©The Author(s) 2022.
World J Gastrointest Endosc. Nov 16, 2022; 14(11): 684-693
Published online Nov 16, 2022. doi: 10.4253/wjge.v14.i11.684
Published online Nov 16, 2022. doi: 10.4253/wjge.v14.i11.684
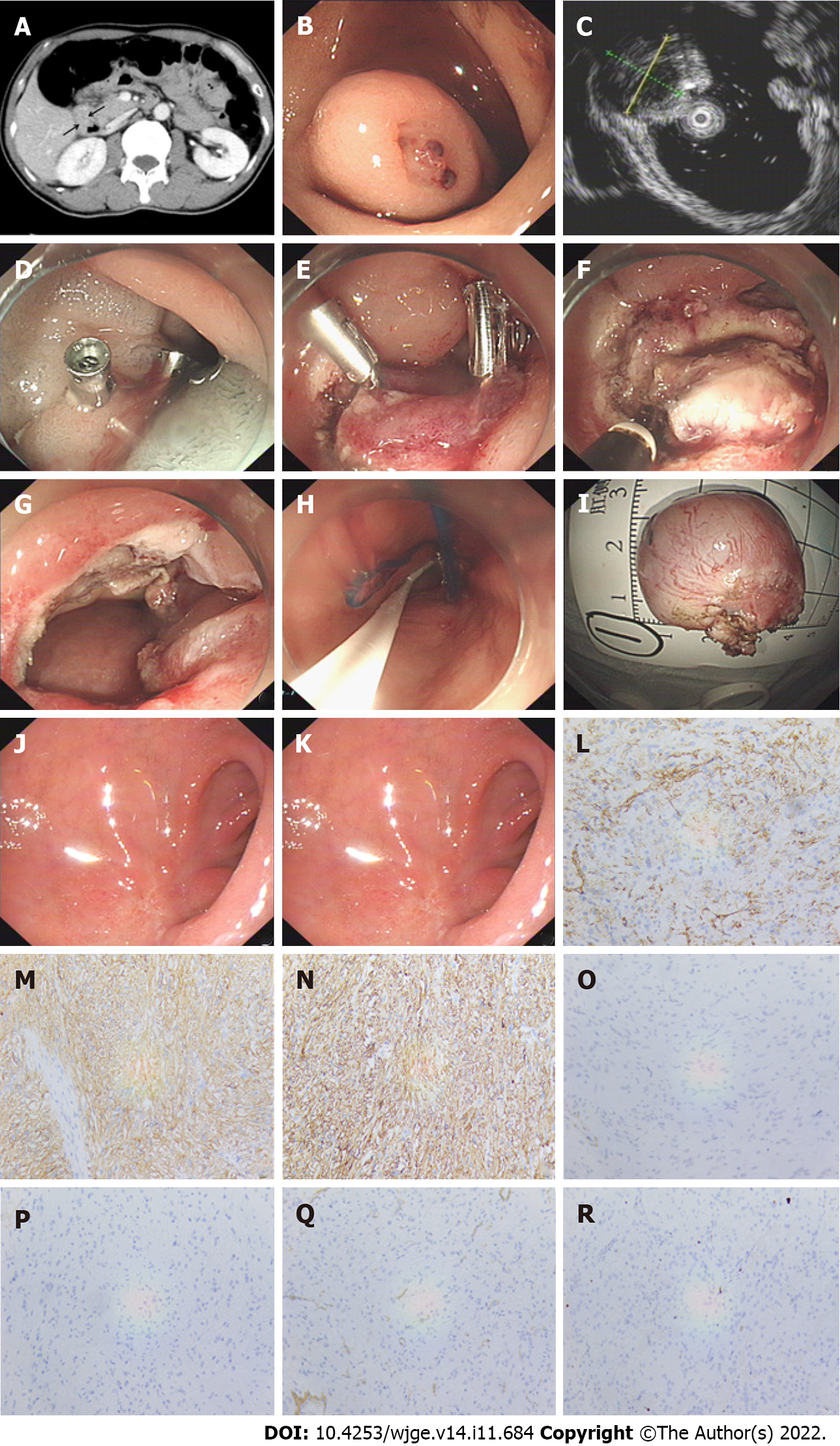
Figure 1 Endoscopic full-thickness resection for duodenal gastrointestinal stromal tumors in the descending junction of the duodenal bulb.
A: Computed tomography revealed a tumor of approximately 3 cm in diameter, with enhancement in the arterial phase; B: A tumor located in the descending junction of the duodenal bulb with ulcer and exposed blood vessels on the surface. Titanium clips were used to stop the bleeding; C: The endoscopic ultrasonography showed that the lesion was a hypoechoic structure originating from the muscularis propria layer, with uniform echo and a clear boundary; D: Submucosal injection after making several marking dots around the lesion; E: A circumferential incision was made outside the border; F: The submucosa and muscularis propria around the lesion were circumferentially dissected; G: The duodenal defect after tumor resection; H: The wound was occluded with several titanium clips + an endoloop + an over-the-scope clip. A jejunal nutrition tube was placed near the wound for drainage; I: The resected tumor with the intact capsule; J: The wound healed well at 3 mo after the procedure; K: Hematoxylin and eosin staining (original magnification × 40); L: Immunohistochemistry showed that the tumor was positive for CD34; M: Immunohistochemistry showed that the tumor was positive for CD117; N: Immunohistochemistry showed that the tumor was positive for Dog-1; O: Immunohistochemistry showed that the tumor was negative for desmin; P: Immunohistochemistry showed that the tumor was negative for S-100; Q: Immunohistochemistry showed that the tumor was negative for SMA; and R: Immunohistochemistry showed that Ki67 was about 2%.
- Citation: Wang ZZ, Yan XD, Yang HD, Mao XL, Cai Y, Fu XY, Li SW. Effectiveness and safety of endoscopic resection for duodenal gastrointestinal stromal tumors: A single center analysis. World J Gastrointest Endosc 2022; 14(11): 684-693
- URL: https://www.wjgnet.com/1948-5190/full/v14/i11/684.htm
- DOI: https://dx.doi.org/10.4253/wjge.v14.i11.684