Published online Jul 16, 2021. doi: 10.4253/wjge.v13.i7.210
Peer-review started: April 29, 2021
First decision: June 17, 2021
Revised: June 22, 2021
Accepted: June 28, 2021
Article in press: June 28, 2021
Published online: July 16, 2021
Processing time: 75 Days and 14.8 Hours
Patients with liver cirrhosis are fragile and present specific clinical hallmarks. When undergoing to gastrointestinal (GI) endoscopy, these subjects require an individual pre evaluation, taking into account: Level of haemostasis impairment, the individual risk of infection, the impact of sedation on hepatic encephalopathy and other factors. The overall assessment of liver function, employing common scoring systems, should be also assessed in the preprocedural phase. Beside some common general problems, regarding GI endoscopy in cirrhotic subjects, also specific issues are present for some frequent indications or procedures. For instance, despite an increased incidence of adenomas in cirrhosis, colon cancer screening remains suboptimal in subjects with this disease. Several studies in fact demonstrated liver cirrhosis as a negative factor for an adequate colon cleansing before colonoscopy. On the other hand, also the routine assessment of gastroesophageal varices during upper GI endoscopy presents some concern, since important inter-observer variability or incomplete description of endoscopic findings has been reported in some studies. In this review we discussed in details the most relevant issues that may be considered while performing general GI endoscopic practice, in patient with cirrhosis. For most of these issues there are no guidelines or clear indications. Moreover until now, few studies focused on these aspects. We believe that targeting these issues with corrective measures may be helpful to develop a tailored endoscopic approach for cirrhosis, in the future.
Core Tip: In this minireview, we discuss some issues that are encountered while performing general gastrointestinal endoscopy in cirrhotic patients. The solution of these aspects may increase, in the future, the yield of this technique in subjects with significant liver disease.
- Citation: Grassi G, Lenci I, Signorello A, Milana M, Baiocchi L. Gastrointestinal endoscopy in cirrhotic patient: Issues on the table. World J Gastrointest Endosc 2021; 13(7): 210-220
- URL: https://www.wjgnet.com/1948-5190/full/v13/i7/210.htm
- DOI: https://dx.doi.org/10.4253/wjge.v13.i7.210
The definition of liver cirrhosis refers to a typical anatomopathological liver change characterized by diffuse fibrosis and regenerative nodules as a result of a chronic immunoinflammatory process[1]. Hepatic architecture distortion gives rise to: (1) A reduced liver blood outflow thus determining portal hypertension and; and (2) An impairment of liver cells activities. These changes may lately determine the typical complications of the disease such as: Ascites, hepatic encephalopathy, hepatorenal syndrome and bleeding after gastroesophageal varices (GEVs) rupture. Therefore, the term cirrhosis does not define a specific clinical condition. In this setting, physicians identify a "compensated" or a "decompensated" form of cirrhosis for medical purposes[2]. In the first case, the cirrhotic patient does not exhibit significant symptoms of the disease, and the diagnosis may be ruled out for tests prescribed for other reasons. In the latter case (decompensated cirrhosis), the subject shows the typical complications of the disease. So, it seems wise before approaching a cirrhotic patient with either diagnostic or therapeutic procedures (including the endoscopic ones) to gain the best information on its function.
In this setting, however, the binary classification into compensated or decom
During their illness, cirrhotic patients may undergo repeated gastrointestinal (GI) endoscopic procedures. For instance, upper GI endoscopy is suggested by United States guidelines as soon as the diagnosis of cirrhosis is achieved, in order to assess for the presence of esophageal varices. In case of absent or small varices, the procedure should be repeated within 2 or 3 years in compensated cirrhosis and yearly in decompensated cirrhosis[6-8].
The British Society of Gastroenterology guidelines recommend screening with slight modification: On an every 3 year basis if no varices were present and annual screening for small varices[6]. Despite the proposal of alternative tests to rule out the presence of varices (such measuring the degree of hepatic stiffness by elastography), the lack of reliability of these techniques still supports the need of upper endoscopy for a definitive diagnosis in the majority of patients[5,9]. Nonetheless, the general use of GI endoscopy has been expanded to also include the cirrhotic population for colon cancer screening, for the advent of ultrasound endoscopy and for the treatment of benign or malignant diseases of the biliary tract. Finally, a specific endoscopy based careful assessment of neoplastic or preneoplastic GI luminal lesions (frequently involving subjects with severe hepatic dysfunction) is required for liver transplant listing.
Given the increased demand of GI endoscopy in cirrhosis and in the attempt to move toward a tailored rather than a general approach in these subjects, in this review, we discuss the possible pitfalls/issues of these procedures in the patient with liver impairment.
Routine sedation, in the course of GI endoscopy, has increased significantly in the last decades, being applied in 60% to 100% of cases, depending on the procedures and practice of the center[10]. Characteristics of most used drugs for sedation in endoscopy are reported in Table 1. Although it is widely considered that any endoscopic examination can be more effectively conducted under sedation[5,11], not all endos
| Drug | Onset of effect (min) | Effect duration (min) | Usual dose | Adverse events |
| Benzodiazepines | ||||
| Midazolam | 1-2 | 15-80 | 1-6 mg | Respiratory depression, disinhibition |
| Flumazenil (Benzodiazepines Antidote) | 1-2 | 60 | 0.1-1 mg | Agitation, withdrawal symptoms |
| Opioids | ||||
| Alfentanyl | < 1 | 30-60 | 0.250-2 mg | Respiratory and cardiovascular depression |
| Fentanyl | 1-2 | 30-60 | 50-200 μg | Respiratory depression, vomiting |
| Pethidine | 3-6 | 60-180 | 25-100 mg | Respiratory depression, vomiting |
| Naloxone (Opioids antidote) | 1-2 | 30-45 | 0.2-1 mg | Narcotic withdrawal |
| Anestethic | ||||
| Propofol | < 1 | 4-8 | 40-400 mg | Respiratory and cardiovascular depression |
In compliance with the American Society of Anesthesiology, sedation should be classified as minimal, moderate or deep, according to a decrease in the consciousness of the patient and depression of effective spontaneous respirations[14]. Minimal and moderate sedation are by far the most adopted solutions in routine GI endoscopy and these are usually achieved by the administration of benzodiazepines (diazepam or midazolam) and/or opioids (meperidine or fentanyl)[15]. Unfortunately, both of these categories of drugs have a delayed metabolism in patients with significant liver impairment, thus possibly exposing them to complications, such as hepatic encephalopathy[16-18]. In this perspective, the use of propofol seems to be superior and safer. A meta-analysis on cirrhotic patients undergoing upper GI endoscopy and comparing midazolam to propofol sedation demonstrated a reduced induction time, shorter time of recovery and most prompt discharge with propofol sedation[19]. The same study reported a worsening of minimal encephalopathy with midazolam, even if a meta-analytic confirmation was not possible, because of the different testing strategies among studies.
Differences between these two drugs may be explained while examining their metabolism. In fact, midazolam is eliminated almost exclusively through the liver, while propofol is eliminated by the kidney after conjugation in hepatic and extra
However, it should be underscored that propofol, differently from benzodiazepines and opioids, does not have a pharmacological antagonist able to counteract possible adverse events. This has given rise the controversial question whether direct administration of propofol by the endoscopist should be considered safe or an anesthesiologist would always be required[25]. On the other hand, despite the fact that adverse events were recorded with similar prevalence employing either propofol or a benzodiazepine plus an opioid, it is questionable that the endoscopist alone can simultaneously induce sedation, supervise the patient and devote himself/herself to the examination.
However, it is evident that this issue remains unsolved and should be approached according to the clinical context, the patient’s condition and possibly on the basis of guidelines produced by the local institution[6,10,17,19,20,23,26].
In many countries, the administration of propofol for sedation, as well as the monitoring during the examination and the evaluation of the restoration to a full state of consciousness, remains to be conducted by a specialist in anesthesiology.
Normal hemostasis implies the coordinate contribution and activation of cells and blood proteins[27]. During liver disease, impairment of this machinery can occur at different times and with different severity. Therefore, any invasive procedure requires a prior evaluation of clotting performance.
Impaired hemostasis in the cirrhotic patient may not be interpreted as the simple deficiency of a coagulation factor. Instead, an imbalance of the entire coagulation cascade (certainly dependent on hepatic pathology), which also involves vascular, renal and medullary dysfunctions, is present[5,16,28]. As a result, cirrhotic patients, besides the increased risk of hemorrhagic complications, may also frequently experience thromboembolic events, since there is a concomitant deficit of anticoagulant factors[29].
In this perspective evaluation of these subjects on the basis of routine tests, such as prothrombin time and international normalized ratio, could be suboptimal[6,30,31], and a hypercoagulable, hypocoagulable or pro-fibrinolytic status should be ruled out just before employing thromboelastography[5,32].
Moreover thrombocytopenia is frequently observed in cirrhosis, further complicating the evaluation of the net clotting performance in the patient with liver disease. Reduced numbers of platelets, in the past, were thought to be mainly dependent to spleen sequestration[33]; however, concurrent bone marrow depression and reduced thrombopoietin production may also have an important role in determining this occurrence[34].
In clinical practice, the treatment of coagulopathy in cirrhotic patients is less standardized in comparison with other subjects[35]. Expert opinions suggest avoiding transfusions of fresh frozen plasma and instead to correct fibrinogen levels in cirrhotic patients undergoing invasive or surgical procedures[36]. Platelet administration is usually considered when the count is < 50 × 109/L. However, one should consider that platelet transfusions are generally afflicted by an increased risk of adverse reactions as compared with the administration of either frozen plasma or red blood cells[37], while platelet refractoriness (lack of increase in platelet count after their administration) is not rare[38]. In this perspective, the new thrombopoietin receptor agonists avatrombopag and lusutrombopag, specifically tested in patients with chronic liver disease undergoing invasive procedures, are of major interest[39,40]. However, despite the good results of these molecules in increasing platelets count, they cannot be considered in urgent situations since they require several days (> 5/8) to achieve a therapeutic effect.
Transmission of infections during GI endoscopy represents an issue that has stimulated the development of specific guidelines for prevention and processing of instruments[41,42]. Despite its rarity, endoscopy-driven infection is also of concern for the possible transmission of antibiotic resistant strains in hospital based units. On the other hand, bacterial infections are responsible for significant morbidity and mortality in cirrhotic patients, also leading to acute-on-chronic liver failure. Moreover, hepatic diseases are known to predispose to infection for several reasons, such as increase intestinal permeability, reduced immunologic defense, portal shunting with peripheral circulation and others[42].
In this perspective, prevention of infections in the cirrhotic patient (also during endoscopy) must always be pursued. While performing endoscopy and with regard to infection prevention, it is necessary to distinguish the compensated cirrhotic patient from the decompensated cirrhotic patient and who is in a state of emergency with bleeding from esophageal or gastric varices.
In the case of a compensated cirrhotic patient undergoing elective endoscopy, no convincing evidence is available on the utility of routine antibiotic prophylaxis, since endoscopy-associated bacteremia does not seem to be relevant[43].
Also, in decompensated cirrhosis with ascites of varying degrees, there is insufficient evidence that colonoscopy can trigger subsequent bacterial peritonitis (frequently these subjects are already under long-term antibiotic prophylaxis), which remains a fairly rare event. Therefore, evacuative paracentesis before endoscopy is also not recommended[5,43].
Conversely, any episode of upper GI bleeding marks a significant event in the patient's medical history. This event can precipitate decompensation, especially in patients with advanced disease or hepatocellular carcinoma. In such situations, bleeding can be fatal in up to 20% of cases[44].
The guidelines strongly recommend, together with prompt endoscopic examina
Screening need in cirrhotic patient: Since the relevant prevalence of colorectal cancer (CRC), accounting for the third most frequent malignant tumor worldwide[45], screening adoption has been suggested by several guidelines[46,47]. Colonoscopy and fecal occult blood immunologic testing are usually regarded as the first-choice strategy[46]. However, the endoscopic colon examination presents several advantages such as: (1) Easy detection of minimal lesions as sessile serrated adenomas; (2) Removal or biopsy of suspected lesions during examination; (3) Is a single-step procedure (achieving the diagnosis without further investigation); and (4) If negative do not require any additional screening assessment within the next 10 years. Patients with liver disease should not be exempt from CRC screening, because they seem to have twice the prevalence for this cancer, in comparison with the general population[48]. On the other hand, liver cirrhosis has long been recognized as an important independent risk factor for colonic adenomas[48], and this finding was recently expanded by the observation that this is also valid for patients with chronic non-cirrhotic liver disease[49]. Given the increased prevalence of preneoplastic colonic lesions and frequent occurrence of chronic low-grade blood loss (because of impaired hemostasis and portal hypertension-related GI abnormalities)[49], the use of fecal occult blood immunologic testing for CRC screening in cirrhotic patients does not seem appropriate compared to that in the general population. Moreover, cirrhotic patients undergoing liver transplantation should be submitted to careful scrutiny and removal of luminal lesions, since immunosuppression may increase the risk of development of CRC after transplant[50]. In this perspective, colonoscopy seems to respond better for the CRC screening needed in patients with significant liver disease. However, the execution of a screening colonoscopy in a cirrhotic patient poses some additional issues in comparison with the general population. Some of these, such as sedation, hemostasis, and infection prevention, were already discussed in the previous paragraphs. Nevertheless, the possible major factor flawing the quality of screening colonoscopy in cirrhosis is represented by bowel cleansing. In fact, among the factors ensuring the good quality of a CRC screening program, adequate bowel cleansing is included, and it should be achieved in at least 90% of subjects[47]. In fact, poor bowel preparation is a well-known predictive factor for missed or delayed cecal intubation and of incomplete colonoscopy[51]. Moreover, it could affect the detection of small preneoplastic luminal lesions, while the detection of a large tumor is usually not impaired[52,53].
Data on bowel cleansing in cirrhotic patient: Optimal colon preparation is a hard task to obtain in patients with severe liver disease. A prospective study examined the predictive factors of inadequate bowel cleansing in 2811 patients undergoing colonoscopy[54]. Liver cirrhosis represented an important contributing factor in the failure to achieve adequate colonic preparation together with body mass index, age and diabetes. In order to further evaluate this issue, our group conducted a prospective observational study comparing normal and cirrhotic patients undergoing screening colonoscopy[55]. Cirrhotic patients completed the prescribed bowel preparation at a similar rate in comparison with the normal control, even if they in general reported a high level of difficulty in assuming the prescribed 4 L standard polyethylene glycol-electrolyte lavage solution. In spite of this, colonic cleansing was inadequate in 49% of cirrhotic patients in comparison with 5% of normal patients (P < 0.001). This statistically impacted the time to reach the cecum and endoscope withdrawal time, while the cecal intubation rate was similar between the two groups. The adenoma detection rate was decreased by liver disease (cirrhosis/normal; 19% vs 27%) but without statistical significance. In another study, differently from our results, a reduced ciecal intubation rate was observed in cirrhosis as a function of ascites volume, but data regarding bowel preparation were not reported in detail[56]. Finally, a further study retrospectively assessed the quality of bowel cleansing between patients with cirrhotic and non-cirrhotic liver disease[57]. This research provided evidence that just cirrhosis and not chronic liver disease was a risk factor for incomplete colonic lavage; however, poor cleansing did not affect the polyp detection rate nor was it a function of severity of cirrhosis as assessed by the MELD score. In conclusion, adequate bowel cleansing seems to be a difficult task to reach in cirrhotic patients. Several gray areas remain to be explored with regard to this issue, such as: (1) The reasons for an impaired lavage in cirrhosis remains unclear; (2) The possibility of improvement with alternative tailored schemes is unexplored; and (3) The net effect of impaired cleansing on diagnostic yield is undefined. Nonetheless, it should be considered wise to specify (also in the informed consent) this with cirrhotic patients, since their colonic cleansing might be suboptimal for an adequate endoscopic diagnosis.
Finally, other groups consider the need for CRC screening marginal in cirrhotic patients or at least in those undergoing liver transplantation. In fact, a study on 808 cirrhotic patients undergoing CRC screening before liver transplant showed a limited diagnostic yield (0.2% of CRC and 5.4% of significant adenomas), but at the same time, an increased risk of significant complications (kidney dysfunction and GI bleeding) in the 30 d following endoscopy was recorded[58].
Perhaps the most frequent reason for endoscopic examination in cirrhotic patients is evaluation and monitoring of endoscopic signs of portal hypertension. GEVs are present in a large portion of cirrhotic patients (60%-85%) and may cause significant bleeding and death[59,60]. While some noninvasive tests may rule out the presence of GEVs in well-selected patients, upper GI endoscopy remains the gold standard to accurately define the extent of individual risk, to attain surveillance and to manage acute bleeding[61]. Adequate assessment of GEVs is of crucial importance to prevent variceal rupture and hemorrhage. Bleeding prevention may be obtained by endoscopic band ligation, use of beta blockers or TIPS placement. These measures are usually adopted in subjects exhibiting large varices with red signs (primary prophylaxis) or in those with a previous bleeding episode (secondary prophylaxis). While the GEV bleeding-related deaths remain significant, accounting for 15%-20% of cases[62,63], endoscopy practice in the real world presents some weaknesses. First of all, while some guidelines suggest valid strategies and timing to assess GEVs[7,64], these indications are frequently neglected. A survey in the United States was conducted in order to assess clinical practice in the screening for GEVs[65].
A questionnaire was administered to hepatologists and gastroenterologists throughout the country. Only 60% of the interviewed physicians prescribed upper GI endoscopy at the first diagnosis of cirrhosis. The surveillance timing, as suggested by guidelines, was fulfilled in less than 50% of cases. A cohort study, in the same country, reported an even worse picture[66]. Among 4230 hepatitis C virus cirrhotic patients, just 54% underwent an upper GI endoscopy in a 6-year follow-up, and the examination was performed within 1 year of the diagnosis in only 33.8% of patients. The reasons for this suboptimal standard of care in GEV assessment are not clear. Multiple factors may contribute to this picture, such as: (1) Limited knowledge of GEV management; (2) Overestimation of clinical parameters for predicting portal hypertension; and (3) Racial disparities for management of cirrhosis in some countries[67]. Of concern, even after GEV bleeding, the subsequent surveillance and treatment is seldom observed. In a study among 99 subjects undergoing endoscopic band ligation for acute variceal bleeding, just one-third of subjects followed an endoscopic GEV eradication protocol and 46% did not have any further endoscopic examination after hospital discharge[68]. Beside the scarce adherence to GEV endoscopic diagnosis and surveillance, another factor that may impair the appropriate clinical management of portal hypertension in cirrhosis is the lack of an adequate and unequivocal description of endoscopic findings. More than three decades ago, an Italian study assessed the reliability of upper GI endoscopic examination in cirrhotic patients, comparing the reports of six experts on the same patients[69].The agreement between endoscopists was fair, in the majority of cases, and poor with regard to some variceal features (blue color and extension of red color sign). Excellent agreement (k index > 75) was not recorded for any of the GEV endoscopic features examined. This study underscored, for the first time in the era of flexible endoscopy, the possible operator-dependent limits in the endoscopic assessment of GEV. More recently, our group evaluated the diagnostic accuracy of upper GI endoscopy in cirrhotic patients during common clinical practice[70]. Endoscopic reports (n = 120), coming from different institutions within our regional area, were retrieved and evaluated by eight independent experts (four endoscopists and four hepatologists). While endoscopists evaluated 41% of the reports as incomplete, the hepatologists considered more than one-third of the examinations (36%) inadequate to make decisions on patient management.
Examining all of the above mentioned studies, it comes clear as upper GI endoscopy is not so frequently or adequately performed as usually required in liver cirrhosis. Possible corrective measures may include: (1) Enhanced diffusion of practice guidelines; (2) Identification of a simplified univocal system for GEV endoscopy reports; and (3) Referral of cirrhotic patients to a dedicated GI endoscopic service. In the meantime, the suboptimal endoscopic approach to GEV likely contributes to the significant bleeding-related mortality in cirrhotic patients.
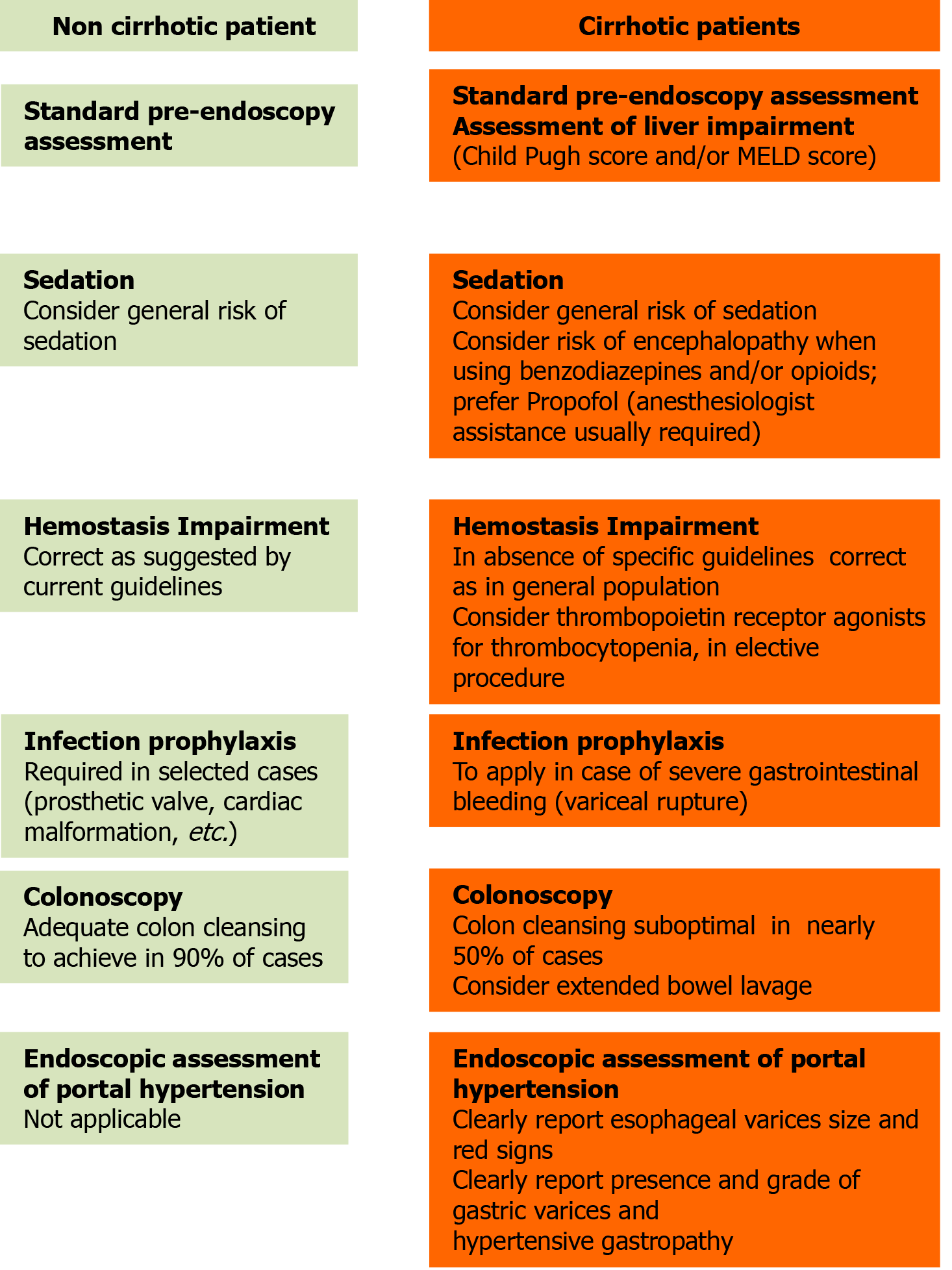
Flexible GI endoscopy has undergone exceptional development and diffusion in the last 70 years[71]. Wide application of endoscopic examination has revealed some definite patient-related issues. Specific guidelines have been produced, for instance, with regard to inflammatory bowel disease[72], for patients on anticoagulant or antiplatelet agents[73] or for bowel cleansing in subjects with chronic kidney disease[74]. These indications were generated in the attempt to move toward the concept of a patient-tailored endoscopy. Several endoscopic guidelines have also been produced for cirrhotic patients, but they mainly focus on prevention and treatment of GEV bleeding, as well as the important associated mortality[7,61,64]. However, other clinical issues may be encountered while approaching a cirrhotic subject with GI endoscopy, and in this review, we attempted to focus on the main ones. In Figure 1 are summarized some tips to consider while approaching the cirrhotic patient with GI endoscopy. As we reported earlier, for the larger part of these, there are no guidelines or even clear indications. Besides, just a marginal part of published literature specifically examined these problems in liver disease patients. In this uncertainty, our manuscript seems novel since it focused on some overlooked aspects of endoscopy in cirrhotic patients, stimulating further research on these issues. On the other hand we attempted to give some practical (even if not conclusive) tips for the everyday clinical activity. Finally, we claim that further studies and collaborative work within experts should be pursued to design cirrhosis-tailored endoscopic behaviors in order to improve routine practice, diagnostic yield, safety and procedure outcomes in these subjects.
| 1. | Schuppan D, Afdhal NH. Liver cirrhosis. Lancet. 2008;371:838-851. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1686] [Cited by in RCA: 1608] [Article Influence: 89.3] [Reference Citation Analysis (0)] |
| 2. | Mansour D, McPherson S. Management of decompensated cirrhosis. Clin Med (Lond). 2018;18:s60-s65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 71] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 3. | Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5490] [Cited by in RCA: 5826] [Article Influence: 109.9] [Reference Citation Analysis (2)] |
| 4. | Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31:864-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1967] [Cited by in RCA: 2107] [Article Influence: 81.0] [Reference Citation Analysis (0)] |
| 5. | Horsley-Silva JL, Vargas HE. Gastrointestinal endoscopy in the cirrhotic patient. Expert Rev Gastroenterol Hepatol. 2015;9:1005-1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Krystallis C, Masterton GS, Hayes PC, Plevris JN. Update of endoscopy in liver disease: more than just treating varices. World J Gastroenterol. 2012;18:401-411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 7. | Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W; Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46:922-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1229] [Cited by in RCA: 1221] [Article Influence: 64.3] [Reference Citation Analysis (2)] |
| 8. | Qureshi W, Adler DG, Davila R, Egan J, Hirota W, Leighton J, Rajan E, Zuckerman MJ, Fanelli R, Wheeler-Harbaugh J, Baron TH, Faigel DO; Standards of Practice Committee. ASGE Guideline: the role of endoscopy in the management of variceal hemorrhage, updated July 2005. Gastrointest Endosc. 2005;62:651-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 90] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 9. | Abraldes JG, Araujo IK, Turón F, Berzigotti A. Diagnosing and monitoring cirrhosis: Liver biopsy, hepatic venous pressure gradient and elastography. Gastroenterol Hepatol. 2012;35:488-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Triantafillidis JK, Merikas E, Nikolakis D, Papalois AE. Sedation in gastrointestinal endoscopy: current issues. World J Gastroenterol. 2013;19:463-481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 172] [Cited by in RCA: 176] [Article Influence: 13.5] [Reference Citation Analysis (3)] |
| 11. | Ferreira AO, Cravo M. Sedation in gastrointestinal endoscopy: Where are we at in 2014? World J Gastrointest Endosc. 2015;7:102-109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 31] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Amornyotin S. Sedation-related complications in gastrointestinal endoscopy. World J Gastrointest Endosc. 2013;5:527-533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 77] [Cited by in RCA: 108] [Article Influence: 8.3] [Reference Citation Analysis (4)] |
| 13. | Vargo JJ 2nd. Sedation-related complications in gastrointestinal endoscopy. Gastrointest Endosc Clin N Am. 2015;25:147-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Das S, Ghosh S. Monitored anesthesia care: An overview. J Anaesthesiol Clin Pharmacol. 2015;31:27-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | ASGE Standards of Practice Committee; Early DS, Lightdale JR, Vargo JJ 2nd, Acosta RD, Chandrasekhara V, Chathadi KV, Evans JA, Fisher DA, Fonkalsrud L, Hwang JH, Khashab MA, Muthusamy VR, Pasha SF, Saltzman JR, Shergill AK, Cash BD, DeWitt JM. Guidelines for sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2018;87:327-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 402] [Article Influence: 50.3] [Reference Citation Analysis (0)] |
| 16. | Assy N, Rosser BG, Grahame GR, Minuk GY. Risk of sedation for upper GI endoscopy exacerbating subclinical hepatic encephalopathy in patients with cirrhosis. Gastrointest Endosc. 1999;49:690-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 57] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Khamaysi I, William N, Olga A, Alex I, Vladimir M, Kamal D, Nimer A. Sub-clinical hepatic encephalopathy in cirrhotic patients is not aggravated by sedation with propofol compared to midazolam: a randomized controlled study. J Hepatol. 2011;54:72-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 18. | Weston BR, Chadalawada V, Chalasani N, Kwo P, Overley CA, Symms M, Strahl E, Rex DK. Nurse-administered propofol vs midazolam and meperidine for upper endoscopy in cirrhotic patients. Am J Gastroenterol. 2003;98:2440-2447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 67] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | Tsai HC, Lin YC, Ko CL, Lou HY, Chen TL, Tam KW, Chen CY. Propofol vs midazolam for upper gastrointestinal endoscopy in cirrhotic patients: a meta-analysis of randomized controlled trials. PLoS One. 2015;10:e0117585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 20. | Bamji N, Cohen LB. Endoscopic sedation of patients with chronic liver disease. Clin Liver Dis. 2010;14:185-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Riphaus A, Lechowicz I, Frenz MB, Wehrmann T. Propofol sedation for upper gastrointestinal endoscopy in patients with liver cirrhosis as an alternative to midazolam to avoid acute deterioration of minimal encephalopathy: a randomized, controlled study. Scand J Gastroenterol. 2009;44:1244-1251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Fagà E, De Cento M, Giordanino C, Barletti C, Bruno M, Carucci P, De Angelis C, Venon WD, Musso A, Reggio D, Fagoonee S, Pellicano R, Ceretto S, Ciccone G, Rizzetto M, Saracco G. Safety of propofol in cirrhotic patients undergoing colonoscopy and endoscopic retrograde cholangiography: results of a prospective controlled study. Eur J Gastroenterol Hepatol. 2012;24:70-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Tanaka N, Horiuchi A, Nakayama Y, Katsuyama Y, Isobe M, Aoyama T, Tanaka E, Ohmori S. Safety and effectiveness of low-dose propofol sedation during and after esophagogastroduodenoscopy in child A and B cirrhotic patients. Dig Dis Sci. 2013;58:1383-1389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Correia LM, Bonilha DQ, Gomes GF, Brito JR, Nakao FS, Lenz L, Rohr MR, Ferrari AP, Libera ED. Sedation during upper GI endoscopy in cirrhotic outpatients: a randomized, controlled trial comparing propofol and fentanyl with midazolam and fentanyl. Gastrointest Endosc 2011; 73: 45-51, 51. e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 49] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 25. | Dumonceau JM. Non-anesthesiologist-administered propofol: where do we stand? Endosc Int Open. 2019;7:E630-E632. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | McGuire BM. Safety of endoscopy in patients with end-stage liver disease. Gastrointest Endosc Clin N Am. 2001;11:111-130. [PubMed] |
| 27. | Mackie IJ, Bull HA. Normal haemostasis and its regulation. Blood Rev. 1989;3:237-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Tripodi A, Primignani M, Chantarangkul V, Mannucci PM. Pro-coagulant imbalance in patients with chronic liver disease. J Hepatol. 2010;53:586-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Tripodi A. Hemostasis abnormalities in cirrhosis. Curr Opin Hematol. 2015;22:406-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 58] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 30. | Lisman T, Caldwell SH, Burroughs AK, Northup PG, Senzolo M, Stravitz RT, Tripodi A, Trotter JF, Valla DC, Porte RJ; Coagulation in Liver Disease Study Group. Hemostasis and thrombosis in patients with liver disease: the ups and downs. J Hepatol. 2010;53:362-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 239] [Article Influence: 14.9] [Reference Citation Analysis (1)] |
| 31. | García-Pagán JC, Reverter E, Abraldes JG, Bosch J. Acute variceal bleeding. Semin Respir Crit Care Med. 2012;33:46-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 32. | Violi F, Basili S, Raparelli V, Chowdary P, Gatt A, Burroughs AK. Patients with liver cirrhosis suffer from primary haemostatic defects? J Hepatol. 2011;55:1415-1427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 125] [Article Influence: 8.3] [Reference Citation Analysis (1)] |
| 33. | Aster RH. Pooling of platelets in the spleen: role in the pathogenesis of "hypersplenic" thrombocytopenia. J Clin Invest. 1966;45:645-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 581] [Cited by in RCA: 561] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 34. | Peck-Radosavljevic M. Thrombocytopenia in chronic liver disease. Liver Int. 2017;37:778-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 199] [Article Influence: 22.1] [Reference Citation Analysis (1)] |
| 35. | Bull-Henry K. Endoscopy in the coagulopathic patient. Curr Opin Gastroenterol. 2019;35:401-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 36. | Tripodi A, Primignani M, Mannucci PM, Caldwell SH. Changing Concepts of Cirrhotic Coagulopathy. Am J Gastroenterol. 2017;112:274-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 145] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 37. | Kiefel V. Reactions Induced by Platelet Transfusions. Transfus Med Hemother. 2008;35:354-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 82] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 38. | Stanworth SJ, Navarrete C, Estcourt L, Marsh J. Platelet refractoriness--practical approaches and ongoing dilemmas in patient management. Br J Haematol. 2015;171:297-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 173] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 39. | Terrault N, Chen YC, Izumi N, Kayali Z, Mitrut P, Tak WY, Allen LF, Hassanein T. Avatrombopag Before Procedures Reduces Need for Platelet Transfusion in Patients With Chronic Liver Disease and Thrombocytopenia. Gastroenterology. 2018;155:705-718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 185] [Article Influence: 23.1] [Reference Citation Analysis (1)] |
| 40. | Peck-Radosavljevic M, Simon K, Iacobellis A, Hassanein T, Kayali Z, Tran A, Makara M, Ben Ari Z, Braun M, Mitrut P, Yang SS, Akdogan M, Pirisi M, Duggal A, Ochiai T, Motomiya T, Kano T, Nagata T, Afdhal N. Lusutrombopag for the Treatment of Thrombocytopenia in Patients With Chronic Liver Disease Undergoing Invasive Procedures (L-PLUS 2). Hepatology. 2019;70:1336-1348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 121] [Article Influence: 17.3] [Reference Citation Analysis (1)] |
| 41. | ASGE Quality Assurance in Endoscopy Committee; Calderwood AH, Day LW, Muthusamy VR, Collins J, Hambrick RD 3rd, Brock AS, Guda NM, Buscaglia JM, Petersen BT, Buttar NS, Khanna LG, Kushnir VM, Repaka A, Villa NA, Eisen GM. ASGE guideline for infection control during GI endoscopy. Gastrointest Endosc. 2018;87:1167-1179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 143] [Article Influence: 17.9] [Reference Citation Analysis (1)] |
| 42. | Reprocessing Guideline Task Force, Petersen BT, Cohen J, Hambrick RD 3rd, Buttar N, Greenwald DA, Buscaglia JM, Collins J, Eisen G. Multisociety guideline on reprocessing flexible GI endoscopes: 2016 update. Gastrointest Endosc 2017; 85: 282-294. e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 137] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 43. | Llach J, Elizalde JI, Bordas JM, Gines A, Almela M, Sans M, Mondelo F, Pique JM. Prospective assessment of the risk of bacteremia in cirrhotic patients undergoing lower intestinal endoscopy. Gastrointest Endosc. 1999;49:214-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 44. | de Franchis R; Baveno V Faculty. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2010;53:762-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1066] [Cited by in RCA: 1047] [Article Influence: 65.4] [Reference Citation Analysis (0)] |
| 45. | Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66:683-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3058] [Cited by in RCA: 3519] [Article Influence: 391.0] [Reference Citation Analysis (4)] |
| 46. | Shaukat A, Kahi CJ, Burke CA, Rabeneck L, Sauer BG, Rex DK. ACG Clinical Guidelines: Colorectal Cancer Screening 2021. Am J Gastroenterol. 2021;116:458-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 539] [Article Influence: 107.8] [Reference Citation Analysis (0)] |
| 47. | Rembacken B, Hassan C, Riemann JF, Chilton A, Rutter M, Dumonceau JM, Omar M, Ponchon T. Quality in screening colonoscopy: position statement of the European Society of Gastrointestinal Endoscopy (ESGE). Endoscopy. 2012;44:957-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 233] [Article Influence: 16.6] [Reference Citation Analysis (1)] |
| 48. | Komaki Y, Komaki F, Micic D, Ido A, Sakuraba A. Risk of colorectal cancer in chronic liver diseases: a systematic review and meta-analysis. Gastrointest Endosc 2017; 86: 93-104. e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 49. | Troschel AS, Miks A, Troschel FM, Hüsing-Kabar A, Maschmeier M, Heinzow HS, Schmidt HH, Kabar I. Chronic liver disease promotes lesions of the colorectal adenoma-carcinoma sequence, independent of liver cirrhosis. United European Gastroenterol J. 2019;7:662-672. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 50. | Haagsma EB, Hagens VE, Schaapveld M, van den Berg AP, de Vries EG, Klompmaker IJ, Slooff MJ, Jansen PL. Increased cancer risk after liver transplantation: a population-based study. J Hepatol. 2001;34:84-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 250] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 51. | Jang JY, Chun HJ. Bowel preparations as quality indicators for colonoscopy. World J Gastroenterol. 2014;20:2746-2750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (2)] |
| 52. | Harewood GC, Sharma VK, de Garmo P. Impact of colonoscopy preparation quality on detection of suspected colonic neoplasia. Gastrointest Endosc. 2003;58:76-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 524] [Cited by in RCA: 566] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 53. | Froehlich F, Wietlisbach V, Gonvers JJ, Burnand B, Vader JP. Impact of colonic cleansing on quality and diagnostic yield of colonoscopy: the European Panel of Appropriateness of Gastrointestinal Endoscopy European multicenter study. Gastrointest Endosc. 2005;61:378-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 642] [Cited by in RCA: 707] [Article Influence: 33.7] [Reference Citation Analysis (2)] |
| 54. | Hassan C, Fuccio L, Bruno M, Pagano N, Spada C, Carrara S, Giordanino C, Rondonotti E, Curcio G, Dulbecco P, Fabbri C, Della Casa D, Maiero S, Simone A, Iacopini F, Feliciangeli G, Manes G, Rinaldi A, Zullo A, Rogai F, Repici A. A predictive model identifies patients most likely to have inadequate bowel preparation for colonoscopy. Clin Gastroenterol Hepatol. 2012;10:501-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 216] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 55. | Salso A, De Leonardis F, Lionetti R, Lenci I, Angelico M, Telese A, Baiocchi L. Standard bowel cleansing is highly ineffective in cirrhotic patients undergoing screening colonoscopy. Dig Liver Dis. 2015;47:523-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 56. | Macken EJ, Steinhauser A, De Schepper HU, De Winter BY, Moreels TG. Colonoscopy in patients with liver cirrhosis : success and safety issues. Acta Gastroenterol Belg. 2015;78:411-414. [PubMed] |
| 57. | Anam AK, Karia K, Jesudian AB, Bosworth BP. Cirrhotic Patients Have Worse Bowel Preparation at Screening Colonoscopy than Chronic Liver Disease Patients without Cirrhosis. J Clin Exp Hepatol. 2016;6:297-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 58. | Oey RC, van Tilburg L, Erler NS, Metselaar HJ, Spaander MCW, van Buuren HR, de Man RA. The Yield and Safety of Screening Colonoscopy in Patients Evaluated for Liver Transplantation. Hepatology. 2019;69:2598-2607. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 59. | Jakab SS, Garcia-Tsao G. Evaluation and Management of Esophageal and Gastric Varices in Patients with Cirrhosis. Clin Liver Dis. 2020;24:335-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 75] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 60. | Jakab SS, Garcia-Tsao G. Screening and Surveillance of Varices in Patients With Cirrhosis. Clin Gastroenterol Hepatol. 2019;17:26-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (1)] |
| 61. | de Franchis R; Baveno VI Faculty. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63:743-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2609] [Cited by in RCA: 2359] [Article Influence: 214.5] [Reference Citation Analysis (4)] |
| 62. | Reverter E, Tandon P, Augustin S, Turon F, Casu S, Bastiampillai R, Keough A, Llop E, González A, Seijo S, Berzigotti A, Ma M, Genescà J, Bosch J, García-Pagán JC, Abraldes JG. A MELD-based model to determine risk of mortality among patients with acute variceal bleeding. Gastroenterology 2014; 146: 412-19. e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 290] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 63. | Amitrano L, Guardascione MA, Manguso F, Bennato R, Bove A, DeNucci C, Lombardi G, Martino R, Menchise A, Orsini L, Picascia S, Riccio E. The effectiveness of current acute variceal bleed treatments in unselected cirrhotic patients: refining short-term prognosis and risk factors. Am J Gastroenterol. 2012;107:1872-1878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 139] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 64. | Tripathi D, Stanley AJ, Hayes PC, Patch D, Millson C, Mehrzad H, Austin A, Ferguson JW, Olliff SP, Hudson M, Christie JM; Clinical Services and Standards Committee of the British Society of Gastroenterology. U.K. guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut. 2015;64:1680-1704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 454] [Cited by in RCA: 428] [Article Influence: 38.9] [Reference Citation Analysis (2)] |
| 65. | Barritt AS 4th, Arguedas MR. Practice patterns in screening for varices: an American survey. Dig Liver Dis. 2009;41:676-682. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 66. | Flemming JA, Saxena V, Shen H, Terrault NA, Rongey C. Facility- and Patient-Level Factors Associated with Esophageal Variceal Screening in the USA. Dig Dis Sci. 2016;61:62-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 67. | Spiewak T, Taefi A, Patel S, Li CS, Chak E. Racial disparities of Black Americans hospitalized for decompensated liver cirrhosis. BMC Gastroenterol. 2020;20:245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 68. | Everett BT, Lidofsky SD. Adherence to surveillance endoscopy following hospitalization for index esophageal variceal hemorrhage. World J Gastrointest Surg. 2018;10:40-48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 69. | Reliability of endoscopy in the assessment of variceal features. The Italian Liver Cirrhosis Project. J Hepatol. 1987;4:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 67] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 70. | Cucchiarelli S, Santopaolo F, Lamazza A, Lionetti R, Lenci I, Manzia TM, Angelico M, Milana M, Baiocchi L. Pitfalls in the reporting of upper endoscopy features in cirrhotic patients. Dig Liver Dis. 2019;51:382-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 71. | Sivak MV. Gastrointestinal endoscopy: past and future. Gut. 2006;55:1061-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 62] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 72. | Leighton JA, Shen B, Baron TH, Adler DG, Davila R, Egan JV, Faigel DO, Gan SI, Hirota WK, Lichtenstein D, Qureshi WA, Rajan E, Zuckerman MJ, VanGuilder T, Fanelli RD; Standards of Practice Committee; American Society for Gastrointestinal Endoscopy. ASGE guideline: endoscopy in the diagnosis and treatment of inflammatory bowel disease. Gastrointest Endosc. 2006;63:558-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 163] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 73. | Veitch AM, Vanbiervliet G, Gershlick AH, Boustiere C, Baglin TP, Smith LA, Radaelli F, Knight E, Gralnek IM, Hassan C, Dumonceau JM. Endoscopy in patients on antiplatelet or anticoagulant therapy, including direct oral anticoagulants: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guidelines. Gut. 2016;65:374-389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 176] [Cited by in RCA: 188] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 74. | Connor A, Tolan D, Hughes S, Carr N, Tomson C. Consensus guidelines for the safe prescription and administration of oral bowel-cleansing agents. Gut. 2012;61:1525-1532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Amornyotin S, Sira AM S-Editor: Fan JR L-Editor: A P-Editor: Wang LL