Lanas A. Asia-Pacific working group consensus on non-variceal upper gastrointestinal bleeding: an update 2018. Gut. 2018;67:1757-1768. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 227] [Cited by in RCA: 201] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 12. | Gralnek IM, Dumonceau JM, Kuipers EJ, Lanas A, Sanders DS, Kurien M, Rotondano G, Hucl T, Dinis-Ribeiro M, Marmo R, Racz I, Arezzo A, Hoffmann RT, Lesur G, de Franchis R, Aabakken L, Veitch A, Radaelli F, Salgueiro P, Cardoso R, Maia L, Zullo A, Cipolletta L, Hassan C. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:a1-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 472] [Cited by in RCA: 520] [Article Influence: 47.3] [Reference Citation Analysis (0)] |
| 13. | Zhang Y, Yan X, Huang Y, Nie D, Wang Y, Chang H, Zhang Y, Yao W, Li K. Efficacy of oral steroid gel in preventing esophageal stricture after extensive endoscopic submucosal dissection: a randomized controlled trial. Surg Endosc. 2022;36:402-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Ghoz H, Patel P, Stancampiano F, Patel S, Fox EA, Yousaf MB, Omer M, Heckman MG, Spiegel MR, Palmer WC. Proton-pump-inhibitor use associated with lower short-term rebleeding and mortality in patients receiving esophageal variceal band ligation: a retrospective cohort study. Eur J Gastroenterol Hepatol. 2020;32:1571-1578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Ryan BM, Stockbrugger RW, Ryan JM. A pathophysiologic, gastroenterologic, and radiologic approach to the management of gastric varices. Gastroenterology. 2004;126:1175-1189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 230] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 16. | Henry Z, Patel K, Patton H, Saad W. AGA Clinical Practice Update on Management of Bleeding Gastric Varices: Expert Review. Clin Gastroenterol Hepatol. 2021;19:1098-1107.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 116] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 17. | Yoshiji H, Nagoshi S, Akahane T, Asaoka Y, Ueno Y, Ogawa K, Kawaguchi T, Kurosaki M, Sakaida I, Shimizu M, Taniai M, Terai S, Nishikawa H, Hiasa Y, Hidaka H, Miwa H, Chayama K, Enomoto N, Shimosegawa T, Takehara T, Koike K. Evidence-based clinical practice guidelines for liver cirrhosis 2020. Hepatol Res. 2021;51:725-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 147] [Article Influence: 29.4] [Reference Citation Analysis (0)] |
| 18. | Seo YS. Prevention and management of gastroesophageal varices. Clin Mol Hepatol. 2018;24:20-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 75] [Article Influence: 8.3] [Reference Citation Analysis (1)] |
| 19. | Park SJ, Kim YK, Seo YS, Park SW, Lee HA, Kim TH, Suh SJ, Jung YK, Kim JH, An H, Yim HJ, Jang JY, Yeon JE, Byun KS. Cyanoacrylate injection versus band ligation for bleeding from cardiac varices along the lesser curvature of the stomach. Clin Mol Hepatol. 2016;22:487-494. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Ríos Castellanos E, Seron P, Gisbert JP, Bonfill Cosp X. Endoscopic injection of cyanoacrylate glue versus other endoscopic procedures for acute bleeding gastric varices in people with portal hypertension. Cochrane Database Syst Rev. 2015;CD010180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 21. | Chang CJ, Hou MC, Lin HC, Lee HS, Liao WC, Su CW, Lee SD. The safety and probable therapeutic effect of routine use of antibiotics and simultaneously treating bleeding gastric varices by using endoscopic cyanoacrylate injection and concomitant esophageal varices with banding ligation: a pilot study. Gastrointest Endosc. 2010;71:1141-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Matsumoto A, Takimoto K. Gastric fundal varices: new aspects of nonsurgical treatment in Japan. Nat Clin Pract Gastroenterol Hepatol. 2006;3:4-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Wang YM, Cheng LF, Li N, Wu K, Zhai JS, Wang YW. Study of glue extrusion after endoscopic N-butyl-2-cyanoacrylate injection on gastric variceal bleeding. World J Gastroenterol. 2009;15:4945-4951. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 33] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 24. | Luo X, Xiang T, Wu J, Wang X, Zhu Y, Xi X, Yan Y, Yang J, García-Pagán JC, Yang L. Endoscopic Cyanoacrylate Injection Versus Balloon-Occluded Retrograde Transvenous Obliteration for Prevention of Gastric Variceal Bleeding: A Randomized Controlled Trial. Hepatology. 2021;74:2074-2084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 64] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 25. | Ward RM, Kearns GL. Proton pump inhibitors in pediatrics: mechanism of action, pharmacokinetics, pharmacogenetics, and pharmacodynamics. Paediatr Drugs. 2013;15:119-131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 135] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 26. | Alaniz C, Mohammad RA, Welage LS. High-dose PPIs in patients with variceal hemorrhage. Arch Intern Med. 2010;170:1698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 27. | Nie D, Yan X, Huang Y. Efficacy of hydrocortisone sodium succinate and aluminum phosphate gel for stricture prevention after ≥3/4 circumferential endoscopic submucosal dissection. J Int Med Res. 2020;48:300060519894122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: García-Compeán D, Mexico; Netto ERA, Brazil; Sano W, Japan S-Editor: Wang JL L-Editor: A P-Editor: Wang JL