Published online Feb 16, 2023. doi: 10.4253/wjge.v15.i2.77
Peer-review started: December 14, 2022
First decision: December 29, 2022
Revised: January 2, 2023
Accepted: January 16, 2023
Article in press: January 16, 2023
Published online: February 16, 2023
Processing time: 61 Days and 8.7 Hours
The incidence of intestinal malrotation in adults has been reported to only be about 0.2%. Duodenal web as a cause of intestinal obstruction is rare, with an incidence of about 1:20000-1:40000. Furthermore, when described, these con
We report a case of a middle-aged woman with intestinal malrotation who pre
Both intestinal malrotation and duodenal webs are infrequently encountered in the adult population. These pathologies can also present with nonspecific abdominal symptoms such as chronic abdominal pain and nausea. Hence, providers might not consider these pathologies in the differential for patients who present with vague symptoms which can lead to delay in management and increased mortality and morbidity.
Core Tip: Intestinal malrotation and duodenal web are gut pathologies that rarely occur or become symptomatic in the adult population. It is even rarer to see an association between the two which leads to intestinal obstruction. Furthermore, adults may present with vague gastrointestinal symptoms which can delay management and increase mortality. We report a case of intestinal obstruction due to a duodenal web in the setting of malrotation in a middle-aged female.
- Citation: Chew K, Bellemare S, Kumar A. Packed with pills - obstructing duodenal web in the setting of intestinal malrotation: A case report. World J Gastrointest Endosc 2023; 15(2): 77-83
- URL: https://www.wjgnet.com/1948-5190/full/v15/i2/77.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i2.77
The incidence of malrotation is around 1:500 and the symptomatic incidence is about 1:6000[1]. The incidence of duodenal web as a cause of intestinal obstruction is 1:10000-1:40000[2]. Intestinal malrotation is associated with various congenital obstructive anomalies, including duodenal atresia and stenosis. However, intestinal obstruction due to a duodenal web in the setting of malrotation has rarely been reported in the literature.
Both these pathological entities can present with vague symptoms such as abdominal pain and nausea. This can lead to delayed diagnosis and treatment, increasing mortality and morbidity. Furthermore, when described, this condition is usually seen in early life and very infrequently in adulthood.
Given the rarity of these diseases, there is limited data in the literature that can help guide better treatment options. Hence, we present a case of a middle-aged woman with intestinal malrotation who developed partial obstruction secondary to a duodenal web.
A 53-year-old woman presenting with three-month history of right-sided abdominal pain, early satiety, worsening nausea, and weight loss.
Symptoms started three months before presentation with worsening right-sided abdominal pain associated with early satiety, nausea and a 22-pound weight loss.
Patient has a past medical history of lupus nephritis status post renal transplant and known intestinal malrotation. Computed tomography (CT) of the abdomen showed large residual debris in the distal stomach and possible gastric outlet obstruction, without suspicious mass lesions or lymphadenopathy. The patient had been noted to have a mildly dilated duodenum and stomach on prior imaging and esophagogastroduodenoscopy (EGD), thought then to be due to her intestinal malrotation.
The patient denied any family history of malignant tumors or abdominal pathologies.
On physical examination, the vital signs were as follows: body temperature, 36.9 ℃; blood pressure, 118/77 mmHg; heart rate, 76 beats per min; respiratory rate, 18 breaths per min. Abdominal exam with no tenderness to palpation, non-distended, normal bowel sounds heard. No lymphadenopathy noted.
Liver enzymes and bilirubin were normal (aspartate aminotransferase 22 U/L, alanine aminotransferase 14 U/L, total bilirubin 0.3 mg/dL, direct bilirubin 0.2 mg/dL, albumin 4.2 g/dL). No abnormalities were found on routine blood and urine analysis.
After presenting with the above concerning symptoms, she underwent another EGD. This demonstrated worsened gastric and intestinal distention with numerous retained pills in a deformed first portion of the duodenum (Figure 1). The endoscope could not be advanced past this region. Although no fixed obstruction was noted, it appeared that this persistent, partial gastric outlet obstruction was the etiology of her symptoms. Patient’s colonoscopy was unremarkable. Both an upper gastrointestinal series (Figure 2) and CT showed marked distention of the proximal duodenum and multiple pills present, with the second portion of the duodenum appearing normal. Additionally, given the presence of a windsock sign on the upper gastrointestinal (GI) series, a duodenal web was on the differential diagnosis. The differential also included Ladd’s bands, fibrous, compressive bands that are associated with intestinal malrotation.
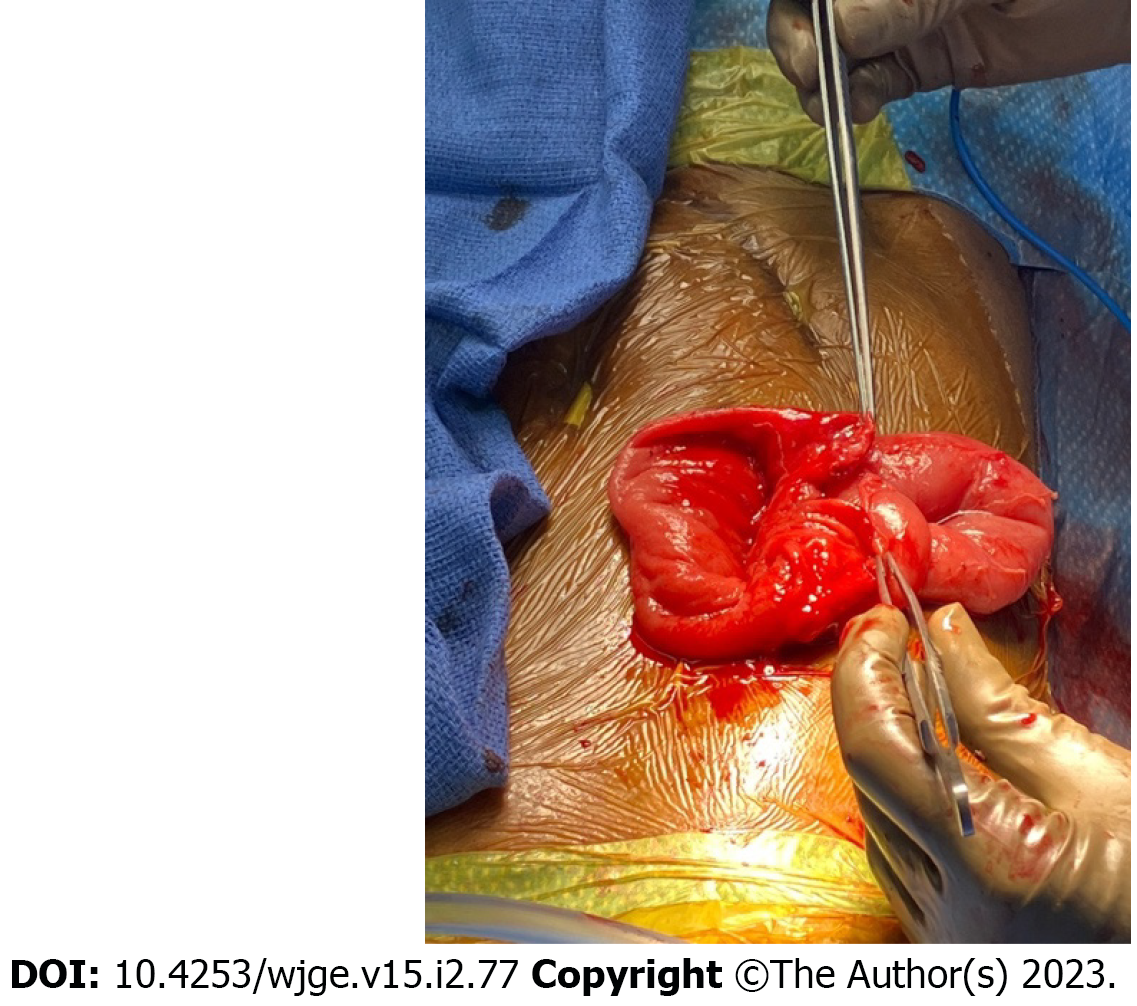
The patient subsequently underwent surgical intervention. During the laparoscopic procedure, adhesions between the duodenum, retroperitoneum and liver were initially seen and lysed. However, they were not true Ladd’s bands because they were not responsible for the obstruction. The exploratory laparotomy ultimately revealed a duodenal web with two lumens.
The final diagnosis was partial obstruction from duodenal web in the setting of intestinal malrotation.
During the surgical intervention, the duodenal web was resected, opening the duodenum (Figure 3). There were over 150 pill capsules, likely those that the patient was taking for immunosuppression, that were removed (Figure 4).
The patient is doing well after this intervention, as she has regained her weight and is no longer suffering from abdominal pain.
Intestinal malrotation is a developmental anomaly of the midgut. In this condition, any deviation from a normal intestinal rotation around the superior mesenteric artery affects the process of fixation in the peritoneal cavity[3,4]. Rotational anomaly of the midgut is uncommon in adults. This disease is usually symptomatic during infancy, with nearly 90% of patients requiring medical intervention during the first year of life[5].
The incidence of intestinal malrotation in adults has been reported to only be about 0.2%[6]. However, certain cases are not symptomatic until much later in life. In adults who become symptomatic with an acute presentation, they may present with symptoms of nausea, vomiting, abdominal pain, and constipation. Peritoneal bands can also form and compress superior mesenteric vessels, leading to bowel infarction and obstruction. This can present with signs and symptoms of volvulus. Patients with chronic presentations usually present with vague abdominal pain and recurrent vomiting[5,7]. Though often difficult to diagnose, rapid recognition of these pathologies and prompt surgical treatment usually lead to successful outcomes.
The gold standard in diagnosing intestinal malrotation is an upper GI series. Any deviation of the ligament of Treitz from just left of the midline at the level of the gastroduodenal junction is diagnostic for malrotation[1]. A contrast barium enema (BE) can be used to help define the location of the cecum if an upper GI series is indeterminate. A contrast BE has been replaced as the gold standard for diagnosis given 20%-40% of confirmed malrotation cases have a normal cecal position[8]. A CT scan can also be used to identify abnormal intestinal locations.
The classical treatment for intestinal malrotation is the Ladd procedure. For patients with known intestinal malrotation presenting with symptoms of intestinal obstruction, peritoneal fibrous bands - also known as Ladd’s bands - should be suspected. This procedure can be performed either laparoscopic or open, with similar outcomes[9]. During the procedure, the mesentery is untwisted, any Ladd’s bands are dissected, and the small bowel is positioned on the right side of the abdominal cavity while the large bowel is positioned on the left[1]. An appendectomy is usually performed as appendicitis can lead to a misdiagnosis. The Ladd procedure is performed with a goal to reduce the risk of intestinal ischemia and volvulus by widening the mesenteric base and locating the small intestine.
Duodenal web as a cause of intestinal obstruction is rare, with an incidence of about 1:20000-1:40000[2]. The concurrence of both intestinal malrotation and duodenal web leading to bowel obstruction is even rarer. The failure of recanalization of the duodenal lumen leaves behind a thin web consisting of the mucosa and submucosa without the muscular layer. Peristalsis causes the diaphragm to balloon distally, resulting in the classic appearance of a wind-sock[10,11]. This windsock sign can be visualized on sonography, upper GI series and endoscopy. Patients usually present early in life with evidence of proximal bowel obstruction; development of symptoms as an adult is very atypical.
Adults who develop a duodenal web usually present with upper abdominal distension, postprandial pain, and intermittent emesis secondary to partial or complete duodenal obstruction. However, nonspecific abdominal symptoms may also be observed. Moreover, this fenestrated membrane could be a site of impaction of food residues or foreign bodies[12]. In our case, the web caused a large buildup of pills at the duodenum. Diagnosis is made using contrast radiography or endoscopy, with the latter being much more sensitive as it can reveal the dilatation of the duodenum and the protrusion of the web in the lumen[13,14]. However, if one fails to visualize the second and third parts of the duodenum, a duodenal web may be missed[15].
Surgical treatment with complete excision of the web is the mainstay of management. If the excision is incomplete, the duodenal web may regrow and lead to recurrent obstruction. Before the mid-1980s, surgical repair was the only treatment available for duodenal webs, with endoscopy being relegated to a diagnostic role. However, with the advancement of therapeutic endoscopic techniques, treatment with procedures such as endoscopic membranotomy with laser, sphincterotome, high-frequency-wave snare/cutter, hot biopsy forceps, insulated-tip diathermic knife and needle knife have been reported[16-19]. It has been suggested that therapeutic endoscopy may be the preferred method of treatment of duodenal webs in adults given its efficacy, lack of invasiveness, is not associated with complications such as adhesion development, involves shorter hospital stay, and the procedures sometimes can be performed without general anesthesia[20].
The aim of this case report is to present a rare case of intestinal obstruction due to a duodenal web in the setting of malrotation in a middle-aged female. Both intestinal malrotation and duodenal webs are infrequently encountered in the adult population, and it is even rarer to see an association between the two. These conditions can present with vague symptoms such as chronic abdominal pain, which can lead to misdiagnosis, delay in management, and increased mortality and morbidity. Although the presence of both pathologies concomitantly is a very rare entity, duodenal web should be looked for and excluded in all cases of malrotation. Diagnosis can be made via endoscopy or contrast radiography. Although surgical treatment with excision of the duodenal web is the mainstay of management, given growing evidence in the literature, endoscopic management should also be considered. To date, reports of endoscopic treatment for duodenal webs have been free of significant complications. However, when considering treatment options, multiple factors should play a part in the decision, including patient’s risk factors and technical abilities of the endoscopist. We present this case to increase awareness of this diagnosis, aiming to prevent delay of definitive diagnosis and management.
| 1. | Ingoe R, Lange P. The Ladd's procedure for correction of intestinal malrotation with volvulus in children. AORN J. 2007;85:300-8; quiz 309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Beeks A, Gosche J, Giles H, Nowicki M. Endoscopic dilation and partial resection of a duodenal web in an infant. J Pediatr Gastroenterol Nutr. 2009;48:378-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Gamblin TC, Stephens RE, Jr, Johnson RK, Michael R. Adult malrotation: A case report and review of the literature. Curr Surg. 2003;60:517-520. [RCA] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 93] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 4. | Williams H. Green for danger! Arch Dis Child Educ Pract Ed. 2007;92:ep87-ep91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Vukić Z. Presentation of intestinal malrotation syndromes in older children and adults: report of three cases. Croat Med J. 1998;39:455-457. [PubMed] |
| 6. | Emanuwa OF, Ayantunde AA, Davies TW. Midgut malrotation first presenting as acute bowel obstruction in adulthood: a case report and literature review. World J Emerg Surg. 2011;6:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 59] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Dietz DW, Walsh RM, Grundfest-Broniatowski S, Lavery IC, Fazio VW, Vogt DP. Intestinal malrotation: a rare but important cause of bowel obstruction in adults. Dis Colon Rectum. 2002;45:1381-1386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 32] [Reference Citation Analysis (0)] |
| 8. | Murphy FL, Sparnon AL. Long-term complications following intestinal malrotation and the Ladd's procedure: a 15 year review. Pediatr Surg Int. 2006;22:326-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Palanivelu C, Rangarajan M, Shetty AR, Jani K. Intestinal malrotation with midgut volvulus presenting as acute abdomen in children: value of diagnostic and therapeutic laparoscopy. J Laparoendosc Adv Surg Tech A. 2007;17:490-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Krieg EG. DUODENAL DIAPHRAGM. Ann Surg. 1937;106:33-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | al-Kawas FH. Management of a duodenal web by endoscopic laser therapy. Gastrointest Endosc. 1989;35:113-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Gupta R, Mathur P, Gubbi S, Gupta PK, Shukla R, Bhandari A. More Distally Located Duodenal Webs: A Case Series. J Neonatal Surg. 2016;5:56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Madura JA, Goulet RJ Jr, Wahle DT. Duodenal webs in the adult. Am Surg. 1991;57:607-614. [PubMed] |
| 14. | Mousavi SA, Karami H, Saneian H. Congenital duodenal obstruction with delayed presentation: seven years of experience. Arch Med Sci. 2016;12:1023-1027. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Evans J, Miranda R, Stanton Jr PE. Double duodenal webs in an adult. South Med J. 1989;82:366-368. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Kay GA, Lobe TE, Custer MD, Hollabaugh RS. Endoscopic laser ablation of obstructing congenital duodenal webs in the newborn: a case report of limited success with criteria for patient selection. J Pediatr Surg. 1992;27:279-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 22] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Torroni F, De Angelis P, Caldaro T, di Abriola GF, Ponticelli A, Bergami G, Dall'Oglio L. Endoscopic membranectomy of duodenal diaphragm: pediatric experience. Gastrointest Endosc. 2006;63:530-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Barabino A, Gandullia P, Arrigo S, Vignola S, Mattioli G, Grattarola C. Successful endoscopic treatment of a double duodenal web in an infant. Gastrointest Endosc. 2011;73:401-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | DiMaio CJ, Kamal N, Hogan CM, Midulla PS. Pediatric therapeutic endoscopy: endoscopic management of a congenital duodenal web. Gastrointest Endosc. 2014;80:166-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Rosario MT, Alves IM, Carneiro AV, Ventura AM, Sales-Luis A. Adult duodenal web: endoscopic management. Endoscopy. 1993;25:483-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American College of Gastroenterology, 63535.
Specialty type: Medicine, research and experimental
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Atanasova EG, Bulgaria; Rezus E, Romania S-Editor: Wang LL L-Editor: A P-Editor: Wang LL