Published online Mar 16, 2021. doi: 10.4253/wjge.v13.i3.82
Peer-review started: December 3, 2020
First decision: December 31, 2020
Revised: December 31, 2020
Accepted: February 12, 2021
Article in press: February 12, 2021
Published online: March 16, 2021
Processing time: 95 Days and 21 Hours
Post-colonoscopy diverticulitis is increasingly recognized as a potential complication. However, the evidence is sparse in the literature.
To systematically review all available evidence to describe the incidence, clinical course with management and propose a definition.
The databases PubMed, EMBASE and Cochrane databases were searched using with the keywords up to June 2020. Additional manual search was performed and cross-checked for additional references. Data collected included demographics, reason for colonoscopy, time to diagnosis, method of diagnosis (clinical vs imaging) and management outcomes.
A total of nine studies were included in the final systematic review with a total of 339 cases. The time to diagnosis post-colonoscopy ranged from 2 h to 30 d. Clinical presentation for these patients were non-specific including abdominal pain, nausea/vomiting, per rectal bleeding and chills/fever. Majority of the cases were diagnosed based on computed tomography scan. The management for these patients were similar to the usual patients presenting with diverticulitis where most resolve with non-operative intervention (i.e., antibiotics and bowel rest).
The entity of post-colonoscopy diverticulitis remains contentious where there is a wide duration post-procedure included. Regardless of whether this is a true complication post-colonoscopy or a de novo event, early diagnosis is vital to guide appropriate treatment. Further prospective studies especially registries should include this as a complication to try to capture the true incidence.
Core Tip: The entity of post-colonoscopy diverticulitis is a rare complication. However, there is no consensus on its definition especially on the duration included post-procedure. It could well represent a de novo event or exacerbation of subacute condition. Regardless, it should be considered as a differential in patients presenting with abdominal pain post-colonoscopy and managed according to the usual treatment of patients presenting with diverticulitis.
- Citation: Ng ZQ, Tan JH, Tan HCL, Theophilus M. Post-colonoscopy diverticulitis: A systematic review. World J Gastrointest Endosc 2021; 13(3): 82-89
- URL: https://www.wjgnet.com/1948-5190/full/v13/i3/82.htm
- DOI: https://dx.doi.org/10.4253/wjge.v13.i3.82
Colonoscopy is usually performed for the purpose of screening, diagnostic or surveillance. It is a relatively safe procedure with complication rate between 0.1%-0.3%[1,2]. Most large studies report mainly on complications such as bleeding, perforation and post-polypectomy syndrome[1,2]. Other rarer complications such as splenic injury and pancreatitis have also been reported[2,3]. In recent years, the entity of post-colonoscopy diverticulitis has emerged as a potential complication. Its exact incidence is not known but estimated to be around 0.04%-0.08%[1]. The underlying pathogenesis is not known as a few theories have been hypothesized.
This entity is likely to be progressively more significant due to the exponential increase in number of colonoscopies performed worldwide from colorectal screening programmes and the improved life expectancy of the global population which coincides with higher incidence of diverticular disease[4]. This is evident in the study from Guertin et al[5] where there were 4066 more screening and surveillance colonoscopies in the last 2 years of the study period as compared with the first 2 years (13841 in 2015-2016 vs 9755 in 2013-2014, P = 0.005).
With no uniform and clear definition of this entity, the aim of this study was to systematically review all available evidence of post-colonoscopy diverticulitis and described its incidence, clinical course and to propose a definition.
A systematic review of the literature from the January 1990 to June 2020 was performed by searching PubMed, EMBASE and Cochrane databases. The medical subject headings (MeSH) and keywords used individually or in combination were: “diverticulitis”, “colonoscopy”, “post-colonoscopy”, “colonoscopy-induced”, “perforation” and “complication”. All references were searched and cross-checked. All foreign language articles if available were translated by medical personnel with proficiency in both foreign language and English. Ethics approval was not required from the institution’s ethics committee for this study.
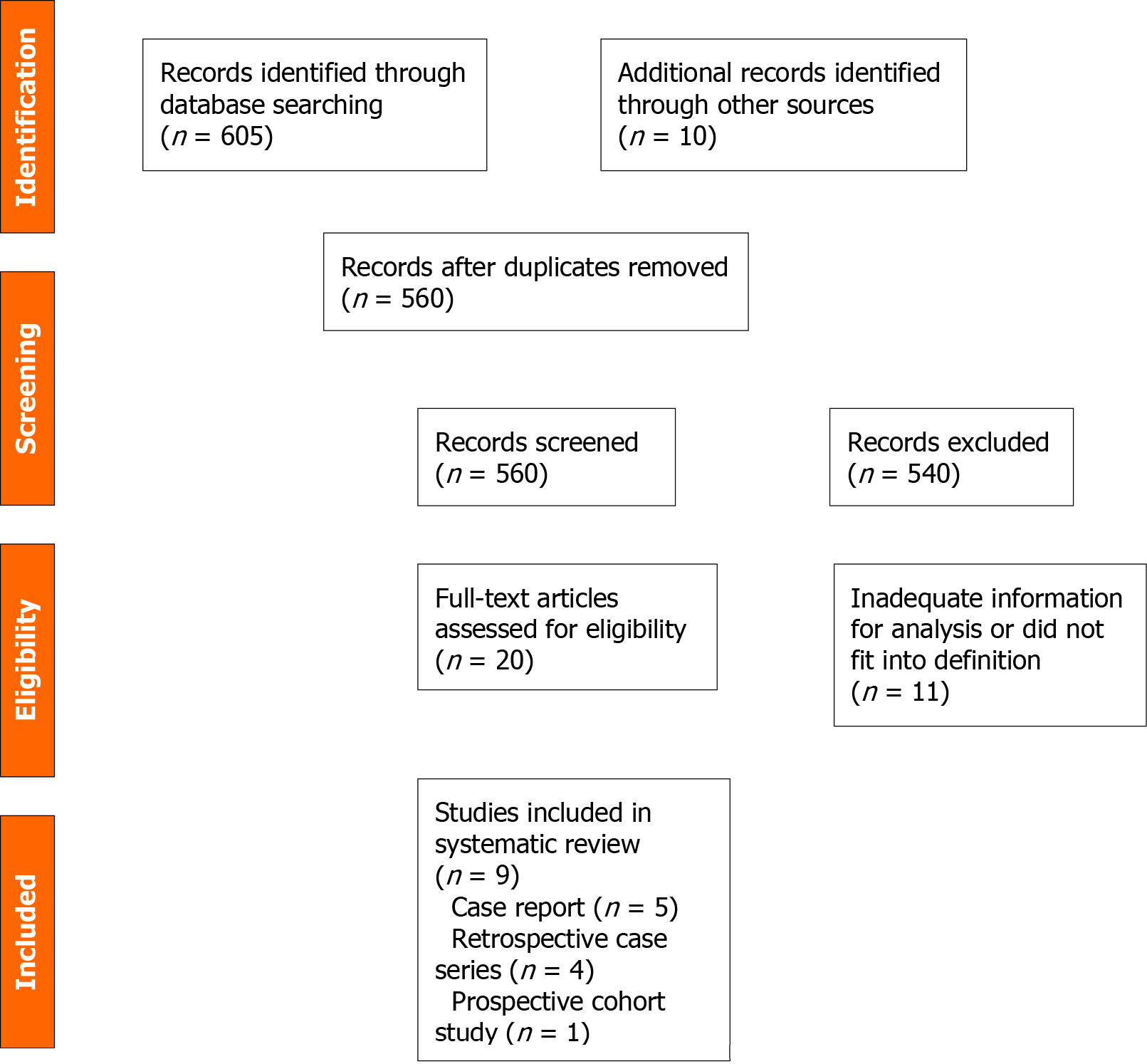
The search pathway is described as per the PRISMA flowchart as shown in Figure 1.
A data proforma was designed prior to the collection of data for uniformity. The investigators (Ng ZQ, Tan JH and Tan HCL) individually collected the data. Any difference in opinion was resolved through discussion with the other author (Theophilus M) but was not required. The data collected included author, journal, year, country, demographics, reason for colonoscopy, time to diagnosis, diagnosis method (clinical or radiological), management (outpatient or inpatient, oral or intravenous antibiotics and radiological or surgical intervention) and recurrence of diverticulitis. Data were analyzed using descriptive statistics.
One prospective study[6], four retrospective cohort studies[7-10] and four case reports[11-14] were included in the final analysis, with a total of 339 cases reported in the literature.
The estimated incidence of post-colonoscopy diverticulitis from the four retrospective and one prospective study in this review was 1.3%.
Of the nine studies, only one was published before 2010[8]. Majority of the literature originated from the United States (n = 5)[6-8,10,11]. The rest were from Asia Pacific (n = 4)[9,12-14].
None of the studies have a definition for the entity of post-colonoscopy diverticulitis. Two large studies considered the episode of diverticulitis induced by colonoscopy up to 30 d post-procedure. The other case reports considered it from 2 h to 16 d post-colonoscopy. Two studies did not specify the timeframe.
Demographics, clinical presentation and management (Table 1)
| Ref. | Type of study | Number of patient (s) | Age | Gender | Type of colonoscopy | Incomplete (I) vs Complete (C) | Reason for colonoscopy | Other concurrent intervention | Diagnosis of Post-colonoscopy diverticulitis | Findings on CT | Duration to diagnosis after scope | Symptoms | Biochemistry | Management |
| Levin et al[8]/United States/2006 | Retrospective | 6/16318 | - | - | C | - | Screening or surveillance | Biopsy (n = 5) | - | - | Within 30 d | - | - | Inpatient antibiotics (n = 4), surgery (n = 2) |
| Ko et al[1]/ United States/2010 | Prospective | 23/21375 | - | - | C | - | Screening and surveillance | - | Self-reported | - | Within 30 d | - | - | - |
| Rutter et al[10]/ United States /2012 | Retrospective | 82/43456 | - | - | C | - | Screening and surveillance | Polypectomy (n = 41) | - | - | - | - | - | - |
| Park et al[13]/Korea/2013 | Case report | 1 | 44 | M | C | C | Surveillance | Polypectomy and EMR | CT scan | Uncomplicated diverticulitis | 2 h | Abdominal pain and fever | Normal WCC | Inpatient intravenous antibiotics |
| Lin et al[9]/Taiwan/2017 | Retrospective | 156/112543 | - | - | C and F | - | Diagnostics and interventional | Biopsy (n = 6) | - | - | - | - | - | - |
| Park et al[14]/Korea/2016 | Case report | 1 | 65 | M | C | C | Surveillance | Polypectomy | CT scan | Uncomplicated diverticulitis | 48 h | Epigastric and left upper quadrant pain | Elevated WCC and CRP | Inpatient intravenous antibiotics |
| Gorgun et al[7]/ United States/2018 | Retrospective | 68/236377 | 56 (mean) | M:F = 25:43 | C | I:C = 13:55 | - | Polypectomy (n = 26) | CT scan | Uncomplicated (n = 62); Complicated diverticulitis (n = 6) | 12 ± 8 d | Abdominal pain (n = 26), nausea/vomiting (n = 12), fever (n = 5), diarrhea (n = 5), chills (n = 3), PR bleeding (n = 2) | Elevated WCC | Antibiotics (n = 60), emergency surgery (n = 6), percutaneous drainage (n = 2) |
| Hudson et al[12]/Australia/2019 | Case report | 1 | 50 | M | C | C | Diagnostics | Polypectomy | CT scan | Uncomplicated diverticulitis | 16 d | PR bleeding, generalized abdominal pain | Elevated CRP | Inpatient intravenous antibiotics |
| Mohan et al[11]/ United States/2019 | Case report | 1 | 59 | F | C | C | Screening | Polypectomy | CT scan | Uncomplicated diverticulitis | 48 h | Left lower quadrant abdominal pain | Elevated WCC | Outpatient oral antibiotics |
The larger studies did not report the mean or median age and gender distribution of the patients with post-colonoscopy diverticulitis. Only the individual cases reported them.
Only four case reports described the individual case presentations that were not completely typical of the usual presentations[11-14]. There was evidence of raised inflammatory markers (white cell count and c-reactive protein).
Six out of nine studies reported the method of diagnosis[6,7,11-14]. Of those reported, 60 patients were diagnosed with computed tomography (CT) scan and 12 based on clinical judgement. Another reported relied on self-reported symptoms and perceived diagnosis of diverticulitis[6]. The findings of CT scan were reported in six studies where 66 patients were classified as uncomplicated and 6 as complicated diverticulitis.
Six out of nine studies described the management of the patients[7,8,11-14]. Of the six studies, only one patient was managed with outpatient oral antibiotics. Two patients needed percutaneous drainage. Surgical management was required in eight patients on the index presentation, but the type of operation was not specified. In a study of 68 cases, six cases subsequently had surgery after non-operative management[7].
Only one study[7] reported the follow-up of patients in recurrence of diverticulitis (26%).
Colonoscopy is a common procedure undertaken and has a relatively safe profile[15]. The common complications post-colonoscopy include bleeding, perforation and post-polypectomy syndrome[2,6,8,16]. Rarer complications reported include splenic injury, pancreatitis, mesenteric ischemia, cholecystitis and small bowel perforation[3]. This systematic review found that the entity of post-colonoscopy diverticulitis is a relatively rare complication with incidence slightly higher than previously estimated 0.11%-0.37%[6-10]. Nonetheless, the true incidence may be clouded due to under-recognition or misdiagnosis, and spontaneous resolution without invasive intervention. This is evident in large studies that this entity was not included in the main study objective[15].
The entity of post-colonoscopy appendicitis is likely to share some similarities in its pathogenesis[17]. Various theories have been postulated for its mechanism: Barotrauma secondary to insufflation, inadvertent intubation of the diverticulum, faecolith introduction or propagation during the procedure leading to inflammation and exacerbation of subclinical/chronic disease. In patients with history of diverticulitis, navigating the colonoscopy through the diseased segment of colon can be challenging and potentially lead to inadvertent intubation of the diverticulum[3]. The choice of gas insufflation (air vs carbon dioxide) is not known to be a risk. The pre-procedure mechanical bowel preparation has a potential role in altering the gut microbiome resulting in subtle defects in the mucosal barrier and subsequently leading to an inflammatory cascade following colonoscopy[4].
This entity is envisaged to be increasingly recognised due to the following reasons. The number of screening colonoscopies is expected to increase due to the colorectal screening programme for prevention of colorectal cancer where the screening population age coincides with the increased incidence of diverticular disease (> 50% of Americans older than 60 years of age have diverticular disease[4]). Besides, although the current evidence for follow-up colonoscopy after index episode of diverticulitis is contentious but most centres still do it as a routine 6-8 wk post-diverticulitis to ensure no underlying malignancy has been missed[18,19]. Taking into consideration the lifetime risk of diverticulitis in a person is approximately 10%-25%[20], a substantial number of the population will likely undergo a colonoscopic follow-up.
The clinical presentation of post-colonoscopy diverticulitis reported from the review was considerably variable with symptoms such as generalized abdominal bleeding, per rectal bleeding, nausea/vomiting and chills. The symptoms may be interpreted as non-specific and could overlap with other entities such as post-polypectomy syndrome. However, the main concern remains iatrogenic perforation especially in patients who had interventional procedures such as polypectomy, endoscopic mucosal resection or endoscopic submucosal dissection concurrently. The initial management should include a rapid assessment with resuscitation as required. Biochemistry examination maybe unremarkable initially but leucocytosis and a raised C-reactive protein maybe observed. The mainstay of imaging is CT scan of the abdomen/pelvis to exclude colonoscopic perforation or intra-abdominal organ injuries. It will help to confirm the diagnosis and guide further management.
The principles of management are no different to the usual presentation of diverticulitis[4,19]. In patients with uncomplicated diverticulitis, a short inpatient stay with intravenous antibiotics and bowel rest are usually sufficient. Depending on regional practice, in those that are clinically well, they could potentially be managed as outpatient with or without oral antibiotics[19,21]. The use of antibiotics can even be considered omitted in uncomplicated diverticulitis with no increased risk of complications[19,22]. In patients with localized complicated diverticulitis, non-operative management should be trialed upfront[19,23,24]. If there is evidence of large abscess > 4 cm, percutaneous drainage can be organised if accessible. In the clinically unstable patient, urgent surgical intervention should be undertaken.
This systematic review has been limited by the relatively small number of patients reported to have post-colonoscopy diverticulitis with variable duration reported after the colonoscopy. The entity remains unclear as: (1) It could represent an episode of de novo acute diverticulitis rather than a sequelae in those that reported up to 30 days post-colonoscopy[6,8,12]; (2) It could also be an exacerbation of subclinical diverticulitis especially in those that underwent a colonoscopy 6-8 wk after an attack[4] and the information of history of diverticulosis or diverticulitis was lacking in the studies; (3) The symptoms can be easily overlooked and misdiagnosed if based on clinical grounds without confirmatory CT findings where some symptoms are commonly reported such as abdominal pain (10.5%), bloating (25%), diarrhea (6.3%), nausea (4%)[1] and lastly; and (4) A few studies correlated this entity based on ICD coding of diverticulitis from the database which may not be accurate[9]. This was also evident on a blog discussion post on New England Journal of Medicine Journal Watch in 2011[25].
Based on this systematic review, we propose the definition of post-colonoscopy diverticulitis as the occurrence of diverticulitis confirmed on CT scan within 72 h post-colonoscopy without the colonoscopic findings of acute or chronic diverticulitis and other pathology. The timeframe was chosen based on the definition of post-colonoscopy appendicitis which is believed to share some of the similar mechanism of pathogenesis.
A few key points raised from this systematic review: (1) It should be included in future audit of complications from colonoscopy; (2) The patients should be explained of this potential complication during the consenting process; (3) Patients with known history of diverticular disease, a difficult colonoscopy should be anticipated, and other methods should be tried to navigate the colonoscope through the diseased segment to prevent accidental intubation of the diverticula; and (4) The patients that had incomplete colonoscopy due to the abovementioned reason should be warned of the possibility of this complication on discharge.
The entity of post-colonoscopy diverticulitis is a relatively rare complication. The clinical presentation can mimic other common symptoms encountered post-colonoscopy. CT scan remains the imaging of choice to diagnose and guide further management. Majority of cases resolve with non-operative management. Endoscopists should be aware of this entity given the increasing number of colonoscopies performed.
The number of colonoscopy performed worldwide is increasing steadily over the past decade for screening, diagnostics and surveillance purposes. Similarly, the incidence of diverticular disease is also increasing in the population.
The entity of post-colonoscopy diverticulitis as a complication of colonoscopy has been reported in the literature without clear description of definition, description, clinical presentation and management strategies.
The aim of this study was to systematically review all available evidence in the literature to propose a definition of post-colonoscopy diverticulitis, describe its incidence, clinical presentation, risk factors and management strategies.
The systematic review was performed by searching the PubMed, EMBASE and Cochrane databases up to June 2020 and the references were manually cross-checked for additional references.
A total of nine studies were included in the final systematic review with a total of 339 cases. The time to diagnosis post-colonoscopy ranged from 2 h to 30 d. Clinical presentation for these patients were non-specific. Diagnosis was made mainly by computed tomography scan. Most of the patients were managed non-operatively with bowel rest and intravenous antibiotics.
The entity of post-colonoscopy diverticulitis remains debatable due to the variable timeframe included following colonoscopy in the literature. Regardless of whether this is a true complication post-colonoscopy or a de novo event, early diagnosis is vital to guide appropriate treatment.
The results of this systematic review should inform future prospective studies especially registries to record this as a potential complication following colonoscopy to further understand its true incidence and risk factors.
| 1. | Ko CW, Dominitz JA. Complications of colonoscopy: magnitude and management. Gastrointest Endosc Clin N Am. 2010;20:659-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 137] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 2. | Fang GD, Brennen C, Wagener M, Swanson D, Hilf M, Zadecky L, DeVine J, Yu VL. Use of ciprofloxacin versus use of aminoglycosides for therapy of complicated urinary tract infection: prospective, randomized clinical and pharmacokinetic study. Antimicrob Agents Chemother. 1991;35:1849-1855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 327] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 3. | Meade TW, Imeson JD, Gordon D, Peart WS. The epidemiology of plasma renin. Clin Sci (Lond). 1983;64:273-280. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 91] [Cited by in RCA: 188] [Article Influence: 26.9] [Reference Citation Analysis (9)] |
| 4. | Potvin M, Finlayson MH, Hinchey EJ, Lough JO, Goresky CA. Cerebral abnormalities in hepatectomized rats with acute hepatic coma. Lab Invest. 1984;50:560-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 306] [Article Influence: 43.7] [Reference Citation Analysis (0)] |
| 5. | Guertin SR, Gordon GJ, Levinsohn MW, Rekate HL. Intracranial volume pressure response in infants and children: preliminary report of a predictive marker in metabolic coma. Crit Care Med. 1982;10:1-4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 22] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Nunn DL, Watson SP. A diacylglycerol kinase inhibitor, R59022, potentiates secretion by and aggregation of thrombin-stimulated human platelets. Biochem J. 1987;243:809-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 173] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 7. | Gorgun E, Isik O, Sapci I, Aytac E, Abbas MA, Ozuner G, Church J, Steele SR. Colonoscopy-induced acute diverticulitis: myth or reality? Surg Endosc. 2018;32:3290-3294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Levin TR, Zhao W, Conell C, Seeff LC, Manninen DL, Shapiro JA, Schulman J. Complications of colonoscopy in an integrated health care delivery system. Ann Intern Med. 2006;145:880-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 382] [Cited by in RCA: 397] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 9. | Lin JN, Wang CB, Yang CH, Lai CH, Lin HH. Risk of infection following colonoscopy and sigmoidoscopy in symptomatic patients. Endoscopy. 2017;49:754-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Rutter CM, Johnson E, Miglioretti DL, Mandelson MT, Inadomi J, Buist DS. Adverse events after screening and follow-up colonoscopy. Cancer Causes Control. 2012; 23: 289-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 11. | Mohan N, Goldstein J. Post-Colonoscopy Diverticulitis: A Rare Complication. Am J Gastroenterol. 2019;00:S916. [DOI] [Full Text] |
| 12. | Hudson D. Acute Diverticulitis Following Colonoscopy. EC Gastroenterol Dig Syst. 2019;6:971-974. |
| 13. | Park DS, Park JW, Kim SY, Hong EY, An JS, Kim SY, Baek IY, Kim JH, Park CK. A Case of Acute Colonic Diverticulitis as a Complication of Colonoscopy. Intest Res. 2013;11:146-148. [DOI] [Full Text] |
| 14. | Park SR, Bae YS, Park KI, Kim Y. Colonoscopy-Induced Acute Diverticulitis. J Korean Geriatr Soc. 2016;20:108-111. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Reumkens A, Rondagh EJ, Bakker CM, Winkens B, Masclee AA, Sanduleanu S. Post-Colonoscopy Complications: A Systematic Review, Time Trends, and Meta-Analysis of Population-Based Studies. Am J Gastroenterol. 2016;111:1092-1101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 260] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 16. | Rathgaber SW, Wick TM. Colonoscopy completion and complication rates in a community gastroenterology practice. Gastrointest Endosc. 2006;64:556-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 115] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 17. | Ng ZQ, Elsabagh A, Wijesuriya R. Post-colonoscopy appendicitis: Systematic review of current evidence. J Gastroenterol Hepatol. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Ng ZQ, Moe KS, Wijesuriya R. Routine Colonoscopy After Acute Diverticulitis: is it Warranted? Surg Laparosc Endosc Percutan Tech. 2019;29:462-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Backon J. Sexual dysfunction, erectile impotence and obstructive azoospermia in respiratory disease. Relevance of lung-mediated regulation of prostaglandins. Chest. 1983;84:508. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 155] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Tétart F, Albigot R, Conter A, Mulder E, Bouché JP. Involvement of FtsZ in coupling of nucleoid separation with septation. Mol Microbiol. 1992;6:621-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 63] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 21. | Cirocchi R, Randolph JJ, Binda GA, Gioia S, Henry BM, Tomaszewski KA, Allegritti M, Arezzo A, Marzaioli R, Ruscelli P. Is the outpatient management of acute diverticulitis safe and effective? Tech Coloproctol. 2019;23:87-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 22. | Desai M, Fathallah J, Nutalapati V, Saligram S. Antibiotics Versus No Antibiotics for Acute Uncomplicated Diverticulitis: A Systematic Review and Meta-analysis. Dis Colon Rectum. 2019;62:1005-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (1)] |
| 23. | Dharmarajan S, Hunt SR, Birnbaum EH, Fleshman JW, Mutch MG. The efficacy of nonoperative management of acute complicated diverticulitis. Dis Colon Rectum. 2011;54:663-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 142] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 24. | Gregersen R, Mortensen LQ, Burcharth J, Pommergaard HC, Rosenberg J. Treatment of patients with acute colonic diverticulitis complicated by abscess formation: A systematic review. Int J Surg. 2016;35:201-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 90] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 25. | New England Journal of Medicine Journal Watch. Can colonoscopy cause diverticulitis? Available from: https://blogs.jwatch.org/gastroenterology/index.php/can-colonoscopy-cause-diverticulitis/2011/02/14/. |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Australia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Hu B, Pietrzak A, Tomizawa M S-Editor: Gao CC L-Editor: A P-Editor: Wang LL