Published online Apr 16, 2019. doi: 10.4253/wjge.v11.i4.271
Peer-review started: February 18, 2019
First decision: February 26, 2019
Revised: March 11, 2019
Accepted: April 8, 2019
Article in press: April 9, 2019
Published online: April 16, 2019
Processing time: 59 Days and 14.7 Hours
Self-expanding metal stents are the main palliative treatment modality for unresectable esophageal cancer. Gastroesophageal reflux is a common adverse outcome after placement of esophageal stent for cancer involving the gastroesophageal junction and the gastric cardia. Anti-reflux stents with valve have been designed to prevent the acid reflux. The superiority of anti-reflux stent over standard stent in preventing gastroesophageal reflux has not been established well. This study compares the anti-reflux stent and the standard stent in terms of their efficacy to prevent acid reflux.
To compare the standard and the anti-reflux stents in terms of their efficacy, safety, and complications.
The meta-analysis included 8 randomized clinical trials (RCTs) to compare pooled outcomes of total 395 patients. Primary outcomes include improvement in reflux symptoms and dysphagia score. Secondary outcomes include complications of stent migration, occlusion, and bleeding.
A total of eight RCTs were included in the meta-analysis. Compared to the standard stent, the anti-reflux stent showed a trend towards reduction in the dysphagia score without reaching a statistical significance [Standardized mean difference (SMD): -0.33 (-0.71, 0.05); P = 0.09, I2: 37%]. There was no statistical difference in the gastrointestinal reflux (GER) scores between the two types of stents [SMD: -0.17 (-0.78, 0.45); P = 0.008, I2: 74%]. Compared to standard stent, anti-reflux stent showed no difference in the risk of stent migration [OR: 1.37 (0.66, 2.83); P = 0.40, I2: 0 %], bleeding [OR: 1.43 (0.40, 5.13); P = 0.59, I2: 0 %], and obstruction [OR: 1.66 (0.60, 4.60); P = 0.33, I2: 0 %].
Traditional self-expanding standard esophageal stent and anti-reflux stent with valve are similar in terms of outcomes and complications.
Core tip: In this meta-analysis, we studied and compared the traditional standard self-expanding metal stent and anti-reflux stent in terms of their efficacy and safety. We included 8 randomized controlled trials in our meta-analysis from 3 different databases. We expected anti-reflux stent with valves, as its name suggests, to show improvement in reflux symptom score, however, this was not observed in our study. This review study shows that there is no difference between standard stent and anti-reflux stent in terms of improving reflux symptom and dysphagia score. This study also confirms that there is no difference in terms of complications including stent migration, bleeding, and obstruction between standard stent and anti-reflux stent.
- Citation: Pandit S, Samant H, Morris J, Alexander SJ. Efficacy and safety of standard and anti-reflux self-expanding metal stent: A systematic review and meta-analysis of randomized controlled trials. World J Gastrointest Endosc 2019; 11(4): 271-280
- URL: https://www.wjgnet.com/1948-5190/full/v11/i4/271.htm
- DOI: https://dx.doi.org/10.4253/wjge.v11.i4.271
The incidence of esophageal cancer, adenocarcinoma in particular, is rising rapidly in the western countries including the United States[1]. Involvement of the esophagogastric junction (EGJ) and gastric cardia is common for esophageal adenocarcinoma[2]. In 2015, a total of 17281 new cases of esophageal cancer were reported in the United States with 15211 deaths due to cancer[3]. About 50 to 80 percent of esophageal cancer patients present with metastasis and/or locally invasive disease which is surgically unresectable[4]. Palliative chemotherapy, radiation therapy, brachytherapy, and endoscopic management are the available treatment modalities for patients with surgically unresectable cancer[5].
Dysphagia and food bolus impaction are the two most common presentations of esophageal cancer. Placing a stent across the tumor is one of the palliative options to relieve dysphagia, and to improve the quality of life. Nonetheless, placement of esophageal stent is associated with various complications such as stent migration, bleeding, perforation, and stent occlusion. Severe acid reflux is one of the most common symptomatic complaints in patients who undergo standard metal stent placement at tumors involving EGJ or cardia, as the lower esophageal sphincter remains wide open after stent placement[6]. Recently, a study by Włodarczyk et al[7] showed that among patients who undergo esophageal stent placement for dysphagia from unresectable esophageal cancer, 45 percent complain of severe acid reflux. To reduce these post stent placement sequels, various modification of traditional standard stent (SS) are in progress, one of them is the development of anti-reflux esophageal stent (ARS).
Many randomized and prospective studies have been reported in literature comparing the efficacy and safety of SS and ARS. Intuitively, ARS with valve is supposed to decrease the gastroesophageal reflux (GER), but multiple studies have shown mixed results. We performed a systematic review and meta-analysis of these studies to ascertain the efficacy and safety of SS and ARS.
We conducted this systematic review and meta-analysis according to the guidelines provided by the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0[8] and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis statement was adopted in the preparation of this manuscript.
All randomized controlled trials (RCTs) including anti reflux stents were identified. A literature search of PubMed, CINAHL, and Cochrane Library for RCTs was performed from inception to 2018. Search terms included self-expanding metal stent, anti-reflux esophageal stent, and RCTs. Additional articles were manually searched from bibliographies of selected articles and pertinent review articles. The title, abstracts, and full text of the articles were reviewed by two independent reviewers (S.P. and H.S.). Abstracts from national and international meetings were also included.
Our inclusion criteria were: (1) RCTs; (2) Age > 18 years old; (3) Esophageal cancer with stent crossing the EGJ and cardia; (4) Comparison between SS and ARS; and (5) Reported improvement in clinical outcome and complications. Exclusion criteria were: (1) Foreign language without English version; (2) Study that included stents for benign esophageal stricture; (3) Stents placed by radiologists; and (4) Prior history of stent placement.
If multiple publications for the same study population were identified, the most recent publication was used. All disagreements were resolved by joint decision between the two authors (S.P. and H.S.), and a senior author (J.M.).
Two authors (S.P. and H.S.) independently extracted data from each study including characteristics of study, characteristics of study population, and results of study. Characteristics of study included first author, year, study design, country, type of stents used, number of patients in each arm, preemptive dilation of stents, and types of procedural sedation. Characteristics of study population included mean age, gender, indications for stent placement, and types of histopathology. Results of study included standard mean difference for GER symptoms, and dysphagia score. Odds ratio (OR) was calculated for comparison of complications which included risk of bleeding, stent migration, and stent occlusion.
Quality assessment was independently performed according to QUADAS-2 by 2 authors (S.P. and H.S.)[9]. The discrepancies between the two authors were resolved by joint decision between the two authors and the senior author (J.M.).
Randomized effects model was used to perform meta-analysis according to the heterogeneity. Pooled estimate of major outcomes studied were the improvement in dysphagia, GER scores, which were reported as standardized mean difference (SMD) with 95%CI. The risk of stent migration, bleeding, and obstruction were reported as OR with 95%CI.
Revman review manager version 5.3 was used for data analysis. Results were considered significant if P < 0.05.
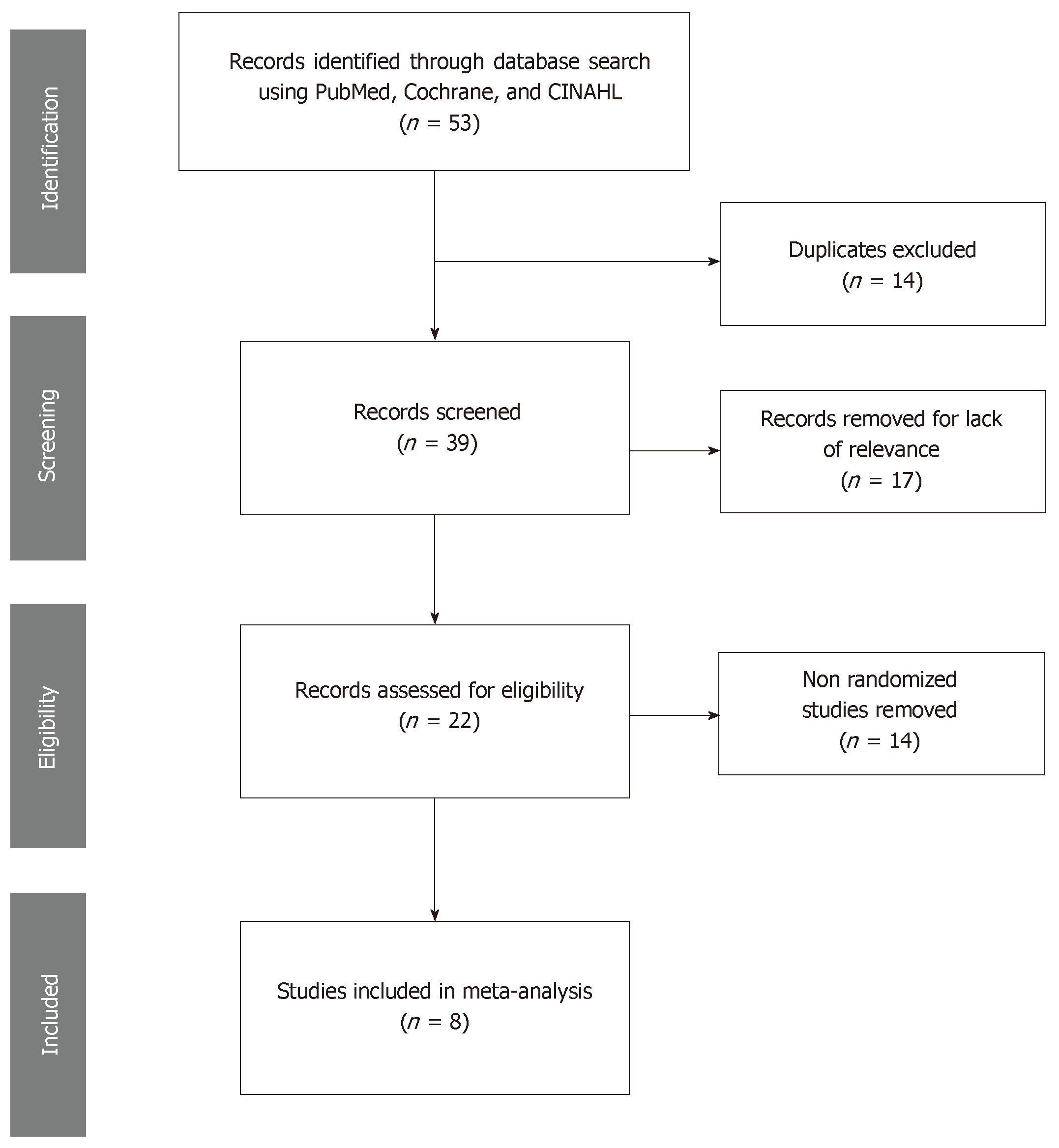
After initial search using key words (esophageal stent, anti-reflux esophageal stent, self-expanding metal stent) fifty-three potential studies were identified. After excluding duplicate studies, twenty-two studies were screened for title and abstracts. After excluding non-RCTs, only eight studies were included for detailed review for this meta-analysis[6,10-16] (Figure 1).
A total of 395 patients were included in the study, ARS (192 patients) and SS (203 patients), comparing their efficacy and outcome (Table 1). Among them 249 were men with mean age of 70.1 years. The studies were published between 2004 and 2016, and all the studies were conducted in the developed countries in the resource rich settings. Out of the eight studies, three studies were multicenter and five were single center studies. The indication for stent was dysphagia secondary to distal esophageal cancer and gastric cardia cancer. Histologically, 189 patients had adenocarcinoma of esophagus, 90 patients had squamous cell carcinoma of esophagus, and 14 had undifferentiated type (Table 2).
| Anti-reflux stent | Standard stent | |
| Patients, total (n) | 192 | 203 |
| Female (n) | 47 | 49 |
| Male (n) | 118 | 131 |
| mean age (yr) | 70 | 70.24 |
| Histology (n) | SCC = 39; Adenocarcinoma = 76; Undifferentiated = 1 | SCC = 51; Adenocarcinoma = 113; Undifferentiated = 13 |
| Study | Country | Design | Brand of stents | n (ARS, SS) | Age (ARS, SS) | Male / Female; ARS / SS | Pre-Dysphagia score (ARS / SS) | Follow-up (mo) | Use of PPI (ARS / SS) | Preemptive dilation of stent (ARS/ SS) |
| Coron et al[10], 2016 | France | RCT, multicenter | Dostent | 20 | 68.9 | 16/4 | 2.75 (0-4) | 6 | NO | YES |
| Choostent | 18 | 74 | 15/3 | 2.65 (0-4) | 6 | YES | YES | |||
| Kaduthodil et al[11], 2011 | United Kingdom | RCT, single center | NR | 27 | NR | NR | NR | NR | NR | NR |
| NR | 23 | NR | NR | NR | NR | |||||
| Blomberg et al[12], 2010 | Sweden | RCT, multicenter | Z stent- Dua- valve | 28 | 74 | 21/7 | 62 (0-100) | 3 | NR | YES |
| Z-stent | 37 | 74 | 23/14 | 61 (0-100) | 3 | NR | YES | |||
| Sabharwal et al[13], 2008 | United Kingdom | RCT, single center | FerX- Ella – valve / | 24 | 71.3 | 15/7 | 2.73 (0-5) | 3 | NO | NR |
| Ultraflex | 26 | 66.3 | 21/5 | 2.54 (0-5) | 3 | YES | NR | |||
| Power et al[14], 2007 | Ireland | RCT, single center | Hanaro stent- valve | 24 | 68.4 | 14/10 | NR | 2 | NR | NR |
| Ultraflex | 25 | 73.9 | 17/8 | NR | 2 | NR | NR | |||
| Wenger et al[15], 2006 | Sweden | RCT, multicenter | Z stent-Dua | 19 | 75 | 13/6 | 63 ± 28 | 6 | NR | NR |
| Z-stent | 25 | 73 | 13/9 | 56 ± 31 | 6 | NR | NR | |||
| Shim et al[16], 2005 | South Korea | RCT, single center | Dostent | 12 | 65.3 | 12/0 | 2.83 ± - 0.85 | 1 | NO | YES |
| Covered metal | 12 | 62.7 | 11/1 | 3.25 ± 0.4 | 1 | NO | YES | |||
| Homs et al[6], 2004 | the Netherland | RCT, single center | FerX-Ella –valve / | 15 | 69 | 12/3 | 3 (0-5) | 6 | NR | NR |
| Fer x -Ella | 15 | 69 | 12/3 | 3 (0-5) | NR | NR |
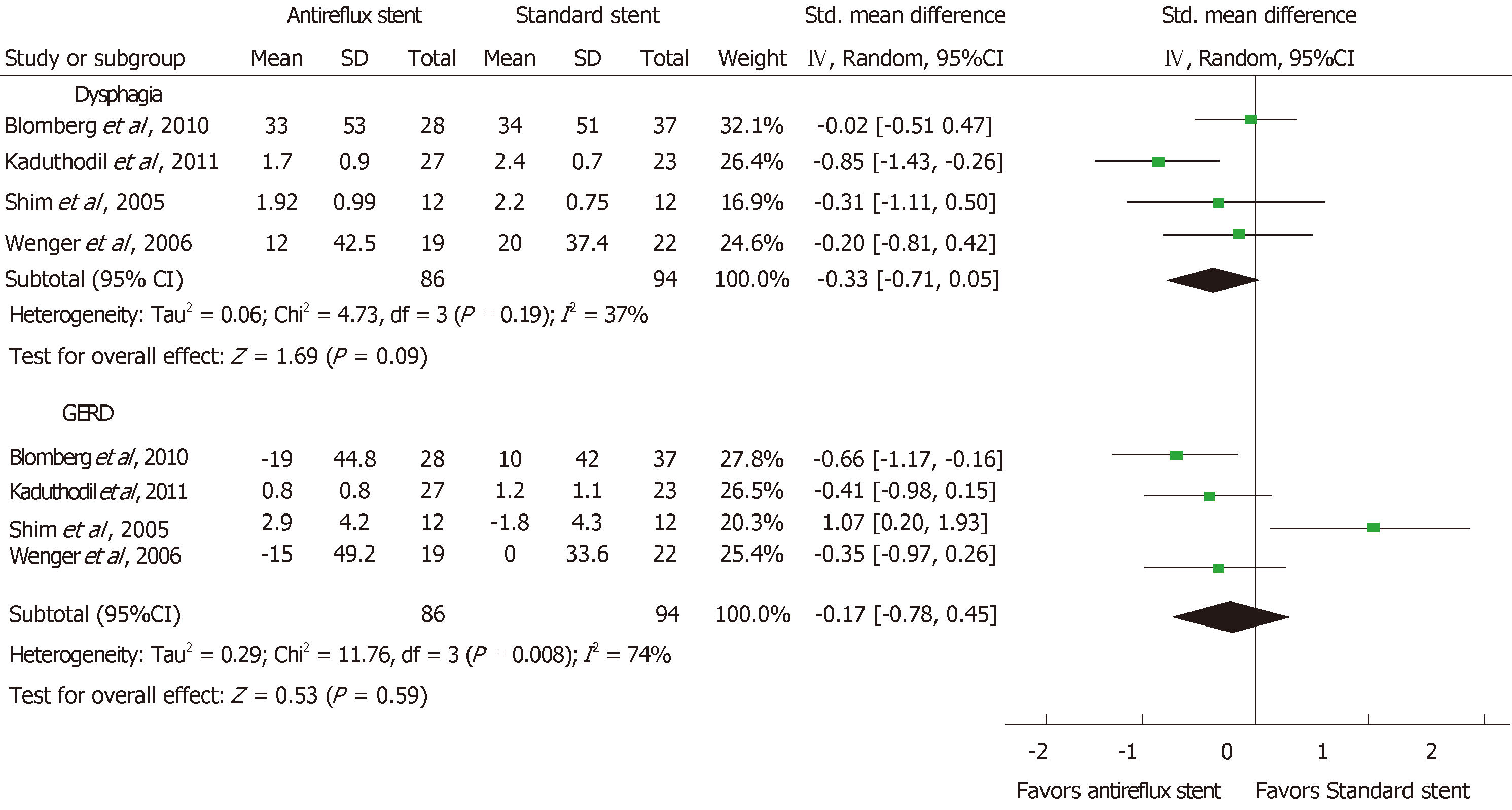
Eight studies were included in the meta-analysis, however, only four studies reported primary outcome as GER and dysphagia, before and after stent placement. Among other four studies, Coron et al[10], Sabharwal et al[13], and Homs et al[6] did not report adequate information to calculate SMD. Three studies fail to report necessary statistical information to calculate SMD, and one study provided partial statistical value that could not be used in the study[14]. Compared to the SS, the ARS showed a trend towards reduction in the dysphagia score but it did not reach a statistical significance [SMD: -0.33 (-0.71, 0.05); P = 0.09, I2: 37%]. And, there was no statistical difference in the GER scores between the two types of stents [SMD: -0.17 (-0.78, 0.45); P = 0.008, I2: 74%] (Figure 2).
Secondary outcomes
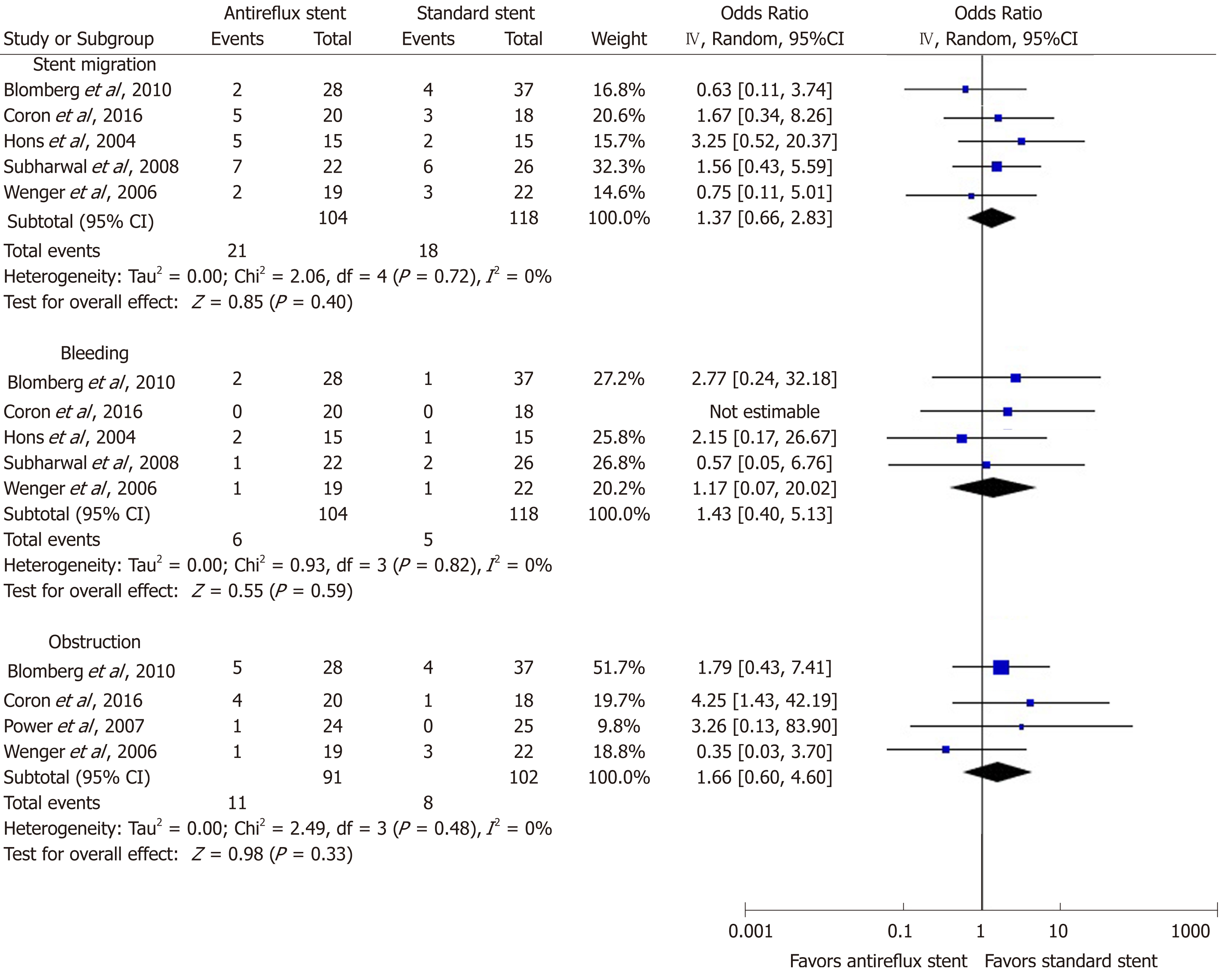
Five studies reported data on stent migration and bleeding related to stent insertion (Figure 3). Out of five studies which reported stent migration, three studies showed stent migration is more likely with SS. However, pooled results showed there was no significant statistical difference between SS and ARS in terms of risk of stent migration (OR = 1.37, 95%CI: 0.66-2.83) (Figure 3).
Five studies reported stent related bleeding but one of them did not provide adequate statistical data to calculate OR. Pooled results from four studies showed no statistical difference in bleeding risk using either SS or ARS (OR = 1.43, 95%CI: 0.40-5.13) (Figure 2).
Four studies reported data on stent occlusion. SS had more cases of stent occlusion; however, pooled data suggested no statistical difference between SS and ARS (OR = 1.66, 95%CI: 0.60-4.60) (Figure 3).
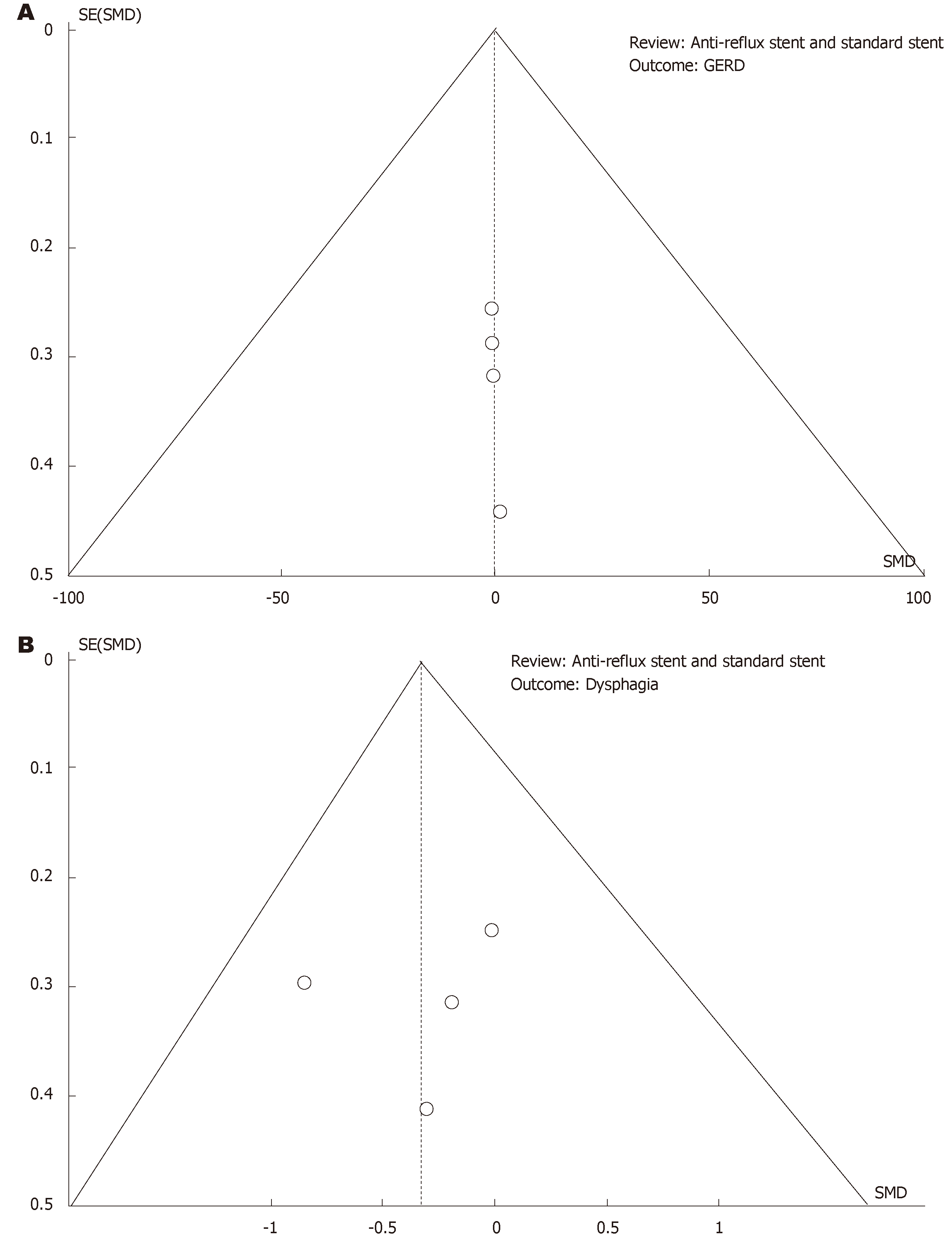
Quality assessment of each study according to the guideline by QUADAS-2 is shown in supplementary Figure 1. Concern for biases regarding patient selection, randomization, index test, reference standard was overall low except for flow of patients through the study and timing of index tests, and reference standard. By utilizing Revman Manager funnel, plots were created for outcome gastroesophageal reflux disease (Figure 4A) and outcome dysphagia (Figure 4B). No significant publication bias was found among studies evaluated.
In this systematic meta-analysis, we compared conventional standard stent with anti-reflux stents in terms of their efficacy and safety. Both types of stents were used as palliative modality to treat dysphagia in unresectable malignant esophageal and gastroesophageal junction cancer. We showed that both types of stents were equivalent in terms of primary outcome including improving GER symptoms, and reducing dysphagia score. The results are similar to the review done by Sgourakis et al[17] in 2010. Sgourakis's study compared multiple different types of SEMS with locoregional therapy whereas our study compared SS and ARS only.
Our study showed that there was no difference between the SS and ARS considering secondary endpoints that included stent migration, bleeding related to stent placement, and occlusion of stent from tumor in growth. In a meta-analysis done by Yang et al[18] comparing bare metal esophageal stents with fully covered self-expanding metal stents, stent occlusion occurred more in bare metal stents, whereas, stent migration occurred more in the covered stents. In our study, all stents were covered stents, and there was no difference in stent migration or stent occlusion. Two previous studies have shown that stainless steel stents tend to migrate more than nitinol stents[19,20]. In our study, four studies used nitinol stent[6,13,14,16] and one study by Wenger et al[15] used combination of nitinol and stainless-steel stents. We found no difference in stent migration with regards to the stent material used. Although more studies showed increased risk of bleeding, stent occlusion, and stent migration with SS; pooled data did not reach statistical significance[6,10,12,13,15].
We anticipated anti-reflux stent to have favorable outcome in improving GER symptom, as it is marketed now, but this was not seen in this study. Even though a favorable trend was seen towards ARS[11,12,15] in improving gastroesophageal reflux and dysphagia score, pooled statistical analysis did not show significant difference between those two stents. Three out of four studies that were included to calculate SMD for improvement of GER symptoms favored ARS, which could be attributed to the variation in the length of stents. Improvement in GER symptoms was seen with 140 mm stent compared to 70 mm stent[11,12,15]. A study by Coron et al[10] showed improvement in GER symptoms in ARS group, which included 20 patients, when proton pump inhibitors was used after the stent placement, however due to lack of sufficient data, this study was not included in the primary outcome.
Treatment related deaths are not included in this study, however, one previous network meta-analysis showed that treatment related deaths were reported more in the open stent group compared toanti-reflux stent group[21]. In this network meta-analysis, open stent and ultraflex stent omeprazole was compared with anti-reflux stent. The relative risk (RR) for treatment related deaths were higher in open stent and ultraflex plus omeprazole (RR = 3.00, 95%CI: 0.13-70.23) and (RR = 2.55, 95%CI: 0.11-59.49), respectively[21].
The major limitation of this meta-analysis is, it’s underpowered. We included studies with reproducible data and studies which explained our research question. The power could have been improved by including the foreign language studies. Additionally, not all studies provided data on each primary or secondary outcome. Therefore, all eight studies could not be included for both primary and secondary outcome. Hence, there is a need for larger randomized controlled studies. Although there was significant heterogeneity in reporting primary and secondary end points across studies, all studies passed the heterogeneity test.
In conclusion, both traditional standard open stent and anti-reflux stent with valve are comparable in terms of their efficacy and safety for the palliative treatment of obstructive esophageal and gastroesophageal junction malignancies. Authors believe both SS and ARS could be used in clinical practice as per the availability of clinical expertise, cost, and patient preference with informed decision.
Self-expanding metal stents are one of the palliative treatment modalities to relieve dysphagia and to improve quality of life in patients with unresectable esophageal cancer involving the gastroesophageal junction and gastric cardia. Although the quality of life improves after stent placement, it is severely limited by gastroesophageal reflux disease (GERD) especially when stent is placed across the gastroesophageal junction. To improve GERD, anti-reflux stents with valve have been designed and studied in many randomized controlled trials. However, the results from these studies are mixed. The main purpose of this study is to identify how effective is anti-reflux stent in improving gastroesophageal reflux and dysphagia when compared to standard stent.
Gastroesophageal reflux is one of the most common adverse outcomes after placement of esophageal stent in esophageal cancer involving the gastroesophageal junction and gastric cardia. Effective anti-reflux stents needs to be designed to overcome the problem of gastroesophageal reflux.
The main objective of this meta-analysis was to assess the efficacy of anti-reflux stents in improving GERD. During data gathering and analysis, authors realized that many randomized controlled trials which compared anti reflux stent and standard stents were under powered. So, more randomized controlled trials with larger number of patients are needed.
Literature search was done using electronic database to gather data for this meta-analysis where we analyzed the efficacy and safety of anti-reflux stent and standard stent. We collected data focusing on the indication for stents, material and type of stent used, demographics of patient, endoscopic technique, type of sedation used. Gastroesophageal reflux and dysphagia improvement score were our primary outcomes. Bleeding risk, stent migration risk, and stent occlusion were our secondary outcome.
There was no difference in terms of GERD score and dysphagia score between anti reflux stent and standard stent. The complications such as bleeding, stent migration, and stent occlusion were also similar between anti reflux and standard stent. Our study showed a favorable trend for anti-reflux stent to improve GERD score, though it was not statistically significant. We believe that further randomized controlled trials with larger number of patients might be helpful to ascertain if anti reflux stent indeed improves GERD score compared to standard stent.
Anti-reflux stent is not superior to standard stent in preventing GERD related to stent placement. The risk of adverse outcomes of bleeding related to stent, stent migration and stent occlusion was also comparable between anti reflux and standard stent. Both anti reflux stent and standard stent are similar in efficacy and safety. Either stent could be selected as a palliative treatment modality to relieve dysphagia in unresectable esophageal cancer. There is no difference between anti reflux stent and standard stent to prevent GERD due to stent placement across the gastroesophageal junction. Few randomized controlled trials at present suggest that anti reflux stent improve GERD related to stent placement across the gastroesophageal junction. The result from this meta-analysis did not show significant statistical difference between anti reflux stent and standard stent in terms of improving GERD score. Clinicians can choose either stent sto treat dysphagia related to esophageal cancer.
This meta-analysis showed that there are no difference in terms of safety and efficacy between anti reflux stent and standard stent. We should focus towards betterment of safety and efficacy of newer esophageal stents. More randomized clinical trials comparing the standard and anti-reflux stents are needed to further characterize their safety and efficacy.
| 1. | Pohl H, Sirovich B, Welch HG. Esophageal adenocarcinoma incidence: are we reaching the peak? Cancer Epidemiol Biomarkers Prev. 2010;19:1468-1470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 318] [Cited by in RCA: 313] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 2. | Buas MF, Vaughan TL. Epidemiology and risk factors for gastroesophageal junction tumors: understanding the rising incidence of this disease. Semin Radiat Oncol. 2013;23:3-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 241] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 3. | US Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on November 2017 submission data (1999-2015): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute, 2017. Available from: https://www.cdc.gov/cancer/uscs/dataviz/index.htm. |
| 4. | Dandara C, Robertson B, Dzobo K, Moodley L, Parker MI. Patient and tumour characteristics as prognostic markers for oesophageal cancer: a retrospective analysis of a cohort of patients at Groote Schuur Hospital. Eur J Cardiothorac Surg. 2016;49:629-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Feldman M, Friedman LS, Brandt LJ. Sleisenger and Fordtran's Gastrointestinal and Liver disease -Pathophysiology, Diagnosis, Management. 10th ed. United States: Elsevier 2016; 773-791. |
| 6. | Homs MY, Wahab PJ, Kuipers EJ, Steyerberg EW, Grool TA, Haringsma J, Siersema PD. Esophageal stents with antireflux valve for tumors of the distal esophagus and gastric cardia: a randomized trial. Gastrointest Endosc. 2004;60:695-702. [PubMed] |
| 7. | Włodarczyk JR, Kużdżał J. Stenting in Palliation of Unresectable Esophageal Cancer. World J Surg. 2018;42:3988-3996. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. Oxford: The Cochrane Collaboration 2011; . |
| 9. | Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2570] [Cited by in RCA: 2769] [Article Influence: 120.4] [Reference Citation Analysis (0)] |
| 10. | Coron E, David G, Lecleire S, Jacques J, Le Sidaner A, Barrioz T, Coumaros D, Volteau C, Vedrenne B, Bichard P, Boustière C, Touchefeu Y, Brégeon J, Prat F, Le Rhun M; Société Française d’Endoscopie Digestive (SFED). Antireflux versus conventional self-expanding metallic Stents (SEMS) for distal esophageal cancer: results of a multicenter randomized trial. Endosc Int Open. 2016;4:E730-E736. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Kaduthodil M, Lowe A, Thrower A, Prasad D, Punekar S, Stephenson S, Jackson C, Kay C. A randomised controlled study on the effectiveness of 'antireflux' stent versus 'standard open' for inoperable tumours of gastro oesophageal junction and in the prevention of symptomatic gastro-oesophageal reflux. Cardiovasc Intervent Radiol. 2011;34:492. |
| 12. | Blomberg J, Wenger U, Lagergren J, Arnelo U, Agustsson T, Johnsson E, Toth E, Lagergren P. Antireflux stent versus conventional stent in the palliation of distal esophageal cancer. A randomized, multicenter clinical trial. Scand J Gastroenterol. 2010;45:208-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Sabharwal T, Gulati MS, Fotiadis N, Dourado R, Botha A, Mason R, Adam A. Randomised comparison of the FerX Ella antireflux stent and the ultraflex stent: proton pump inhibitor combination for prevention of post-stent reflux in patients with esophageal carcinoma involving the esophago-gastric junction. J Gastroenterol Hepatol. 2008;23:723-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 34] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Power C, Byrne PJ, Lim K, Ravi N, Moore J, Fitzgerald T, Keeling PW, Reynolds JV. Superiority of anti-reflux stent compared with conventional stents in the palliative management of patients with cancer of the lower esophagus and esophago-gastric junction: results of a randomized clinical trial. Dis Esophagus. 2007;20:466-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Wenger U, Johnsson E, Arnelo U, Lundell L, Lagergren J. An antireflux stent versus conventional stents for palliation of distal esophageal or cardia cancer: a randomized clinical study. Surg Endosc. 2006;20:1675-1680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Shim CS, Jung IS, Cheon YK, Ryu CB, Hong SJ, Kim JO, Cho JY, Lee JS, Lee MS, Kim BS. Management of malignant stricture of the esophagogastric junction with a newly designed self-expanding metal stent with an antireflux mechanism. Endoscopy. 2005;37:335-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 72] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 17. | Sgourakis G, Gockel I, Radtke A, Dedemadi G, Goumas K, Mylona S, Lang H, Tsiamis A, Karaliotas C. The use of self-expanding stents in esophageal and gastroesophageal junction cancer palliation: a meta-analysis and meta-regression analysis of outcomes. Dig Dis Sci. 2010;55:3018-3030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Yang Z, Wu Q, Wang F, Ye X, Qi X, Fan D. A systematic review and meta-analysis of randomized trials and prospective studies comparing covered and bare self-expandable metal stents for the treatment of malignant obstruction in the digestive tract. Int J Med Sci. 2013;10:825-835. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Kullman E, Frozanpor F, Söderlund C, Linder S, Sandström P, Lindhoff-Larsson A, Toth E, Lindell G, Jonas E, Freedman J, Ljungman M, Rudberg C, Ohlin B, Zacharias R, Leijonmarck CE, Teder K, Ringman A, Persson G, Gözen M, Eriksson O. Covered versus uncovered self-expandable nitinol stents in the palliative treatment of malignant distal biliary obstruction: results from a randomized, multicenter study. Gastrointest Endosc. 2010;72:915-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 224] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 20. | Isayama H, Mukai T, Itoi T, Maetani I, Nakai Y, Kawakami H, Yasuda I, Maguchi H, Ryozawa S, Hanada K, Hasebe O, Ito K, Kawamoto H, Mochizuki H, Igarashi Y, Irisawa A, Sasaki T, Togawa O, Hara T, Kamada H, Toda N, Kogure H. Comparison of partially covered nitinol stents with partially covered stainless stents as a historical control in a multicenter study of distal malignant biliary obstruction: the WATCH study. Gastrointest Endosc. 2012;76:84-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 21. | Doosti-Irani A, Mansournia MA, Rahimi-Foroushani A, Haddad P, Holakouie-Naieni K. Complications of stent placement in patients with esophageal cancer: A systematic review and network meta-analysis. PLoS One. 2017;12:e0184784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: de Moura DTH, Richardson WS S-Editor: Wang JL L-Editor: A E-Editor: Wu YXJ