©The Author(s) 2020.
World J Gastrointest Endosc. Aug 16, 2020; 12(8): 220-230
Published online Aug 16, 2020. doi: 10.4253/wjge.v12.i8.220
Published online Aug 16, 2020. doi: 10.4253/wjge.v12.i8.220
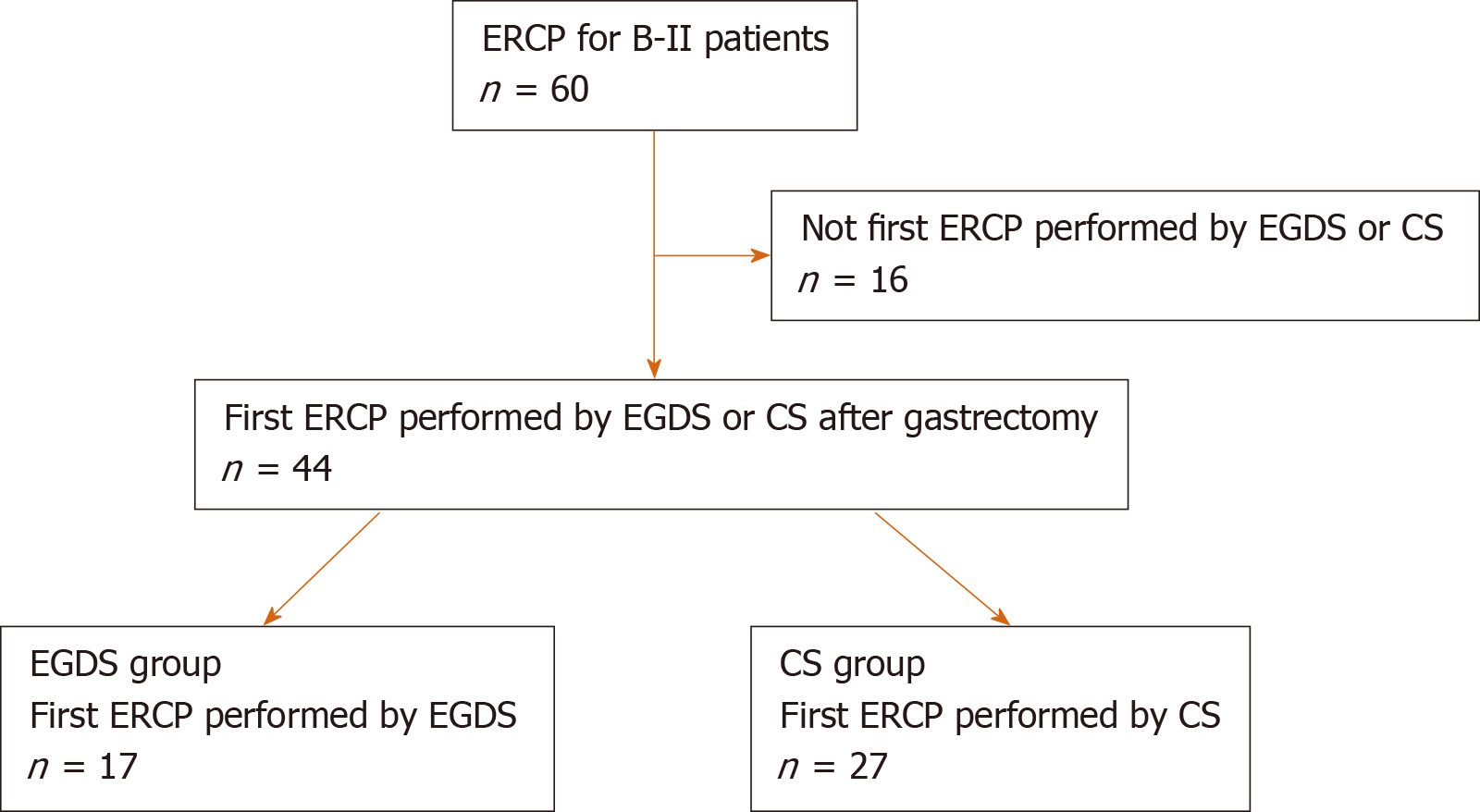
Figure 1 Target of this study.
In all, 60 cases of endoscopic retrograde cholangiopancreatography (ERCP) after Billroth II were performed. Among them, 44 cases were first procedures performed by esophagogastroduodenoscopy (EGDS) or colonoscopy (CS) after gastrectomy. Seventeen patients who underwent the first ERCP procedure by EGDS were included in the EGDS group. Twenty-seven patients who underwent the first ERCP procedure by CS were included in the CS group. ERCP: Endoscopic retrograde cholangiopancreatography; EGDS: Esophagogastroduodenoscopy; CS: Colonoscopy; B II: Billroth II.
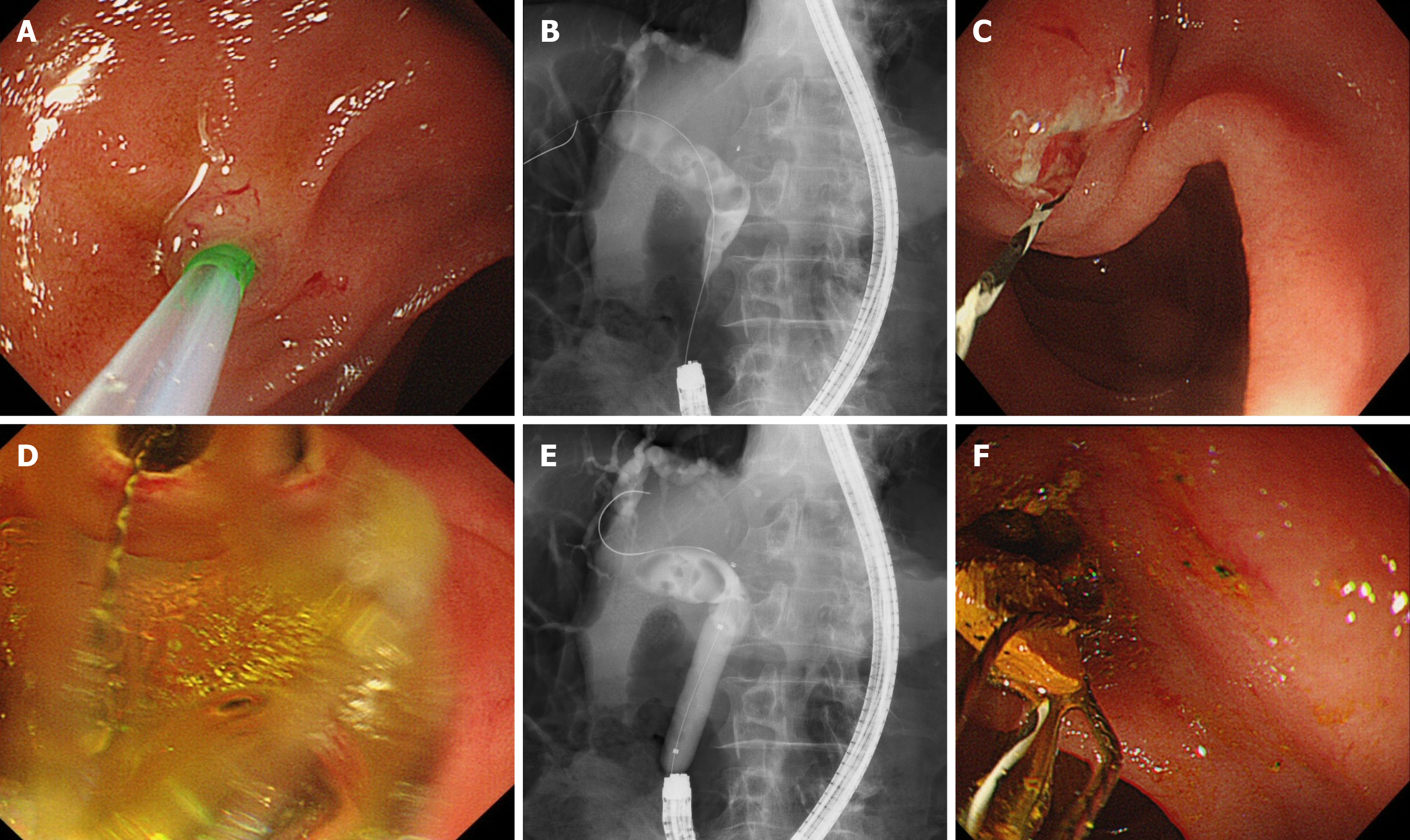
Figure 2 A case from the esophagogastroduodenoscopy group.
A: After the papilla was positioned at 11 o’clock, biliary cannulation was performed; B: Common bile duct stones were confirmed by cholangiography; C, D and E: Endoscopic sphincterotomy and endoscopic papillary large balloon dilation were performed; F: Common bile duct stones were removed.
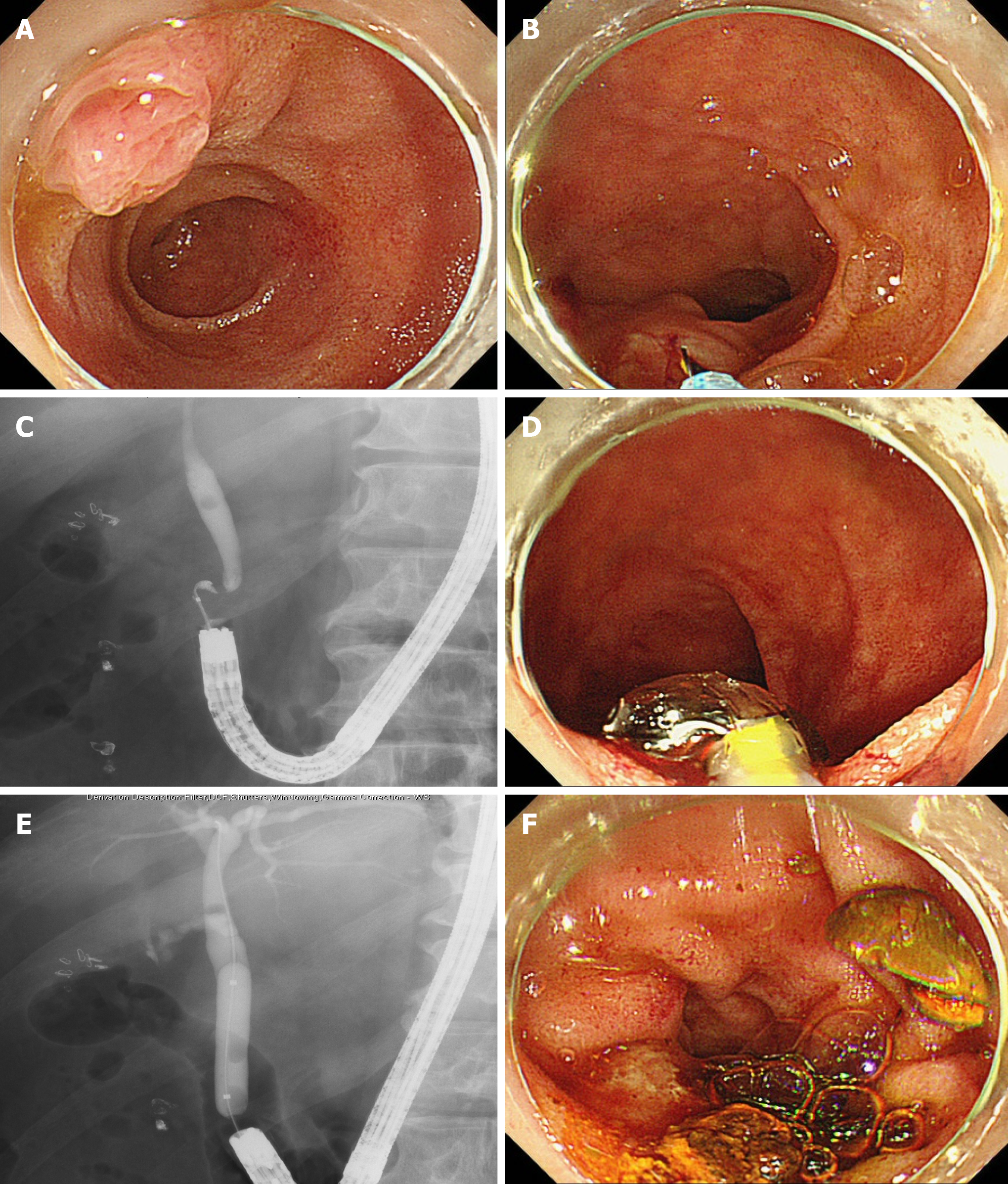
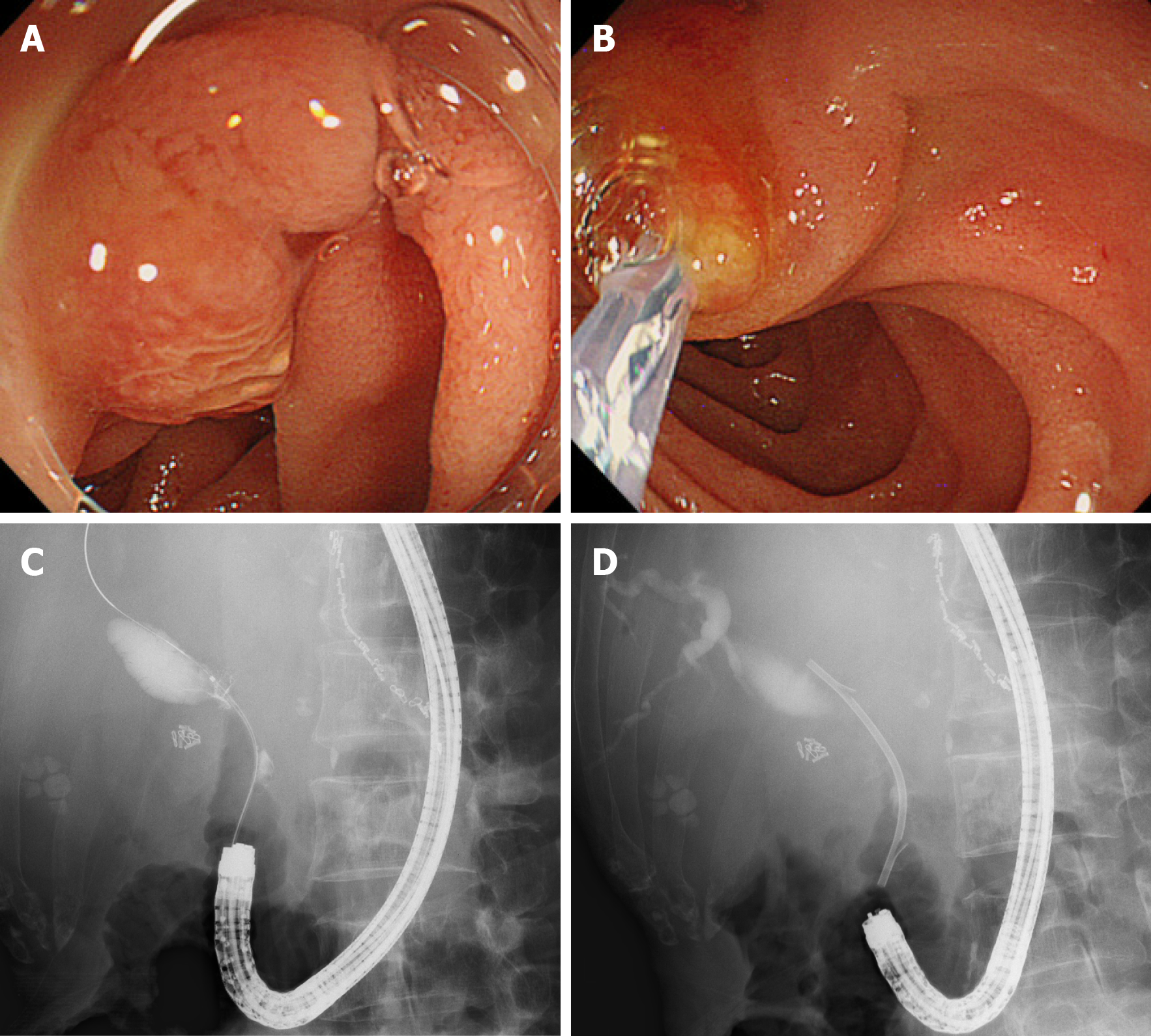
Figure 3 A case from the colonoscopy group.
A: The papilla of Vater was difficult to observe in the front; B: The papilla was positioned at 6 o’clock; C: A common bile duct stone was confirmed by cholangiography; D and E: Endoscopic papillary large balloon dilation was performed after endoscopic sphincterotomy; and F: Common bile duct stones were removed.
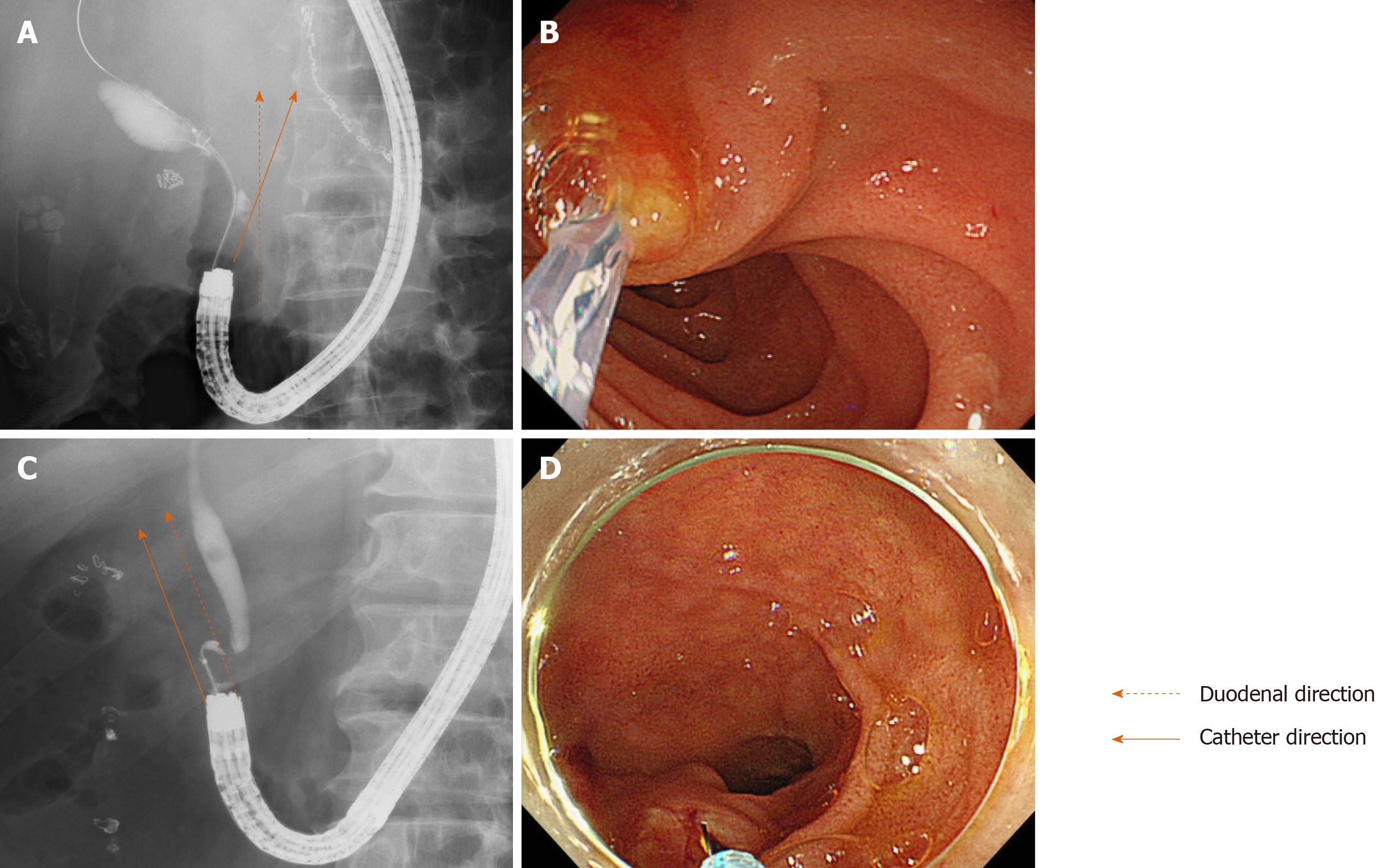
Figure 4 The duodenal and catheter directions in esophagogastroduodenoscopy and colonoscopy groups.
A and B: The duodenal direction and catheter direction crossed when endoscopic retrograde cholangiopancreatography was performed by esophagogastroduodenoscopy; C and D: The duodenal direction and catheter direction ran parallel in endoscopic retrograde cholangiopancreatography when colonoscopy was performed.
Figure 5 A case of treatment that was not successful by colonoscopy was successful by esophagogastroduodenoscopy.
A: Cannulation to the papilla of Vater was not achieved because the papilla was difficult to observe in the front by colonoscopy; B: The papilla was observed in front by esophagogastroduodenoscopy, and cannulation was achieved; C: A common bile duct stricture caused by pancreatic cancer was observed by cholangiography; and D: A biliary stent was inserted.
- Citation: Sugimoto M, Takagi T, Suzuki R, Konno N, Asama H, Sato Y, Irie H, Watanabe K, Nakamura J, Kikuchi H, Takasumi M, Hashimoto M, Kato T, Hikichi T, Ohira H. Which scope is appropriate for endoscopic retrograde cholangiopancreatography after Billroth II reconstruction: An esophagogastroduodenoscope or a colonoscope? World J Gastrointest Endosc 2020; 12(8): 220-230
- URL: https://www.wjgnet.com/1948-5190/full/v12/i8/220.htm
- DOI: https://dx.doi.org/10.4253/wjge.v12.i8.220