Published online Nov 16, 2023. doi: 10.4253/wjge.v15.i11.666
Peer-review started: May 10, 2023
First decision: July 4, 2023
Revised: August 3, 2023
Accepted: September 22, 2023
Article in press: September 22, 2023
Published online: November 16, 2023
Processing time: 183 Days and 17.6 Hours
Fibrovascular polyps are rare type of esophageal submucosal neoplasms. They are highly vascularized and can cause difficulty swallowing and even fatal complications such as uncontrolled bleeding and death caused by asphyxiation in case of tumor migration to oropharynx. In the article we describe a novel hybrid technique to surgical treatment – an endoscopic submucosal dissection with laparoscopic removal of the tumor.
The patient with a giant fibrovascular esophageal polyp presented with cough, discomfort in the throat, difficulty swallowing, and an episode of tumor migration into oropharynx. The patient was investigated with several imaging studies and was diagnosed with a giant highly vascularized esophageal fibrovascular polyp. The follow-up period of eight months accompanied with no complications.
This method has been shown to have comparable rates of recurrence and a low risk of complications.
Core Tip: In our case the patient was investigated with several imaging studies and was diagnosed with a giant highly vascularized esophageal fibrovascular polyp. It is crucial to consider the size and vascularization of fibrovascular polyps when assume endoscopic removal as a treatment option and to carefully plan the surgical technique to avoid difficulties or discomfort during the procedure. However, there is an alternative approach to traditional surgical removal known as the endoscopic approach that can be both safe and effective for treating giant fibrovascular polyps in the esophagus. Therefore, the aim of our study is to demonstrate demonstrate a novel hybrid technique to surgical treatment – an endoscopic submucosal dissection with laparoscopic removal of the tumor.
- Citation: Dzhantukhanova S, Avetisyan LG, Badakhova A, Starkov Y, Glotov A. Hybrid laparo-endoscopic access: New approach to surgical treatment for giant fibrovascular polyp of esophagus: A case report and review of literature. World J Gastrointest Endosc 2023; 15(11): 666-675
- URL: https://www.wjgnet.com/1948-5190/full/v15/i11/666.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i11.666
Fibrovascular polyp (FVP) are rare (approximately 0.03% of esophageal tumors), benign, richly vascularized tumors of the esophagus or hypopharynx[1]. The etiology of this disease has yet to be well-known. Esophageal fibrovascular polyps arise from the submucosal layer of the esophagus and usually are covered with normal mucosa, mostly appearing from the esophagus's upper third. Also, the lesions can be attached to the inferior aspect of the cricopharyngeal muscle and often have a stalk. Histologically the polyp contains loose or dense fibrous tissue, adipose tissue, and vascular structures[2].
In the early stages, FVP are clinically asymptomatic. The clinical symptoms correlate with the size of the tumor. The most common complaints are dysphagia, chest discomfort, and foreign body sensation[2]. There can also present other symptoms, such as odynophagia, dyspnea, coughing, neck pain, respiratory distress, and gastrointestinal bleeding[3].The most common complications that can cause even fatal exits are fatal bleeding and airway obstruction due to the aspiration of a tumor.
Even though in the modern world of the 21st century there are a lot of technologies and facilitating methods of diagnosis and treatment, the difficulties are still relevant. Furthermore, depending on the size of the polyp, there can be either endoscopic or surgical resection[4].
A 70-year-old female presented to the endoscopic surgical department of the A. V. Vishnevsky National Medical Research Center of Surgery in October 2022.
On admission, the patient complained of cough, dysphagia, discomfort in the throat, and the presence of large soft mass in the esophagus with episodes of its migration into oropharynx. The patient was examined.
During the last 5 years, a tumor was discovered during the examination and an episode of tumor migration into oropharynx.
The patient has consistently maintained a state of general well-being throughout her life, without encountering notable medical complications. Nevertheless, the patient mentioned that she has experienced persistent elevation of blood pressure, for which she received a diagnosis of stage 1 arterial hypertension (measuring between 140-145 mm Hg). In an effort to regulate her blood pressure levels, perindopril and indapamide in combination (marketed as Noliprel) were prescribed for her.
No allergies, recent infections, or harmful habits (such as smoking, alcohol consumption, or drug use) were reported. There is no family or personal history of genetic hypertension/cardiovascular issues; the elevated pressure seems to be linked to lifestyle factors. Apart from the prescribed anti hypertensives, the patient did not mention the use of any concurrent medications or supplements.
The patient is married and has two daughters. No significant family medical history of diseases or conditions prono
The Patient observed without any signs of visible immediate discomfort. Upon admission, the vital signs were measured: blood pressure at 140/80 mmHg, heart rate at 72 bpm, temperature at 98.6°F (37°C), and oxygen saturation at 98%. A thorough examination of all organ systems was done, and no abnormalities were found.
During the palpation the abdomen was non-tender, without masses, and both the liver and spleen were non-palpable below the rib cage. No palpable lymph nodes were found in cervical, axillary, or inguinal areas. Patient reported no discomfort during palpation.
The blood count and coagulation assessment results revealed that all measured parameters resided comfortably within established normative reference intervals. The concentration of Albumin manifested at 3.73 g/dL, alanine transaminase at 8 g/dL, and Aspartate transaminase at 26 g/dL, as shown in Table 1.
| AST | 26 | 0-40 U/L |
| ALT | 8 | 0-41 U/L |
| Albumin | 3.73 | 3.5-5.5 g/dL |
| Urea | 25.2 | 16.6-48.5 mg/dL |
| Creatinine | 0.42 | < 1.2 mg/dL |
| Sodium | 140 | 136-145 mmol/L |
| Potassium | 4.61 | 3.5-5 mmol/L |
| Chloride | 104 | 98-106 mmol/L |
| Calcium | 7.9 | 7.6-11 mg/dL |
| Procalcitonin | 0.26 | < 0.5 ng/mL |
| Blood culture | Sterile | Sterile |
The upper gastrointestinal (GI) endoscopy showed a base of non-epithelial tumor right behind the upper esophageal sphincter (UES). Tumor continues distally throughout the esophagus, freely locating and occupying almost the entire space of esophageal lumen. The neoplasm was a 25 cm in length and 4-5 cm width in the distal part, covered by a normal mucosa of squamous esophageal epithelium. Also, there was significant dilation of the esophagus due to a large size of the tumor, maximum up to 6 cm in middle and lower thirds. The tumor had a complex configuration, the distal part of the tumor splits into two parts and it reaches the stomach cardia. On retroflexion the distal part of non-epithelial neoplasm is visible in the gastric lumen, size of the diaphragmatic crura is up to 5 cm with sliding of cardia and fungus above diaphragm during examination - signs of sliding hiatal cardiofundal hernia (Figure 1A and B).
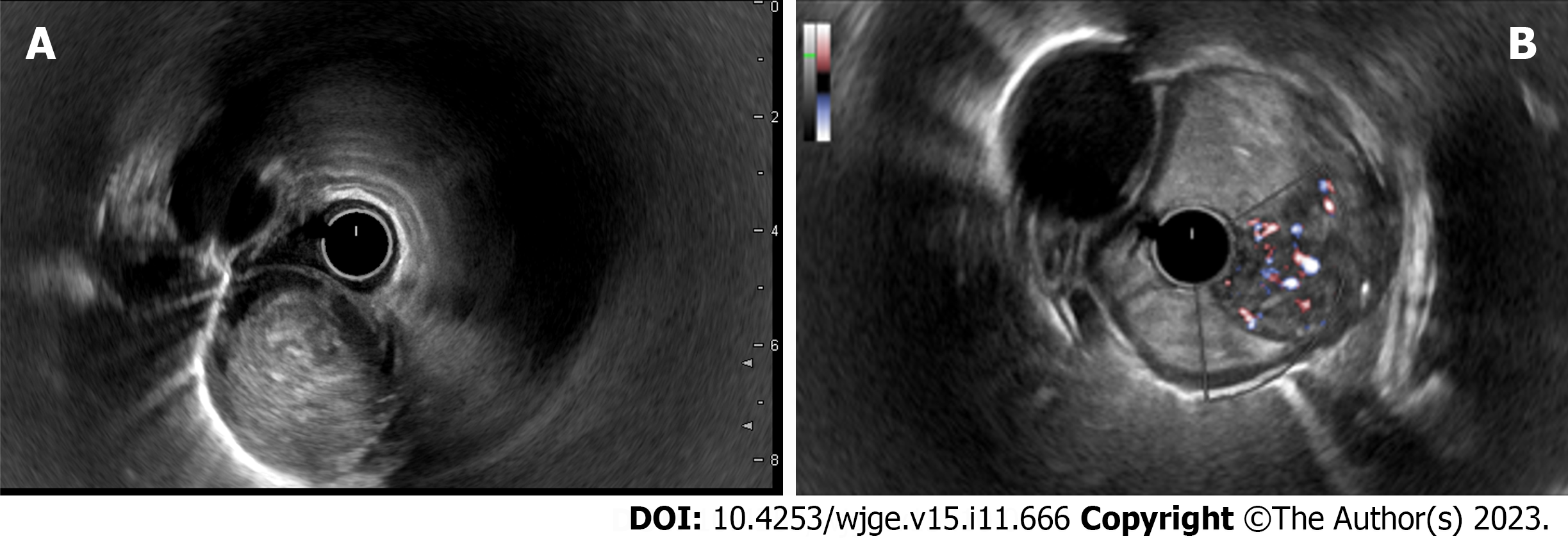
For identification of tumor features, type of growth and localization related to layers of the esophageal walls, an endoscopic ultrasound (EUS) was done. An ultrasound scanning showed heterogeneous hypo-echoic neoplasm with a smooth, clear-contoured, irregular cylindrical shape. The base of the tumor is located right behind the UES and originates from the submucosal layer of the esophagus (3rd echo-layer), type 1 according to the classification of non-epithelial tumors of the gastrointestinal tract[5]. The doppler color mode showed a hypervascular zone at the base of the tumor with multiple large feeding vessels, up to 4-5 mm in diameter, extending along the wall of the esophagus for 8-10 cm. Paragastric lymphatic nodes are not enlarged (Figure 2A and B). EUS imaging, most likely, corresponded to a FVP of the esophagus.
Computed tomography (CT) with intravenous contrast enhancement revealed an expansion of the esophagus up to 5-6 cm in the distal part, a hypervascular neoplasm in the lumen of the esophagus extending throughout the entire length from UES to the gastric cardia with a maximum diameter of up to 6 cm (Figure 3A and B).
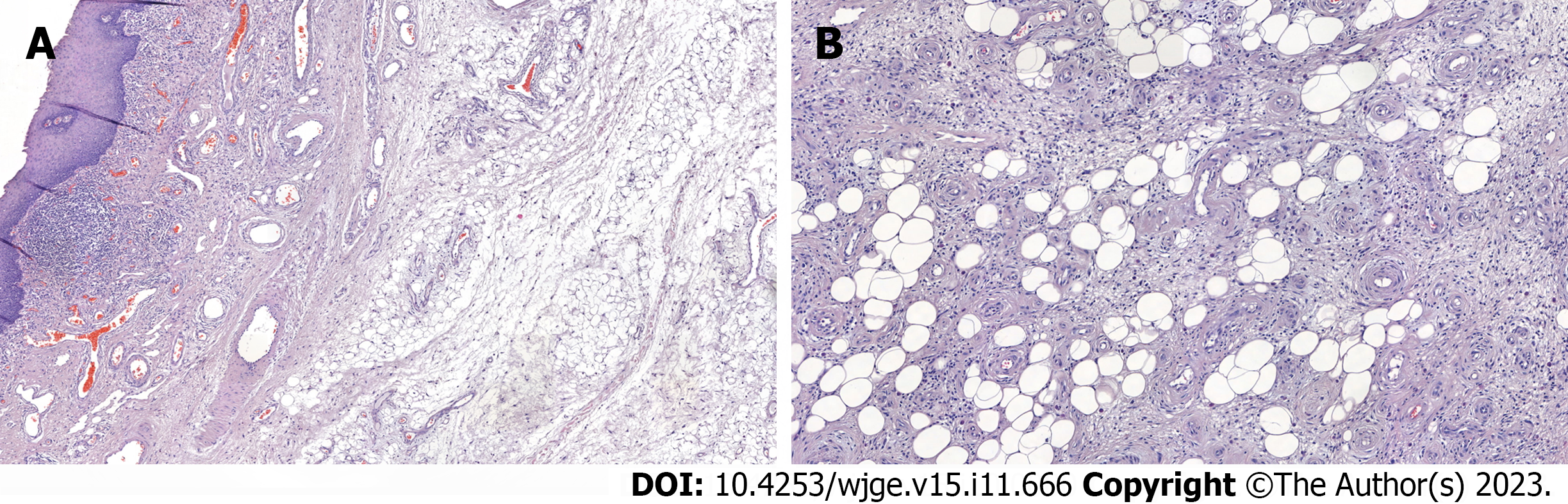
Fibrovascular polyp with foci of highly differentiated liposarcoma, tumor tissue at the sight of endoscopic dissection is not determined, R0, М 8850/3; Grade 1.
Hybrid laparo-endoscopic access - endoscopic submucosal dissection with laparoscopic removal of the tumor.
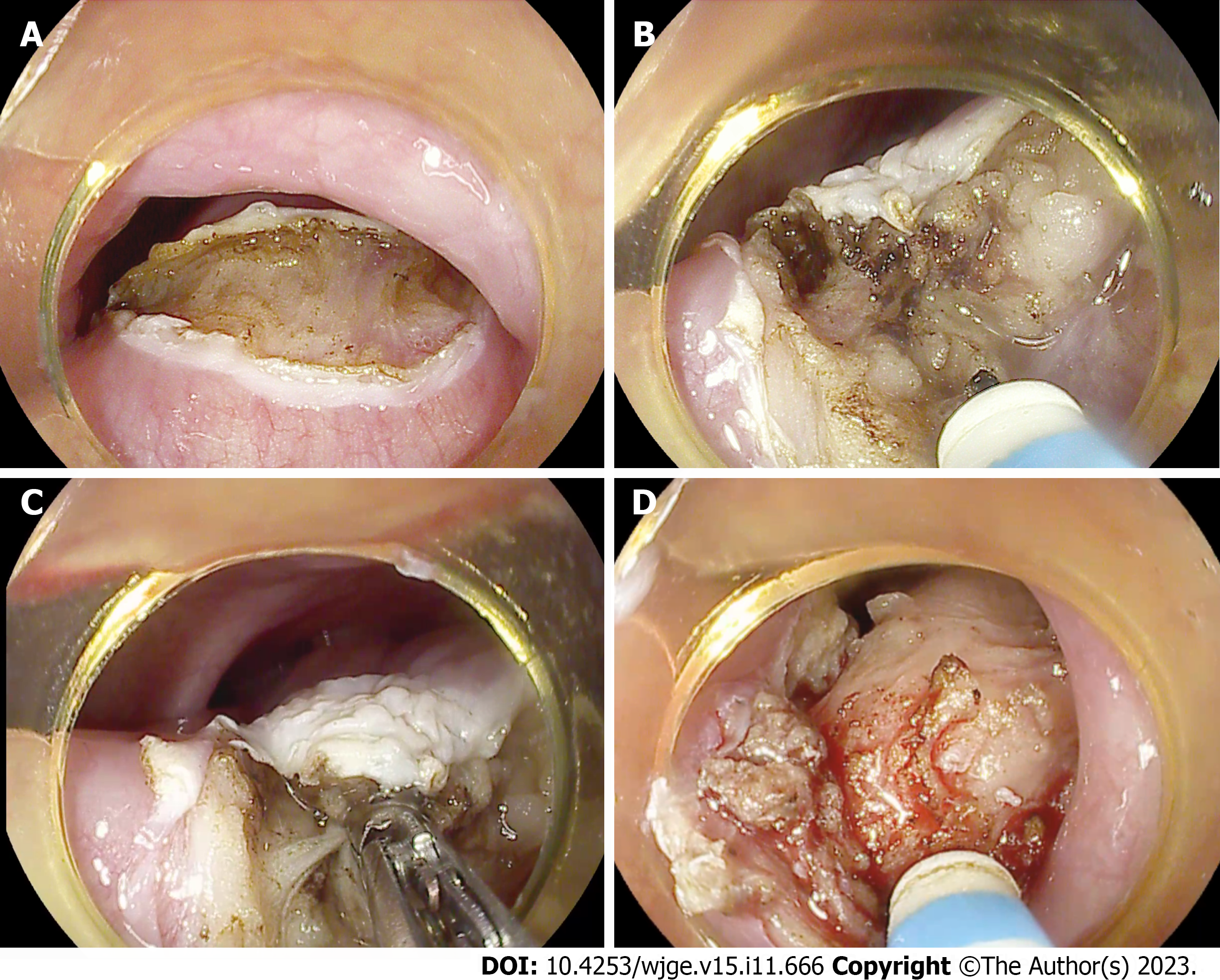
Before to start an endoscopic submucosal dissection (ESD) first step of the procedure was creating a lifting by injection of Gelofusine solution dyed with indigo carmine into submucosal layer. Thereafter, using an endoscopic knife, a dissection of the mucosa and submucosal layer was performed immediately behind UES in horizontal plane (Figure 4А). In order to achieve a stable position of the endoscope in the submucosal layer, a transparent dissection cap was installed on the distal end of the endoscope according to the standard ESD technique. Next, the steps of dissection in the submucosal layer were performed up to 11 cm distally until the tumor was completely cut off at the base. For the dissection of the submucosal layer an endoscopic knife was used. For the coagulation of large feeding vessels in the submucosal layer a coagrasper was used. Using high frequent electro generator, the larger vessels of the submucosal layer were coagulated using <Soft coagulation> mode and the smaller vessels using <Spray coagulation> mode (Figure 4B-D). On the control endoscopic view the area of ESD was 1.5 cm × 2.5 cm × 11 cm in size.
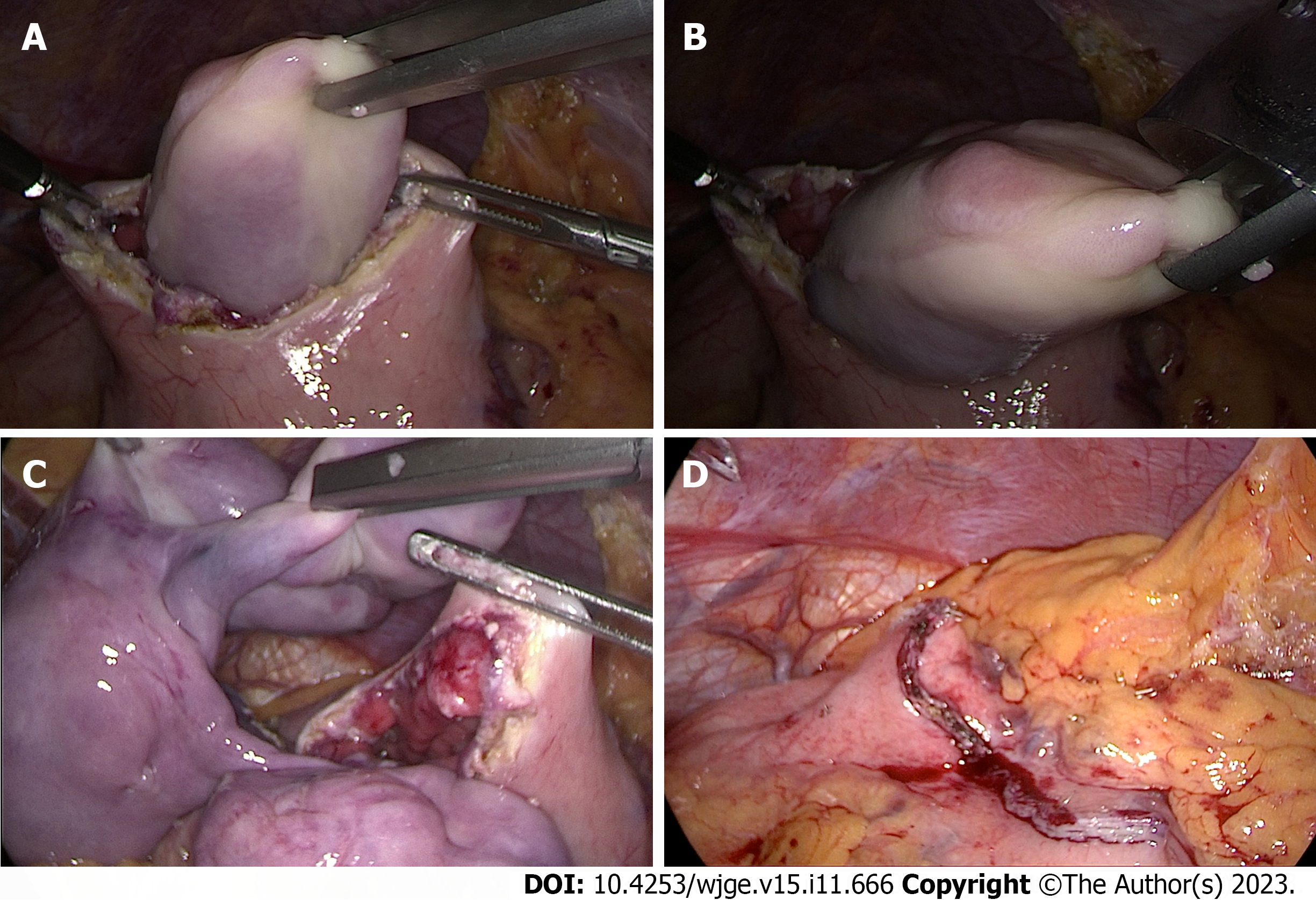
The expected challenges of surgical intervention for esophageal FVP are the technical difficulties of adequate endoscope positioning, instrumental manipulations, and exposure of the surgical field because of anatomically limited space of UES, which corresponds to area of tumor base. One more challenge is the transoral extraction of the tumor with a high risk of stuck of the tumor in a small space of UES and oropharynx due to the large size of the tumor especially in the distal part. That is why we decided to implement an innovative technique - a hybrid laparo-endoscopic approach. After complete excision of the tumor by ESD technique at the base, the neoplasm was brought down into the stomach and removed through a laparoscopic gastrotomy (Figure 5A and B). The detection of the neoplasm did not entail complications, since the patient was also diagnosed with a hernia of the esophageal opening of the diaphragm, characterized by a distance between its size of 5 cm (Figure 5C and D). Next, a standard technique for hiatal hernia repair was performed - diaphragm cruroraphy with Nissen fundoplication (pictures from the operation).
The duration of the operation was 3 h and 50 min. There were no intraoperative and postoperative complications. At the follow-up X-Ray examination done on the 3rd day after surgery, swallowing was not disturbed when taking a contrast, the esophagus was free to pass a contrast agent, no exit of the contrast beyond the walls of the esophagus was registered; no signs of pneumothorax and hydrothorax were revealed. The patient was discharged on the 7th postoperative day. The removed specimen represents a tumor of an irregular elongated shape splitting into two parts at the distal end, 25 cm × 4 cm × 5 cm in size, with a smooth surface covered by intact mucosa (Figure 6). On section, the tumor is represented by vascularized adipose tissue with foci of fibrosis. Morphology study showed fragments of tumor represented by adipose tissue, separated by wide fields of sclerotic fibrous tissue with numerous vessels and cells of the inflammatory infiltrate. Among the fibrous tissue there are unilocular and different-sized adipocytes and hyperchromic cells with angular nuclei (Figure 7A and B). Morphology report: fibrovascular polyp with foci of highly differentiated liposarcoma, tumor tissue at the sight of endoscopic dissection is not determined, R0, М 8850/3; Grade 1 (Figure 7A and B).
The follow-up endoscopic examination 3 mo after surgery showed no residual fragments of the tumor, no narrowing and pathological changes of the mucosa at the area of endoscopic dissection (Figure 8A and B). The fundoplication cuff is well closed, located below the diaphragmatic crura, no gastroesophageal reflux was noted by the patient. The follow-up period up to date is 6 mo. At the moment, the patient has no complaints.
The giant FVP of the esophagus are benign non-epithelial tumors that originate from submucosal layer, covered with normal esophageal mucosa. Usually they appear from the esophagus's upper third at the level of upper esophageal sphincter. Previously the tumor was known as pedunculated lipoma, myxofibroma, and fibroma[6]. FVP are rare tumors, that are composed of around 0.03% esophageal tumors and less than 2% esophageal benign tumors[1,7,8].
There have been fewer than 100 reported cases so far, with most cases occurring in males aged between their late sixties and early nineties[9]. The risk of malignancy is extremely low.
The term ‘fibrovascular polyp’ is collecting the esophageal neoplasms, such as fibroma, fibrolipoma, lipoma, or fibromyxoma, according to World Health Organization classification[10]. Different terms for this type of tumor appeared because the polyps can be composed of various tissues, such blood vessels, muscles, fat, and fibrous tissue.
The etiology of giant fibrovascular polyps is debated. One theory suggests that the lack of muscular support at the pharyngoesophageal junction causes elongation of tissue due to peristalsis traction and swallowing[11]. Another theory, supported by a cytogenetic study, proposes that giant fibrovascular polyps is a neoplastic process with chromosomal changes indicating instability[12]. Retrospective analysis of cases previously labeled as giant fibrovascular polyp of the esophagus lipoma, or liposarcoma revealed murine double minute 2 amplification in all cases, suggesting that most large polypoid fat-containing masses in the esophagus are actually liposarcoma[13].
The size of the tumor can vary from a few centimeters up to large sizes (the widest reported size was 25 cm), which can cause serious complications such as asphyxia as a result of obstruction of the aero-digestive crossroads, dysphagia associated with the tumor’s complete occupation of the lumen of the esophagus. Usually, symptoms are not presented in the early stages due to a small size of the tumor, and the risk of previous complications is mainly presented for tumors above 8 cm[14]. Other clinical symptoms that can alert to this disease are foreign body sensation, coughing, dyspnea, chest discomfort, neck pain, and odynophagia[3].
Diagnosis of fibrovascular polyps is not easy and often requires a combination of patient`s symptoms, history, invasive and non-invasive methods of diagnosis. Among non-invasive methods of diagnosis, barium swallow can show a dilated esophagus and long, smooth filling defects in the lumen of the upper esophagus[14]. However, the sensitivity of this method is not high. CT scans and magnetic resonance imaging are still regarded as the most reliable method to identify the characteristics and origin of a mass. A CT scan of the cervicothoracic region provides important information about a mass, including its characteristics, location in relation to surrounding organs and tissues, and blood supply. This information is crucial in deciding the best approach for clinical treatment[15]. In addition to regular CT scan, positron emission tomography (PET)-CT can also be used to identify, which can help to identify abnormal F-fluoroxy-d-glucose values in various parts of the polyp, which aided in distinguishing between benign and malignant lesions. As a result, PET-CT can be recommended for certain diagnostically challenging cases[15].
Sometimes esophageal polyps are not correctly identified during diagnosis. Around 25% of esophagoscopy may result in misdiagnosis due to the microscopic appear of the polyp[16].
GI endoscopy and EUS play a crucial role in identifying and differentiating between various forms of esophageal fibrovascular polyps. EUS enables real-time ultrasound scanning to gather information about the polyp's origin, echogenicity, and blood supply[17]. Some studies showed that fine Doppler can be unsuccessful in showing vascularization due to the mobile characteristic of fibrovascular polyp. In such cases EUS with contrast enhancement could be helpful. Using EUS with a contrast Sonovue®, tissue microcirculation was highlighted inside the entire head of the polyp, leading to better appreciate the risk of bleeding related to its resection. Sonovue®, as enhancement contrast agent, confirmed its efficacy in identifying microvascularization and improving characterization of a submucosal tumor of the upper digestive tract[6]. On endoscopy, fibrovascular polyps are usually seen as a large intraluminal mass that can be freely moved through the lumen of the esophagus and covered by regular mucosa. However, on occasion, these polyps may go unnoticed if they are covered by normal mucosa or they may be misidentified as cancerous tumors because their pedicles are not easily visible[18].
The accepted approach to address fibrovascular polyps is through surgical excision[19].
This method not only alleviates symptoms but also eliminates the possibility of choking. It can be performed through various approaches, including transoral, transthoracic, transcervical, and endoscopic resection[9,20-24]. Cockbain et al[25] presented a study on the open technique treatment of four patients with epidural field potentials, recommending it for polyps more prominent than 10 cm due to its advantages. However, there were difficulties with polyp removal, but there were no recurrences during long-term follow-up. Quijano et al[26] believe the open technique is best for treating recurrent polyps. The review analyzed 31 patients who underwent transluminal resection, with 15 cases undergoing transoral resection using instruments such as the Weerda laryngoscope and the Weerda diverticuloscope[19]. According to Iván et al[27], transoral resection is a safe approach for giant fibrovascular polyps if specific criteria are met. In one of the reported case series, a combined endoscopic/transoral approach was used to extract the polyp through the oral cavity gradually, and an endo-Gia stapler was used for the stalk section[19].
The neoplasms usually are pedunculated and does not contain deep muscular layers of esophagus which is one of the benefits for minimal invasive surgery[10]. The stag beetle knife can be beneficial in removing large polyps along with their stalks, as it can grab, evaluate, extract, and cauterize specific tissues[28].
Endoscopic resection is a minimally invasive option, but the procedure can be challenging, particularly for larger polyps with a broad pedicle measuring > 8 cm, which may have a higher risk of bleeding. New and more flexible endoscopic guides have made the approach more feasible[29]. The most commonly used technical device is the Endoloop, which is used to trap the polyp stalk and section it with an electrosurgical snare, after which the polyp can be removed by transoral or gastrotomic passway[19]. However, the difficulty of exposing the lesion and the risk of uncontrollable bleeding is higher with endoscopic resection, especially for larger polyps. In choosing the appropriate treatment method, surgeons must consider the size, location, and characteristics polyp's size, as well as the patient's overall health status. If a lesion has only one pedicle, it can be eliminated by endoscopic resection by ligating and electrocoagulating the pedicle[30].
However, endoscopic follow-up examination, typically once every three years, is strongly recommended, as the risk of recurrence is high (up to 50% reported in the literature)[25].
Overall, the treatment and management of fibrovascular polyps require a multidisciplinary approach involving a team of specialists, including gastroenterologists, thoracic surgeons, and endoscopists, to ensure optimal outcomes for the patient.
It is crucial to consider the size and vascularization of fibrovascular polyps when assume endoscopic removal as a treatment option and to carefully plan the surgical technique to avoid difficulties or discomfort during the procedure. However, there is an alternative approach to traditional surgical removal known as the new laparo-endoscopic approach that can be both safe and effective for treating giant fibrovascular polyps in the esophagus.
| 1. | Plachta A. Benign tumors of the esophagus. Review of literature and report of 99 cases. Am J Gastroenterol. 1962;38:639-652. [PubMed] |
| 2. | Khamaysi I, Asbeh YA. Endoscopic resection of giant esophageal fibrovascular polyp. Turk J Gastroenterol. 2020;31:276-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Caceres M, Steeb G, Wilks SM, Garrett HE Jr. Large pedunculated polyps originating in the esophagus and hypopharynx. Ann Thorac Surg. 2006;81:393-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 63] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | I H, Kim JS, Shim YM. Giant fibrovascular polyp of the hypopharynx: surgical treatment with the biappoach. J Korean Med Sci. 2006;21:749-751. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Dzhantukhanova S, Starkov Y, Solodinina E, Zamolodchikov R. The smart approach to surgical treatment of submucosal tumors based on preoperative EUS-typing. Ann Laparosc Endosc Surg. 2019;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Williet N, Kassir R, Casteillo F, Yvorel V, Habougit C, Roblin X, Phelip JM. First Characterization with Ultrasound Contrast Agent of a Fibrovascular Polyp Before Its Endoscopic Resection: A Case Report (with Videos). Clin Endosc. 2019;52:186-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 7. | Jose P, Scott N, Sarela AI. Two-stage removal of giant fibrovascular polyp of the oesophagus. BMJ Case Rep. 2010;2010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Levine MS, Buck JL, Pantongrag-Brown L, Buetow PC, Hallman JR, Sobin LH. Fibrovascular polyps of the esophagus: clinical, radiographic, and pathologic findings in 16 patients. AJR Am J Roentgenol. 1996;166:781-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 73] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Paik HC, Han JW, Jung EK, Bae KM, Lee YH. Fibrovascular polyp of the esophagus in infant. Yonsei Med J. 2001;42:264-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Watanabe H, Jass JR, Sobin LH. Histological typing of oesophageal and gastric tumours, in: Collaboration With Pathologists in 8 Countries (World Health Organization. International Histological Classification of Tumours), 2nd ed., Springer, Berlin, 1998. [DOI] [Full Text] |
| 11. | Pinto A, Abastado B, Cattan P. An esophageal tumor unlike others: The fibrovascular polyp. J Visc Surg. 2019;156:271-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Yu Z, Bane BL, Lee JY, Pitha JV, Peyton M, Houck J, Li S. Cytogenetic and comparative genomic hybridization studies of an esophageal giant fibrovascular polyp: a case report. Hum Pathol. 2012;43:293-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Graham RP, Yasir S, Fritchie KJ, Reid MD, Greipp PT, Folpe AL. Polypoid fibroadipose tumors of the esophagus: 'giant fibrovascular polyp' or liposarcoma? A clinicopathological and molecular cytogenetic study of 13 cases. Mod Pathol. 2018;31:337-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 14. | Blacha MM, Sloots CE, Van Munster IP, Wobbes T. Dysphagia caused by a fibrovascular polyp: a case report. Cases J. 2008;1:334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Wang J, Han DM, Ni X, Ma LJ, Ye JY, Xiao Y. Fibrovascular polyp of the hypopharynx and esophagus. Chin Med J (Engl). 2011;124:3182-3184. [PubMed] |
| 16. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 26126] [Article Influence: 1187.5] [Reference Citation Analysis (2)] |
| 17. | Costa PM, Marques A, Távora, Oliveira E, Diaz M. Inflammatory fibroid polyp of the esophagus. Dis Esophagus. 2000;13:75-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Yannopoulos P, Manes K. Giant fibrovascular polyp of the esophagus - imaging techniques can localize, preoperatively, the origin of the stalk and designate the way of surgical approach: a case report. Cases J. 2009;2:6854. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Ferri V, Vicente E, Quijano Y, Duran H, Diaz E, Fabra I, Malave L, Ruiz P, Isernia R, Caruso R. Giant fibrovascular polyps of the esophagus. Trans oral versus surgical approach. Case report and systematic literature review. Int J Surg Case Rep. 2022;97:107412. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 20. | Chourmouzi D, Drevelegas A. Giant fibrovascular polyp of the oesophagus: a case report and review of the literature. J Med Case Rep. 2008;2:337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Lee SY, Chan WH, Sivanandan R, Lim DT, Wong WK. Recurrent giant fibrovascular polyp of the esophagus. World J Gastroenterol. 2009;15:3697-3700. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 44] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Dutta R, Kumar A, Handa KK, Dinda AK. Large pedunculated fibrovascular polyp of oesophagus in a young woman. Interact Cardiovasc Thorac Surg. 2009;9:352-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Lorenzo D, Gonzalez JM, Barthet M. Endoscopic resection of a giant esophageal fibrovascular polyp. Endoscopy. 2016;48 Suppl 1 UCTN:E69-E70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Murino A, Eisendrath P, Blero D, Ibrahim M, Neuhaus H, Devière J. A giant fibrovascular esophageal polyp endoscopically resected using 2 gastroscopes simultaneously (with videos). Gastrointest Endosc. 2014;79:834-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Cockbain AJ, England R, Dexter SPL, Sarela AI. Surveillance Is Important After Surgical Excision of Giant Fibrovascular Polyps of the Esophagus. Ann Thorac Surg. 2017;104:e341-e343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Quijano Y, Ferri V, Duran H, Diaz E, Fabra I, Malave L, Ruiz P, de Nobili G, Caruso R, Vicente E. Recurrent giant fibrovascualr oesophageal polyp: Benefits and pitfalls of a multimodal approach. Int J Surg Case Rep. 2021;83:105935. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Iván L, Paczona R, Szentpáli K, Jóri J. Peroral endoscopic removal: as a minimally invasive long-term surgical treatment of a regurgitated giant polisegmented fibrovascular polyp of the esophagus. Eur Arch Otorhinolaryngol. 2009;266:1031-1034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 28. | Yamazaki K, Yoshida Y, Maruta A, Shimizu M, Kushima R. Endoscopic resection of a giant fibrovascular esophageal polyp by use of a scissor-type knife. VideoGIE. 2019;4:451-453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Park JS, Bang BW, Shin J, Kwon KS, Kim HG, Shin YW, Choi SJ. A Case of Esophageal Fibrovascular Polyp That Induced Asphyxia during Sleep. Clin Endosc. 2014;47:101-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 30. | Goenka AH, Sharma S, Ramachandran V, Chattopadhyay TK, Ray R. Giant fibrovascular polyp of the esophagus: report of a case. Surg Today. 2011;41:120-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Russia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kanetaka K, Japan; Zhang J, China S-Editor: Liu JH L-Editor: A P-Editor: Cai YX